Pregnancy is a natural biological process that occurs when a female’s body becomes fertilized by a male’s sperm, leading to the development of a new human life inside the mother’s womb.

- Conception: Pregnancy begins with the fertilization of an egg by a sperm.
- Three Trimesters: Pregnancy is divided into three trimesters, each lasting about three months.
- Prenatal Care: Regular prenatal check-ups are essential for monitoring the health of both the mother and the baby.
- Early Symptoms: Common early signs of pregnancy include missed periods, nausea, and breast tenderness.
- Fetal Development: The fetus undergoes significant growth and development during pregnancy.
- Ultrasound: Ultrasound scans provide a visual of the developing fetus and can determine the baby’s sex.
- Maternal Diet: A balanced and nutritious diet is crucial for the health of the mother and baby.
- Exercise: Safe and regular exercise can benefit a pregnant woman’s overall well-being.
- Weight Gain: Healthy weight gain during pregnancy is important for fetal development.
- Morning Sickness: Nausea and vomiting, often called “morning sickness,” can occur at any time of day.
- Back Pain: Many pregnant women experience back pain due to the extra weight and changes in posture.
- Prenatal Vitamins: These supplements help ensure the mother and baby get essential nutrients.
- Labor: Labor is the process of childbirth, involving contractions and dilation of the cervix.
- Delivery Options: Mothers can choose between vaginal birth and cesarean section (C-section) delivery.
- Postpartum Period: This is the time after childbirth when the mother’s body undergoes recovery and adjustment.
- Breastfeeding: Breast milk is the recommended source of nutrition for newborns.
- Gestational Diabetes: Some women develop diabetes during pregnancy, known as gestational diabetes.
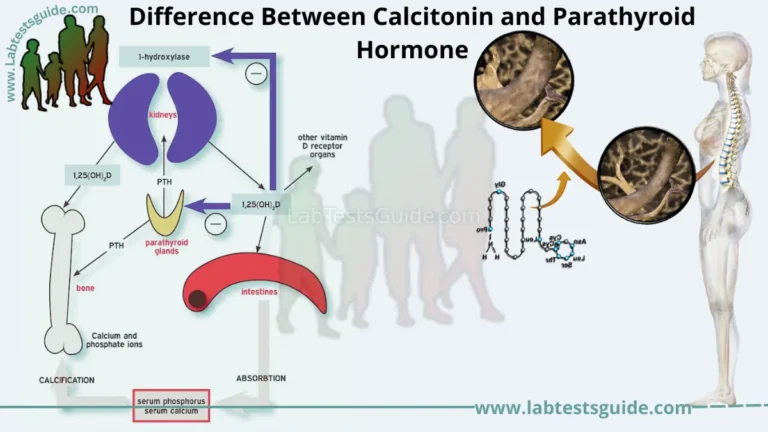
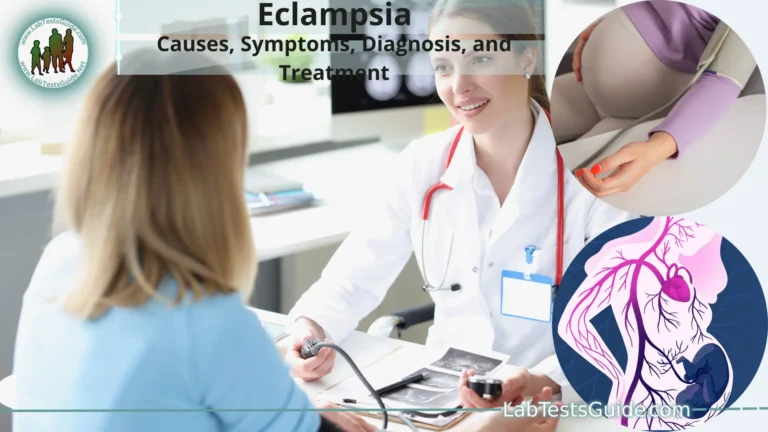
- Preeclampsia: A condition characterized by high blood pressure and organ damage during pregnancy.
- Preterm Birth: Babies born before 37 weeks of gestation are considered premature.
- Fetal Monitoring: Various tests and screenings monitor the health and development of the fetus.
