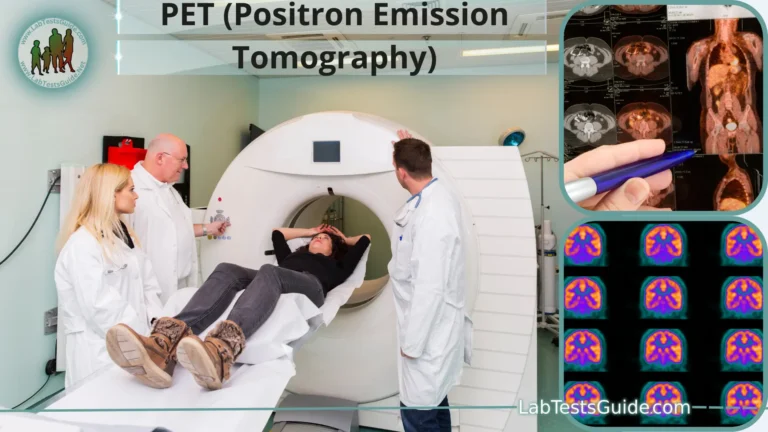
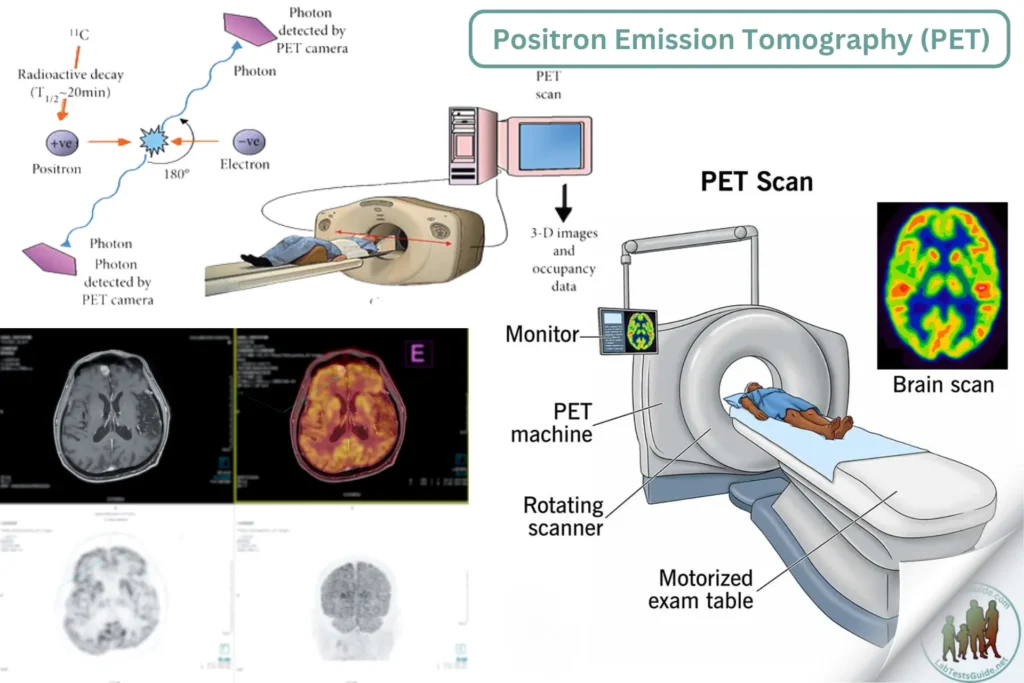
Positron Emission Tomography (PET) is a nuclear medicine imaging technique used to visualize metabolic processes in the body. It is widely used for diagnosing and monitoring cancer, neurological disorders, and cardiovascular diseases by detecting areas of increased or decreased metabolic activity.
Methodology for Positron Emission Tomography (PET) in Clinical Laboratory
Introduction
Positron Emission Tomography (PET) is a nuclear medicine imaging technique used to visualize metabolic processes in the body. It is widely used for diagnosing and monitoring cancer, neurological disorders, and cardiovascular diseases by detecting areas of increased or decreased metabolic activity.
Principle
- PET involves the administration of a radiotracer, typically fluorodeoxyglucose (FDG), which emits positrons as it decays. These positrons interact with electrons in the body, producing gamma rays. The PET scanner detects these gamma rays and constructs detailed images of the body’s metabolic activity.
Patient Preparation
- Patient History: Obtain relevant medical history, including previous imaging studies, surgeries, and current medications.
- Consent: Explain the procedure and obtain informed consent.
