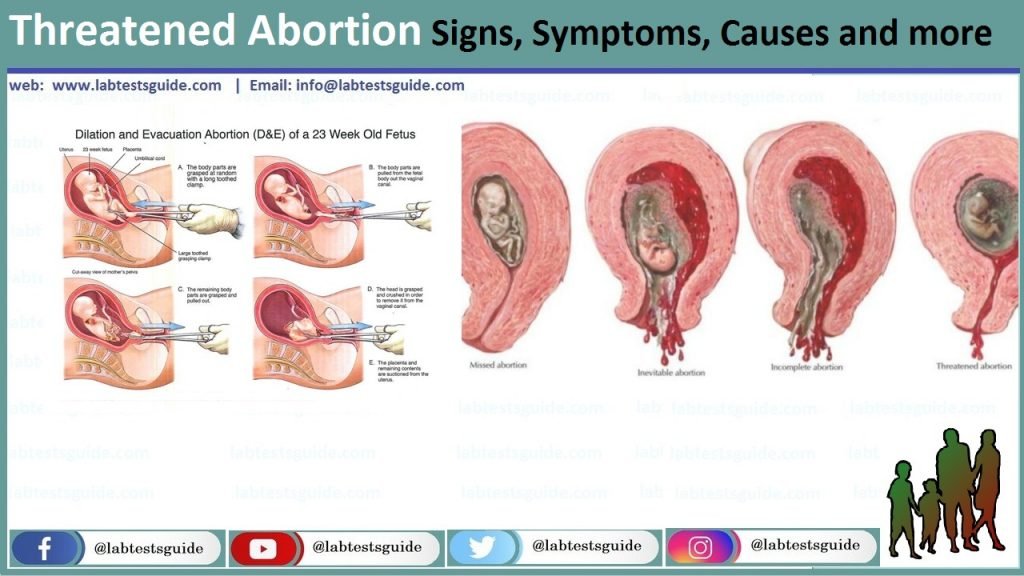
A threatened abortion occurs when a pregnant patient at less than 20 weeks gestation presents with vaginal bleeding. The cervical os is closed on a physical exam. The patient may also experience abdominal cramping, pelvic pain, pelvic pressure, and/or back pain.
Definition of Threatened Abortion.
A threatened abortion, also known as a threatened miscarriage, is a medical term used to describe a condition in which a pregnant woman experiences vaginal bleeding and/or abdominal cramping during the early stages of pregnancy (usually within the first 20 weeks). The term “threatened” is used because there is a potential risk of miscarriage, but it doesn’t necessarily mean that a miscarriage will occur.
In a threatened abortion, the pregnancy is at a stage where the embryo or fetus is still developing, and the uterus has not yet reached a point where it can support a healthy pregnancy to full term. However, it’s important to note that not all cases of vaginal bleeding during pregnancy result in a miscarriage. Many women who experience bleeding in early pregnancy go on to have healthy pregnancies.
Causes of Threatened Abortion:
Some common causes of threatened abortion include.
- Hormonal Changes: Fluctuations in hormone levels, particularly in early pregnancy, can sometimes lead to vaginal bleeding. These changes may affect the uterine lining and implantation of the embryo.
- Implantation Bleeding: In some cases, bleeding occurs when the embryo implants into the uterine lining, typically around the time when a woman would expect her menstrual period. This bleeding is usually lighter and shorter in duration than a regular period.
- Cervical Changes: Changes in the cervix, such as cervical inflammation or irritation, can lead to bleeding. Cervical irritation can result from sexual intercourse or the use of certain cervical procedures.
- Infections: Infections of the reproductive tract, such as sexually transmitted infections (STIs) or urinary tract infections (UTIs), can cause vaginal bleeding during pregnancy.
- Structural Issues: Anatomical abnormalities of the uterus or cervix, such as uterine fibroids or cervical polyps, may contribute to bleeding during pregnancy.
- Subchorionic Hematoma: Sometimes, a collection of blood may form between the chorion (the outer fetal membrane) and the uterine wall. This condition, known as subchorionic hematoma, can lead to bleeding.