- Childbirth Education: Classes can help prepare expectant parents for labor and delivery.
- Labor Pain Management: Pain relief options include epidurals, breathing techniques, and medication.
- Postpartum Depression: Some women experience mood disorders after childbirth, requiring support and treatment.
- Teen Pregnancy: Adolescent pregnancies may come with unique challenges and considerations.
- High-Risk Pregnancy: Certain medical conditions or factors may categorize a pregnancy as high-risk, requiring extra monitoring and care.
Introduction to Pregnancy:
This introduction to pregnancy covers the following key points:
- Conception: Pregnancy begins with the process of conception, where a sperm cell from a male fertilizes an egg cell from a female, forming a fertilized embryo.
- The Miracle of Life: Pregnancy is often regarded as a miraculous and awe-inspiring event, as it represents the creation of a new human being.
- Duration: On average, a full-term pregnancy lasts about 40 weeks or nine months, although it may vary slightly from person to person.
- Fetal Development: During pregnancy, the fertilized egg undergoes rapid development, eventually forming a fully developed fetus with all its major organs and body systems.
- Prenatal Care: Proper prenatal care is crucial to monitor the health of both the mother and the developing fetus. This care includes regular check-ups with healthcare providers, dietary adjustments, and lifestyle changes.
- Emotional Journey: Pregnancy is not only a physical process but also an emotional journey. Expectant parents often experience a range of emotions, from joy and excitement to anxiety and uncertainty.
- Preparing for Parenthood: Pregnancy is a time for expectant parents to prepare for the responsibilities of parenthood, including creating a safe and nurturing environment for the baby.
Early Signs and Symptoms:
- Missed Period: One of the most common early signs of pregnancy is a missed menstrual period. However, some women may experience light bleeding or spotting, known as implantation bleeding, around the time of their expected period.
- Breast Changes: Hormonal changes in early pregnancy can lead to breast tenderness, swelling, and increased sensitivity. The breasts may also darken and the areolas (the area around the nipples) may become more pronounced.
- Fatigue: Many pregnant women experience increased tiredness and fatigue, especially during the first trimester. Hormonal changes, increased blood volume, and the body’s effort to support the growing fetus can contribute to this.
- Nausea and Morning Sickness: Nausea and vomiting, often referred to as “morning sickness,” can occur at any time of the day or night. It typically begins around the sixth week of pregnancy and may last into the second trimester.
- Frequent Urination: Pregnant women often notice an increased need to urinate, even in the early weeks of pregnancy. This is due to hormonal changes and increased blood flow to the pelvic area.
- Food Aversions and Cravings: Changes in hormones can lead to changes in taste and smell preferences. Some women experience food aversions or cravings for specific foods.
- Mood Swings: Hormonal fluctuations can affect mood, leading to emotional changes such as mood swings, irritability, or heightened emotions.
- Increased Basal Body Temperature: Some women track their basal body temperature (BBT) as part of fertility monitoring. A sustained elevated BBT can indicate pregnancy.
- Sensitivity to Smells: An increased sensitivity to certain odors or a heightened sense of smell can be a sign of pregnancy.
- Bloating and Constipation: Hormonal changes can slow down the digestive system, leading to bloating and constipation.
- Tender or Swollen Gums: Pregnancy hormones can affect oral health, leading to gum tenderness and bleeding in some cases.
- Changes in Skin: Some women experience changes in skin pigmentation, such as darkening of the skin on the face, known as melasma or “the mask of pregnancy.”
- Vein Changes: Increased blood flow can cause visible changes in veins, particularly in the breasts and abdomen.
Trimesters of Pregnancy:
First Trimester (Months 1-3):
- Conception to 4 Weeks: This is the time of conception and early cell division. The fertilized egg attaches to the uterine lining, and the placenta begins to form.
- 5 to 8 Weeks: Organs and body systems start developing rapidly. The embryo becomes a fetus, and the heart begins beating. Most major organs take shape during this time.
- 9 to 12 Weeks: By the end of the first trimester, the fetus is fully formed, and all major organs are present. The fetus starts moving, but these movements are not typically felt by the mother yet. The risk of miscarriage decreases significantly after the first trimester.