- Dietary Restrictions: Instruct patients to fast for at least 4-6 hours before the scan to ensure optimal radiotracer uptake.
- Hydration: Encourage patients to drink water to stay hydrated and facilitate radiotracer distribution.
- Avoid Physical Activity: Advise patients to avoid strenuous physical activity for 24 hours before the scan to reduce background metabolic activity.
- Medication: Review and adjust medications that might interfere with the procedure, such as insulin or glucose-lowering agents.
Reagents and Materials
- Radiotracer (e.g., FDG)
- Intravenous catheters and syringes
- Saline solution for flushing
- Patient gown
- Sedation medications (if needed)
- Quality control materials for radiotracer purity and activity
Equipment
- PET scanner
- Radiopharmaceutical preparation unit (hot lab)
- Gamma counter or dose calibrator
- Blood glucose meter
- Radioprotective shielding and handling tools
- Image reconstruction and analysis software
Procedure
Radiotracer Preparation:
- Prepare the radiotracer according to the manufacturer’s instructions and radiopharmacy protocols.
- Measure the radiotracer’s activity using a dose calibrator to ensure the correct dose.
- Perform quality control tests to verify the radiotracer’s purity and specific activity.
Patient Preparation and Radiotracer Administration:
- Verify patient identity and ensure compliance with pre-scan instructions.
- Measure and record the patient’s blood glucose level to ensure it is within the acceptable range (typically below 200 mg/dL).
- Insert an intravenous catheter and administer the radiotracer.
- Allow the patient to rest in a quiet, dimly lit room for 30-60 minutes to allow for radiotracer uptake.
Imaging:
- Position the patient on the PET scanner table.
- Secure the patient to minimize movement during the scan.
- Perform a scout scan to verify patient positioning.
- Acquire PET images, typically from the base of the skull to the mid-thigh.
- If a PET/CT or PET/MRI scanner is used, acquire corresponding anatomical images for precise localization of metabolic activity.
Image Reconstruction and Analysis:
- Reconstruct PET images using appropriate software, applying corrections for attenuation, scatter, and random coincidences.
- Fuse PET images with CT or MRI images for anatomical reference.
- Analyze the images for areas of abnormal radiotracer uptake, indicating potential pathological conditions.
Quality Control
- Radiotracer Quality: Perform routine checks on radiotracer purity and specific activity.
- Scanner Calibration: Regularly calibrate the PET scanner to ensure accurate image acquisition and quantification.
- Phantom Studies: Use phantoms to test scanner performance and validate imaging protocols.
- Image Quality: Review images for artifacts and ensure adequate resolution and contrast.
Interpretation and Reporting
- Quantitative Analysis: Measure standardized uptake values (SUVs) to quantify radiotracer uptake in regions of interest.
- Qualitative Analysis: Assess images visually for abnormal areas of increased or decreased uptake.
- Reporting: Generate a detailed report describing the findings, including any detected abnormalities and their potential clinical significance.
- Consultation: Discuss findings with referring physicians and recommend further diagnostic tests or follow-up if necessary.
Limitations
- Radiation Exposure: Although PET involves low radiation exposure, it should be minimized and justified by clinical necessity.
- Resolution: PET has lower spatial resolution compared to other imaging modalities like MRI.
- False Positives/Negatives: Non-specific radiotracer uptake can lead to false positives, while small lesions might be missed (false negatives).
Safety Precautions
- Radiation Safety: Follow radiation safety protocols to protect patients, staff, and the public from unnecessary exposure.
- Radiotracer Handling: Use radioprotective shielding and tools to handle radiotracers safely.
- Patient Monitoring: Monitor patients for adverse reactions to the radiotracer and provide appropriate care if needed.
- Waste Disposal: Dispose of radioactive waste according to local regulations and institutional guidelines.
References
- Wahl, R. L., & Buchanan, J. W. (2002). Principles and Practice of Positron Emission Tomography. Lippincott Williams & Wilkins.
- Clinical PET and PET/CT: Principles and Applications by E. Edmund Kim, Myung-Chul Lee, et al.
- Manufacturer’s guidelines for PET scanners and radiotracers.
- Clinical guidelines and standards from institutions such as the Society of Nuclear Medicine and Molecular Imaging (SNMMI) and the European Association of Nuclear Medicine (EANM).
This format provides a comprehensive approach to conducting PET in clinical laboratories, focusing on accurate imaging, quality control, and safety precautions for reliable diagnostic results.
Possible References Used