- Maternal Health Conditions: Certain maternal health conditions, like thyroid disorders or uncontrolled diabetes, may increase the risk of bleeding during pregnancy.
- Medications or Supplements: Some medications or herbal supplements might increase the risk of bleeding in early pregnancy. Always inform your healthcare provider about any medications or supplements you are taking.
- Trauma or Injury: Physical trauma or injury to the abdomen, such as from a fall or accident, can cause vaginal bleeding during pregnancy.
- Unknown Causes: In some cases, the exact cause of threatened abortion remains unknown.
Signs and Symptoms:
- Vaginal Bleeding: The most common and noticeable sign of a threatened abortion is vaginal bleeding during pregnancy. This bleeding can range from light spotting to heavy bleeding. The color of the blood may vary, appearing red, pink, brown, or even slightly orange. It’s important to note that bleeding during pregnancy is never considered “normal,” and any bleeding should be reported to a healthcare provider.
- Abdominal Cramping: Many women with a threatened abortion experience abdominal cramps or lower abdominal pain. These cramps can range from mild to moderate and may feel similar to menstrual cramps. The pain may come and go.
- Backache: Some women may also experience lower back pain or discomfort along with the other symptoms.
- Pelvic Pressure: Some women report feeling a sensation of pelvic pressure, which can be associated with a threatened abortion.
- Passing Clots: In more severe cases, women may pass blood clots along with the bleeding. Passing large clots can be a cause for concern.
- Decreased Pregnancy Symptoms: Some women may notice a decrease in pregnancy symptoms such as breast tenderness or nausea, although these symptoms can vary widely from woman to woman.
Diagnosis:
The diagnostic process may include the following steps.
- Medical History: Your healthcare provider will begin by asking you about your medical history, including details about your current pregnancy and any previous pregnancies or miscarriages. Be prepared to provide information about the onset and duration of symptoms, the amount and color of vaginal bleeding, and any associated pain or discomfort.
- Physical Examination: A physical examination, including a pelvic exam, will be performed to assess the cervix and uterus. Your healthcare provider will look for any signs of cervical changes or abnormalities.
- Ultrasound: An ultrasound scan is a crucial diagnostic tool in assessing the health of the pregnancy. Transvaginal ultrasound (TVUS) is often used in early pregnancy to visualize the uterus, the gestational sac, and the developing embryo or fetus. It can help determine the location of the pregnancy within the uterus, check for a fetal heartbeat, and assess the presence of any structural issues or abnormalities.
- Blood Tests: Blood tests may be ordered to measure specific hormone levels, such as human chorionic gonadotropin (hCG), and to assess the overall health of the pregnancy. Serial hCG measurements over time can help determine the viability of the pregnancy.
- Additional Tests: Depending on the circumstances and suspected causes, additional tests may be ordered. These could include tests for infections, genetic testing, or other specialized assessments.
- Monitoring: In some cases, your healthcare provider may recommend continuous or periodic monitoring to assess the progression of symptoms and the status of the pregnancy.
Prevention and Risk Factors:
Here are some prevention tips and common risk factors to consider.
Prevention:
- Prenatal Care: Early and regular prenatal care is crucial. Attend all scheduled prenatal appointments, follow your healthcare provider’s guidance, and take any prescribed medications or supplements as directed.
- Healthy Lifestyle: Maintain a healthy lifestyle by eating a balanced diet, getting regular exercise (with your healthcare provider’s approval), and avoiding harmful substances like alcohol, tobacco, and recreational drugs.
- Stress Management: High stress levels may contribute to pregnancy complications. Practice stress-reduction techniques such as deep breathing, meditation, yoga, or counseling if needed.
- Avoid Trauma: Take precautions to avoid physical trauma or injury to the abdomen during pregnancy. Use seatbelts properly, be cautious when participating in physical activities, and take steps to prevent falls.
- Infection Prevention: Practice safe sex to reduce the risk of sexually transmitted infections (STIs) that can harm the pregnancy. Ensure that any pre-existing infections are properly treated and managed.
- Medication Awareness: Inform your healthcare provider about all medications and supplements you are taking, as some may be harmful during pregnancy. Follow their recommendations regarding medication use.