Common First Trimester Symptoms:
- Morning sickness (nausea and vomiting)
- Fatigue
- Frequent urination
- Breast tenderness
- Mood swings
Second Trimester (Months 4-6):
- 13 to 16 Weeks: The second trimester is often considered the “honeymoon” phase of pregnancy. The fetus grows rapidly, and the mother may start to feel fetal movements, often referred to as “quickening.”
- 17 to 20 Weeks: The sex of the baby can often be determined during this period. The mother’s abdomen becomes more noticeable as the uterus expands. Skin changes, like the appearance of the “linea nigra” (a dark line on the abdomen), can occur.
- 21 to 24 Weeks: Fetal movements become more pronounced, and the fetus’s senses, including hearing and taste, continue to develop. The fetus’s lungs start producing surfactant, a substance essential for breathing.
Pregnancy Week By Week:
Week 1-2: Conception usually occurs during week 2. The fertilized egg, called a zygote, begins to divide and make its way down the fallopian tube toward the uterus.
Week 3: The zygote implants into the uterine lining, and the process of cell division continues. The placenta begins to form.
Week 4: The embryo is about the size of a poppy seed. The neural tube, which will become the baby’s brain and spinal cord, starts to develop. Some women may notice early signs of pregnancy, such as a missed period.
Week 5: The embryo’s heart begins to beat. Limb buds start forming, and facial features begin to develop.
Week 6: The embryo’s facial features become more distinct. Organs, such as the liver and kidneys, begin to form. Many women may start experiencing symptoms like morning sickness.
Week 7: The baby’s arms and legs are more defined. Facial features, including the eyes and nose, continue to develop.
Week 8: The embryo is now referred to as a fetus. Fingers and toes are forming, and the baby’s heartbeat is detectable with ultrasound.
Week 9: The fetus begins to move, although these movements are not typically felt by the mother yet. External genitalia start to differentiate.
Week 10: The fetus’s major organs are in place, and it is now less susceptible to birth defects caused by environmental factors. The placenta takes over hormone production.
Week 11-12: The fetus’s facial features become more refined. Fingernails and toenails develop. The mother may have her first prenatal appointment.
Week 13-14: The fetus is growing rapidly, and its limbs are moving more. Gender may be determined during this time through ultrasound.
Week 15-16: The fetus can make facial expressions, and the mother may start to feel fetal movements, commonly known as “quickening.”
Week 17-18: The baby’s bones are hardening, and the placenta is fully developed. The mother’s abdomen becomes more noticeable.
Week 19-20: The baby’s skin is covered in a protective substance called vernix. The mother may undergo an anatomy ultrasound to check the baby’s development.
Week 21-22: The fetus begins to hear sounds from the outside world. Eyelids and eyebrows are fully formed.
Week 23-24: The baby’s lungs are developing surfactant, a substance necessary for breathing. The mother may experience Braxton-Hicks contractions.
Week 25-26: The fetus’s brain continues to develop, and it may respond to external stimuli like light and sound.
Week 27-28: The baby’s eyes can open, and it starts to develop a sleep-wake cycle. The mother’s abdomen continues to expand.
Week 29-30: The baby’s bones are becoming harder, but they are still flexible. The mother may experience increased discomfort due to the size of the baby.
Week 31-32: The baby’s movements may become less vigorous as it grows and has less room to move. The mother may have more frequent contractions.
Week 33-34: The baby often moves into a head-down position in preparation for birth. The mother may experience increased pressure on her pelvis.
Week 35-36: The baby continues to gain weight rapidly. The mother may have more frequent prenatal check-ups.
Week 37-38: The baby is considered full-term, and the mother’s body prepares for labor. She may experience signs of labor, such as contractions and the loss of the mucus plug.
Week 39-40: Labor and delivery can occur at any time during these weeks. The mother may experience stronger contractions and other signs of impending labor.
Prenatal Care:
- Regular Check-ups: Schedule and attend regular prenatal check-ups with a healthcare provider throughout pregnancy.
- Healthy Diet: Maintain a balanced and nutritious diet to support the growing baby’s development.
- Prenatal Vitamins: Take prenatal vitamins containing essential nutrients, including folic acid and iron, as recommended by your healthcare provider.
- Hydration: Drink plenty of water to stay hydrated.
- Exercise: Engage in regular, low-impact exercises suitable for pregnancy to promote overall health and prepare for labor.
- Avoid Harmful Substances: Refrain from smoking, alcohol consumption, and illicit drug use.
- Medication Consultation: Discuss with your healthcare provider which medications are safe during pregnancy and which should be avoided.
- Manage Stress: Practice stress-reduction techniques and seek support when needed.
- Fetal Monitoring: Undergo recommended prenatal tests, ultrasounds, and screenings to monitor the baby’s health and development.
- Educate Yourself: Attend prenatal classes or workshops to learn about pregnancy, childbirth, and postpartum care.
- Sleep: Get adequate rest and sleep to support your energy levels and overall well-being.
- Gentle Stretching: Incorporate gentle stretching exercises to alleviate discomfort and improve flexibility.
- Dental Care: Maintain good oral hygiene, and inform your dentist about your pregnancy.
- Weight Management: Monitor weight gain to ensure it aligns with your healthcare provider’s recommendations.
- Awareness of Warning Signs: Be aware of warning signs such as bleeding, severe abdominal pain, or decreased fetal movements, and promptly report any concerns to your healthcare provider.
- Birth Plan: Consider creating a birth plan detailing your preferences and wishes for labor and delivery.
- Preparation for Labor: Take childbirth education classes and explore pain management options for labor.
- Postpartum Planning: Start thinking about postpartum care and support for after the baby’s arrival.
Labor and Delivery:
- Onset of Labor:
- Labor typically begins with contractions. These contractions cause the cervix to dilate and efface (thin out).
- Contractions can start gradually, with increasing frequency and intensity, or they may begin suddenly.
- Stages of Labor:
- First Stage: This stage is divided into early, active, and transition phases.
- Early Labor: Contractions are mild and irregular, often lasting 30-45 seconds with 5-30 minutes between them. This stage can last hours or longer.
- Active Labor: Contractions become stronger, last longer (45-60 seconds), and occur closer together (3-5 minutes apart). The cervix continues to dilate.
- Transition Phase: Contractions are intense and frequent, with little rest between them. This phase can be emotionally and physically challenging but is usually the shortest.
- Second Stage: This is the stage of pushing and birth.
- The cervix is fully dilated (10 cm), and the baby’s head moves down the birth canal.
- The mother pushes during contractions to help the baby move through the birth canal.
- The baby’s head crowns (becomes visible at the vaginal opening) before it emerges completely.
- Third Stage: This is the delivery of the placenta.
- After the baby is born, the placenta, or afterbirth, detaches from the uterine wall and is expelled through the vagina.
- Healthcare providers monitor for any signs of complications during this stage.
- First Stage: This stage is divided into early, active, and transition phases.
- Pain Management:
- Pain management options include natural techniques like breathing and relaxation exercises, as well as medical options such as epidurals or intravenous pain relief.
- Pain management choices should be discussed with the healthcare team in advance.
- Positioning:
- Finding comfortable positions during labor, such as walking, rocking, or changing positions, can help manage pain and facilitate the baby’s descent.
- Monitoring:
- Healthcare providers continuously monitor the baby’s heart rate and the mother’s contractions during labor.
- Monitoring helps identify any potential issues.
- Medical Interventions:
- Medical interventions like induced labor, assisted delivery with forceps or vacuum, and C-sections may be necessary in certain situations.
- Emotional Support:
- Emotional support from a partner, doula, or healthcare team can be invaluable during labor.
- Bonding and Care After Birth:
- After birth, the baby is often placed on the mother’s chest for skin-to-skin contact.
- Healthcare providers assess and care for the baby’s immediate needs.
- Recovery: Recovery after childbirth includes uterine contractions to expel any remaining tissue, vaginal bleeding (lochia), and physical and emotional adjustments.
- Postpartum Care: Postpartum care involves follow-up appointments, breastfeeding support, and addressing any concerns or complications that may arise after delivery.