Risk Factors:
- Previous Pregnancy Loss: Women who have had previous miscarriages may be at a slightly higher risk for threatened abortion. However, many women with a history of miscarriage go on to have successful pregnancies.
- Advanced Maternal Age: Women over the age of 35 are at an increased risk for pregnancy complications, including threatened abortion.
- Chronic Health Conditions: Conditions such as diabetes, thyroid disorders, and autoimmune diseases can increase the risk of pregnancy complications, including threatened abortion. Proper management of these conditions is crucial.
- Uterine and Cervical Abnormalities: Structural issues with the uterus or cervix can increase the risk of threatened abortion. Some of these issues may be present since birth (congenital) or develop over time.
- Infections: Infections of the reproductive tract, such as STIs, can lead to complications during pregnancy.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and illicit drug use are known risk factors for pregnancy complications, including threatened abortion.
- Environmental Factors: Exposure to certain environmental toxins or workplace hazards may pose risks to pregnancy. Be aware of potential hazards and take necessary precautions.
Treatment and Management:
Here are some common approaches to treatment and management.
- Bed Rest: In some cases, healthcare providers may recommend bed rest or reduced physical activity to minimize strain and pressure on the uterus. This can help reduce the risk of further bleeding and cramping.
- Pelvic Rest: Healthcare providers often advise pelvic rest, which includes abstaining from sexual intercourse and avoiding the use of tampons. These measures help reduce the risk of infection and additional trauma to the cervix.
- Medications: Depending on the situation, your healthcare provider may prescribe medications to address specific causes or symptoms associated with a threatened abortion. Common medications include:
Progesterone supplements:
These may be used to support the pregnancy in cases of hormonal imbalances.
- Antibiotics: If an infection is suspected or confirmed, antibiotics may be prescribed.
- Pain relievers: Over-the-counter or prescription pain medications may be recommended to alleviate cramping and discomfort.
- Close Monitoring: Healthcare providers may recommend close monitoring through follow-up appointments, serial ultrasounds, and blood tests to assess the progression of the pregnancy and the status of the threatened abortion.
- IV Fluids: In cases of severe bleeding or dehydration, intravenous (IV) fluids may be administered to maintain hydration.
- Surgery: In certain situations, surgery may be necessary. This could involve removing any retained tissue from the uterus or addressing other issues contributing to the threatened abortion.
- Emotional Support: Experiencing a threatened abortion can be emotionally challenging. It’s important to seek emotional support from friends, family, or a mental health professional. Many healthcare providers also offer counseling or referrals to support groups for individuals dealing with pregnancy complications.
When to Seek Medical Help:
- Vaginal Bleeding: Any vaginal bleeding during pregnancy, regardless of the amount or color, should be taken seriously and evaluated by a healthcare provider. This includes light spotting, pink or brown discharge, or heavy bleeding.
- Abdominal Cramping: Moderate to severe abdominal cramping or lower abdominal pain, especially if it is accompanied by bleeding, should prompt you to seek medical attention.
- Back Pain: Persistent or severe lower back pain in combination with other symptoms like bleeding and cramping may indicate a potential issue with the pregnancy.
- Passing Clots: Passing blood clots, particularly large ones, during pregnancy is a concerning symptom that requires immediate medical evaluation.
- Decreased Pregnancy Symptoms: If you notice a sudden decrease in pregnancy symptoms such as breast tenderness, nausea, or fatigue, it may be a sign of a potential problem with the pregnancy.
- Fever and Chills: The presence of fever and chills along with bleeding or pain could indicate an infection, which requires immediate medical attention.
- Any Unusual or Severe Symptoms: If you experience any unusual or severe symptoms that cause you concern, it’s always best to err on the side of caution and seek medical help.
Emotional Support and Coping:
Here are some tips for emotional support and coping.
- Communicate Openly: Share your feelings, concerns, and fears with your partner, family members, or close friends. Open communication can help you feel understood and less isolated.
- Seek Professional Help: Consider talking to a mental health professional, such as a therapist or counselor, who specializes in reproductive health and pregnancy-related issues. They can provide you with coping strategies and a safe space to express your emotions.