Postpartum Period:
The postpartum period, often referred to as the postpartum or postnatal period, is the period of time following childbirth when a woman’s body undergoes physical and emotional adjustments as it transitions back to a non-pregnant state. This period is typically divided into the early postpartum period, which lasts about 6-8 weeks, and the extended postpartum period, which can last several months or longer. Here’s an overview of the postpartum period:
- Physical Recovery:
- Uterine Contractions: After childbirth, the uterus continues to contract to expel any remaining placental tissue and return to its pre-pregnancy size.
- Vaginal Bleeding: Lochia is a type of vaginal discharge that consists of blood, mucus, and uterine tissue. It is normal and can last for a few weeks.
- Perineal Healing: If there were any tears or episiotomies during delivery, the perineum (the area between the vagina and anus) may require time to heal.
- Breast Changes: The breasts may become engorged as they produce milk for breastfeeding.
- Emotional Adjustment:
- Baby Blues: Many women experience mood swings, sadness, or weepiness in the days following childbirth. This is often referred to as the “baby blues” and is usually temporary.
- Postpartum Depression (PPD): Some women may develop more serious and persistent mood disorders, such as postpartum depression or anxiety. It’s important to seek help if these feelings persist.
- Breastfeeding and Infant Care:
- The postpartum period involves establishing breastfeeding, if chosen, or adapting to infant feeding routines.
- Learning to care for and bond with the newborn is a significant aspect of this period.
- Postpartum Check-ups:
- Women typically have postpartum check-ups with their healthcare providers to ensure their physical and emotional well-being.
- Birth Control:
- Decisions regarding birth control options after childbirth should be discussed with a healthcare provider.
- Physical Activity:
- Exercise and physical activity may be gradually resumed, following guidance from healthcare providers.
- Sleep:
- Sleep patterns often change with a newborn. Adequate rest and sleep are crucial for the mother’s recovery and well-being.
- Support and Self-Care:
- Seeking support from family, friends, or support groups can be invaluable during this period.
- Self-care is essential for the mother’s physical and mental health.
- Resuming Sexual Activity:
- Decisions about when to resume sexual activity should be made in consultation with healthcare providers.
- Emotional Support:
- Partners and loved ones play a crucial role in providing emotional support during the postpartum period.
Pregnancy Complications:
Pregnancy complications are health issues or conditions that can arise during pregnancy, potentially affecting the health of the mother, the developing fetus, or both. It’s important to note that many pregnancies progress without complications, but healthcare providers closely monitor expectant mothers to identify and address any potential issues promptly. Here are some common pregnancy complications:
- Gestational Diabetes: This condition occurs when a woman’s blood sugar levels become elevated during pregnancy. It usually resolves after childbirth but requires careful management during pregnancy to prevent complications for both the mother and baby.
- Preeclampsia: Preeclampsia is a potentially serious condition characterized by high blood pressure and damage to organs like the liver and kidneys. It typically occurs in the second half of pregnancy and can lead to complications such as premature birth.
- Preterm Birth: Preterm birth is when a baby is born before 37 weeks of gestation. Premature infants may face health challenges because their organs are not fully developed.
- Multiple Pregnancies (Twins, Triplets): Carrying more than one fetus can increase the risk of complications, including preterm birth and low birth weight.
- Placenta Previa: Placenta previa is a condition in which the placenta covers part or all of the cervix. It can lead to bleeding during pregnancy and often requires a cesarean section (C-section) for delivery.
- Placental Abruption: Placental abruption occurs when the placenta separates from the uterine wall before delivery, leading to bleeding and potential complications for both the mother and baby.
- Ectopic Pregnancy: An ectopic pregnancy is when a fertilized egg implants outside the uterus, usually in the fallopian tube. It cannot result in a full-term pregnancy and can be life-threatening if not treated promptly.
- Infections: Infections during pregnancy, such as urinary tract infections, sexually transmitted infections, or intrauterine infections, can pose risks to both the mother and baby.
- Hyperemesis Gravidarum: This severe form of morning sickness involves persistent and severe nausea and vomiting, potentially leading to dehydration and weight loss.
- Rh Incompatibility: Rh incompatibility occurs when a mother and baby have different Rh blood types, potentially leading to an immune response in which the mother’s body attacks the baby’s red blood cells.
- Intrauterine Growth Restriction (IUGR): IUGR is a condition in which the baby does not grow at the expected rate in the womb, often due to placental problems.
- Cervical Insufficiency: Cervical insufficiency is when the cervix begins to open prematurely, increasing the risk of preterm birth.
- Anemia: Anemia during pregnancy can result in a low red blood cell count and may require iron supplementation.
Fetal Monitoring:
1. External Fetal Monitoring:
- External fetal monitoring involves placing sensors on the mother’s abdomen to monitor the baby’s heart rate and the frequency and duration of contractions.
- Doppler Ultrasound: A handheld Doppler ultrasound device is used to listen to the baby’s heartbeat. It provides information about the baby’s heart rate and rhythm.
- External Tocodynamometer: This device records uterine contractions by measuring the changes in the abdomen’s size during contractions.
- Electronic Fetal Heart Rate Monitoring (EFM): EFM combines Doppler ultrasound for monitoring the baby’s heart rate and the tocodynamometer for tracking contractions. EFM can provide a continuous record of the baby’s heart rate and uterine contractions during labor.
2. Internal Fetal Monitoring:
- Internal fetal monitoring involves inserting sensors directly into the baby’s scalp and the uterine wall.
- Fetal Scalp Electrode (FSE): A small electrode is attached to the baby’s scalp through the cervix to provide a more accurate and continuous measurement of the fetal heart rate.
- Intrauterine Pressure Catheter (IUPC): A thin catheter is inserted through the cervix to measure the strength and frequency of uterine contractions from within the uterus.
When is Fetal Monitoring Used?
- Fetal monitoring is commonly used during labor, especially if:
- There are risk factors or complications during pregnancy.
- The pregnancy has gone beyond the due date.
- There are concerns about the baby’s well-being.
- The mother is receiving medications or undergoing procedures that could affect the baby’s heart rate.
Interpreting Fetal Monitoring:
- Healthcare providers assess the fetal heart rate patterns and the contractions to evaluate the baby’s condition.
- Patterns that are within normal ranges are reassuring, while patterns that deviate from the norm may indicate potential issues, such as fetal distress.
- Decisions about interventions, such as changing positions, administering medication, or considering a cesarean section, are made based on the monitoring findings and clinical judgment.
Pregnancy Choices:
- Prenatal Care: Choosing a healthcare provider and scheduling regular prenatal check-ups are essential decisions. Options include obstetricians, midwives, family physicians, and nurse practitioners.
- Birth Plan: Deciding on the type of birthing experience you want is a significant choice. Consider options such as a hospital birth, home birth, birthing center, or water birth.
- Pain Management: Choose whether you want to explore natural pain management techniques, use medical pain relief options like epidurals, or a combination of both during labor.
- Genetic Testing and Screening: Decide whether you want to undergo genetic testing or screenings to assess the risk of genetic conditions or birth defects in the baby.
- Birthing Team: Consider who you want to be present during labor and delivery. This may include a partner, family members, a doula, or friends.
- Infant Feeding: Decide whether you plan to breastfeed, formula-feed, or use a combination of both, and seek support and education on your chosen method.
- Birthplace: Choose where you want to give birth. Options may include a hospital, birthing center, or home.
- Cord Blood Banking: Decide whether you want to bank your baby’s cord blood, which contains valuable stem cells.
- Circumcision: If you’re having a male baby, decide whether you want to have a circumcision.
- Vaccinations: Discuss and make decisions about vaccinations for your baby according to your healthcare provider’s recommendations.
- Postpartum Care: Plan for postpartum support, including who will assist with childcare, household chores, and emotional support after the baby arrives.
- Parenting Style: Discuss and align your parenting philosophies and styles with your partner if applicable.
- Work and Maternity Leave: Decide when to take maternity leave and how to manage work responsibilities during pregnancy and after childbirth.
- Financial Planning: Make financial decisions regarding medical expenses, insurance, and budgeting for the added costs associated with a new baby.
- Name Selection: Choose a name for your baby, considering cultural, familial, and personal preferences.
- Baby Gear and Nursery: Plan for and select baby gear, such as cribs, car seats, strollers, and nursery items.