- Support Groups: Joining a support group for individuals who have experienced pregnancy complications or miscarriages can be highly beneficial. These groups provide a sense of community and a platform to share experiences with others who understand what you’re going through.
- Educate Yourself: Learning more about threatened abortion and the potential outcomes can help alleviate some anxiety. Ask your healthcare provider for reliable resources or recommended reading materials.
- Self-Care: Prioritize self-care practices that promote relaxation and reduce stress. This can include meditation, deep breathing exercises, yoga, or simply taking time to do activities you enjoy.
- Maintain a Healthy Lifestyle: Eating well, staying hydrated, and getting regular exercise (with your healthcare provider’s approval) can contribute to your overall well-being. Avoid alcohol, smoking, and illicit drugs, as they can exacerbate stress.
- Lean on Your Healthcare Team: Don’t hesitate to ask your healthcare provider questions and seek guidance on your specific situation. They can provide medical information and reassurance.
- Journaling: Keeping a journal can be a helpful way to process your emotions and thoughts. Write down your feelings, experiences, and any questions you have. It can be therapeutic to reflect on your journey.
- Limit Stressors: Try to minimize sources of stress in your life, both at work and at home. Letting go of non-essential commitments or tasks can provide you with more time to focus on self-care and recovery.
- Lean on Your Faith or Beliefs: If you have spiritual or religious beliefs, draw upon them for support and comfort during challenging times.
- Be Patient with Yourself: Understand that grieving and coping with a threatened abortion may take time. There is no specific timeline for healing, and everyone’s experience is unique.
- Lean on Loved Ones: Let friends and family members help with practical tasks or offer emotional support. You don’t have to go through this alone.
FAQs:
What is a threatened abortion?
A threatened abortion, also known as a threatened miscarriage, is a condition in which a pregnant woman experiences vaginal bleeding and/or abdominal cramping during the early stages of pregnancy. It’s called “threatened” because it signifies a potential risk of miscarriage, but not necessarily a guarantee.
What are the common signs of a threatened abortion?
Common signs include vaginal bleeding (ranging from spotting to heavy bleeding), abdominal cramping, lower backache, and pelvic pressure.
What causes a threatened abortion?
Various factors can contribute, including hormonal changes, implantation bleeding, cervical issues, infections, structural abnormalities, and more.
When should I seek medical help if I suspect a threatened abortion?
Seek immediate medical attention if you experience vaginal bleeding during pregnancy, abdominal cramping, back pain, or any other unusual symptoms.
How is a threatened abortion diagnosed?
Diagnosis typically involves a medical history assessment, physical examination, ultrasound, blood tests, and possibly other specialized tests, depending on the situation.
What are the treatment options for a threatened abortion?
Treatment depends on the underlying cause and severity. It may include rest, pelvic rest (avoiding intercourse), medications, monitoring, surgery (in severe cases), and emotional support.
Can a threatened abortion be prevented?
Prevention may be possible in some cases by maintaining a healthy lifestyle, managing chronic health conditions, and avoiding known risk factors. However, not all cases can be prevented.
What is the prognosis for a threatened abortion?
The outcome varies depending on the cause, the stage of pregnancy, and how early medical attention is sought. Many women with threatened abortions go on to have successful pregnancies.
How can I cope emotionally with a threatened abortion?
Seek emotional support from loved ones, consider professional counseling or support groups, practice self-care, and be patient with yourself during the healing process.
Are there support groups or resources for individuals experiencing a threatened abortion?
Yes, there are support groups, online communities, and organizations that provide support and resources for individuals dealing with pregnancy complications and loss.
Conclusion:
In conclusion, a threatened abortion, marked by vaginal bleeding and abdominal cramping during early pregnancy, is a distressing and potentially serious condition that warrants immediate medical attention. While it does carry the risk of miscarriage, not all cases result in pregnancy loss, and timely diagnosis and appropriate treatment can significantly improve the chances of a positive outcome. Seeking emotional support, adhering to healthcare provider recommendations, and practicing self-care are crucial aspects of managing the physical and emotional challenges that can arise when facing a threatened abortion. Each case is unique, and compassionate care, both medical and emotional, plays a pivotal role in navigating this difficult journey.
Possible References Used