- Childbirth Education: Consider enrolling in childbirth education classes to prepare for labor, delivery, and newborn care.
- Adoption or Alternative Paths: For individuals or couples considering adoption or alternative paths to parenthood, research and make informed choices regarding adoption agencies, surrogacy, or fertility treatments.
Preparing for Parenthood:
- Prenatal Care: Begin prenatal care early in pregnancy to monitor your health and the baby’s development. Attend all recommended check-ups and follow your healthcare provider’s advice.
- Parenting Classes: Consider enrolling in prenatal and parenting classes to gain knowledge about pregnancy, childbirth, infant care, and child development.
- Create a Birth Plan: Develop a birth plan outlining your preferences for labor, delivery, and postpartum care. Discuss it with your healthcare provider and birthing team.
- Financial Planning: Review your finances and create a budget to accommodate the costs associated with raising a child, including healthcare, childcare, diapers, clothing, and education.
- Choose a Pediatrician: Research and select a pediatrician or healthcare provider for your baby. Schedule your baby’s first check-up shortly after birth.
- Create a Support System: Build a support network of family and friends who can offer emotional support and assistance with childcare when needed.
- Parental Leave: nderstand your parental leave options and discuss them with your employer. Plan for the period when you or your partner will be away from work.
- Childproof Your Home: Babyproof your living space by securing dangerous items, installing safety gates, and covering electrical outlets.
- Stock Baby Essentials: Purchase essential baby items such as diapers, clothing, bottles, formula or breastfeeding supplies, and a safe crib or bassinet.
- Consider Childcare Options: Research childcare options, including daycare centers, in-home daycare providers, or family caregivers if you plan to return to work.
- Establish a Sleep Routine: Learn about newborn sleep patterns and consider establishing a bedtime routine that promotes healthy sleep habits.
- Plan for Feeding: If breastfeeding, educate yourself about breastfeeding techniques and support systems. If formula feeding, have formula and bottles ready.
- Mental and Emotional Preparation: Understand that parenthood can be emotionally challenging. Seek emotional support through friends, family, or therapy if needed.
- Baby Name: Choose a name for your baby, considering cultural, familial, and personal preferences.
- Time Management: Evaluate your daily schedule and adjust it to accommodate the demands of parenthood.
- Health and Well-being: Prioritize your physical and mental health. Get adequate rest, eat well, exercise, and manage stress.
- Baby-Proof Transportation: Ensure you have a safe and appropriate car seat installed correctly for transporting your baby home from the hospital.
- Legal and Financial Planning: Update or create a will, designate guardianship, and review your life insurance and estate planning.
- Embrace Flexibility: Understand that parenting doesn’t always go as planned. Be flexible and willing to adapt to the needs and quirks of your child.
- Paternity/Maternity Leave: If you or your partner are taking parental leave, understand your employer’s policies and plan for this time together.
Tests Associated With Pregnancy:
- Pregnancy Tests: A pregnancy test is usually the first step to confirm pregnancy. Home pregnancy tests detect the presence of human chorionic gonadotropin (hCG) in the urine. A blood test can also confirm pregnancy.
- Blood Tests:: Blood tests can provide valuable information about the mother’s health and the baby’s development. Common blood tests during pregnancy include:
- Complete Blood Count (CBC): Checks for anemia or other blood-related issues.
- Blood Type and Rh Factor: Determines the mother’s blood type and Rh factor, which may affect the baby.
- Blood Glucose Test: Screens for gestational diabetes.
- TORCH Panel: Tests for infections that can affect pregnancy.
- HIV and Other Sexually Transmitted Infections (STIs): Screenings to ensure the mother’s and baby’s health.
- Genetic Testing: To assess the risk of genetic conditions in the baby (e.g., Down syndrome).
- Ultrasound Exams: Ultrasound scans use sound waves to create images of the developing fetus. They are used for various purposes, including confirming the pregnancy, dating the pregnancy, and assessing the baby’s growth and anatomy.
- Non-Invasive Prenatal Testing (NIPT): NIPT is a blood test that screens for chromosomal abnormalities in the fetus, such as Down syndrome, without the risk of miscarriage associated with some invasive tests.
- Amniocentesis: Amniocentesis involves the removal of a small amount of amniotic fluid from the uterus for testing. It is usually performed in the second trimester to diagnose chromosomal abnormalities and genetic conditions.
- Chorionic Villus Sampling (CVS): CVS is a procedure in which a small sample of placental tissue is taken for genetic testing. It is typically performed in the first trimester.
- Group B Streptococcus (GBS) Screening: GBS is a bacterium that can affect newborns during childbirth. A screening test is performed during the third trimester to determine if the mother is a carrier.
- Glucose Challenge Test (GCT) and Glucose Tolerance Test (GTT): These tests are used to screen for gestational diabetes, a condition that can develop during pregnancy. If the GCT results are elevated, a follow-up GTT may be recommended.
- Cervical Length Measurement: This ultrasound measurement assesses the length of the cervix and can help predict the risk of preterm birth.
- Group Prenatal Care: – Some healthcare providers offer group prenatal care, where expectant mothers with similar due dates attend group sessions to discuss pregnancy topics, share experiences, and receive prenatal care simultaneously.
- Non-Stress Test (NST): – An NST monitors the baby’s heart rate in response to its movements to assess its well-being.
- Biophysical Profile (BPP): A BPP combines an ultrasound and NST to evaluate the baby’s health and well-being, particularly in high-risk pregnancies.
FAQs:
1. How soon can I take a pregnancy test after a missed period?
You can take a pregnancy test as early as the first day of your missed period or later. Some tests claim to detect pregnancy even a few days before your expected period, but accuracy may vary.
2. What are the early signs of pregnancy?
Early signs may include a missed period, breast tenderness, fatigue, nausea (morning sickness), frequent urination, and mood swings. However, symptoms can vary widely among individuals.
3. When should I start prenatal care?
Ideally, you should schedule your first prenatal care appointment as soon as you suspect you’re pregnant or shortly after a positive pregnancy test. Early prenatal care is important for monitoring your health and the baby’s development.
4. What should I eat during pregnancy?
A well-balanced diet is essential. Focus on foods rich in nutrients like folic acid, iron, calcium, and protein. Avoid or limit certain foods like raw seafood, unpasteurized dairy, and excessive caffeine.
5. Can I continue exercising during pregnancy?
Yes, exercise is generally beneficial during pregnancy. Consult your healthcare provider to determine a safe exercise routine based on your individual circumstances.
6. What is gestational diabetes, and how is it managed?
Gestational diabetes is a type of diabetes that develops during pregnancy. It is managed through dietary changes, regular monitoring of blood sugar levels, and, if needed, medication or insulin.
7. What is preeclampsia, and how is it treated?
Preeclampsia is a condition characterized by high blood pressure and organ damage. Treatment may involve medications, monitoring, and, in severe cases, early delivery.
8. What is the difference between a midwife and an obstetrician?
Midwives are trained to provide prenatal, childbirth, and postpartum care with a focus on natural childbirth. Obstetricians are medical doctors who specialize in pregnancy and childbirth and can handle high-risk pregnancies and surgeries.
9. When should I start preparing for labor and delivery?
It’s a good idea to start preparing for labor and delivery in the second trimester by taking prenatal classes, discussing your birth plan with your healthcare provider, and considering pain management options.
10. How can I relieve common pregnancy discomforts like morning sickness and back pain?
There are various strategies to manage discomforts, including eating small, frequent meals for morning sickness, practicing good posture and gentle exercises for back pain, and discussing over-the-counter remedies with your healthcare provider.
Conclusion:
In conclusion, pregnancy is a unique and transformative journey marked by physical, emotional, and lifestyle changes. It’s a time of anticipation, preparation, and joy as expectant parents await the arrival of their baby. Throughout pregnancy, prenatal care plays a crucial role in ensuring the health and well-being of both the mother and the developing fetus. Regular check-ups, screenings, and tests help monitor the pregnancy’s progress and address any potential complications.
As you embark on this journey, remember that every pregnancy is different, and it’s essential to consult with healthcare providers for personalized guidance. Preparing for parenthood involves not only physical preparations but also emotional readiness and building a support system.
Possible References Used



3 Comments