Obesity is a medical condition characterized by an excessive and unhealthy accumulation of body fat. It is typically defined using the body mass index (BMI), which is a ratio of a person’s weight to their height. A BMI of 30 or higher is generally considered indicative of obesity.
Definition of Obesity
Obesity is a medical condition characterized by the excessive and unhealthy accumulation of body fat, which can have a negative impact on a person’s health. It is typically defined using the body mass index (BMI), which is a ratio of a person’s weight to their height. An individual is generally considered obese if their BMI is 30 or higher.
Obesity results from a complex interplay of genetic, environmental, and lifestyle factors. It occurs when a person consumes more calories than they expend through physical activity and daily metabolic processes, leading to the storage of excess calories as fat in the body.
Causes and Risk Factors:
Here are some of the primary causes and risk factors associated with obesity.
- Genetics: Genetics can play a significant role in determining an individual’s susceptibility to obesity. Some people may have a genetic predisposition that makes it easier for them to gain weight.
Diet and Nutrition:
- Caloric Intake: Consuming more calories than the body needs can lead to weight gain. Overeating and consuming high-calorie, low-nutrient foods can contribute to obesity.
- High Sugar and High-Fat Diets: Diets high in sugar and saturated fats can lead to weight gain, as they are often calorie-dense and lack essential nutrients.
- Large Portion Sizes: Larger portion sizes, common in many fast food and restaurant meals, can lead to overeating.
Physical Activity and Sedentary Behavior:
- Lack of Exercise: A sedentary lifestyle with little or no physical activity can increase the risk of obesity.
- Screen Time: Excessive time spent in front of screens, such as television and computers, can contribute to reduced physical activity.
Environmental Factors:
- Access to Healthy Food: Limited access to affordable, healthy food options can lead to reliance on fast food and processed foods, which are often high in calories and low in nutrients.
- Built Environment: Neighborhoods without sidewalks or safe places for physical activity can discourage exercise.
- Socioeconomic Status: Lower-income individuals may face challenges in accessing nutritious foods and opportunities for physical activity.
Psychological Factors:
- Stress: Chronic stress can lead to emotional eating, where individuals consume high-calorie foods as a coping mechanism.
- Depression and Trauma: Emotional and psychological factors, such as depression or a history of trauma, can contribute to overeating and weight gain.
Medical Conditions:
- Certain medical conditions, such as polycystic ovary syndrome (PCOS) and hypothyroidism, can make it more challenging to maintain a healthy weight.
- Medications: Some medications, like certain antidepressants or corticosteroids, can lead to weight gain as a side effect.
Family and Social Influences:
- Family habits and dynamics can influence eating and exercise habits.
- Social and cultural norms may promote overeating or a sedentary lifestyle.
- Hormonal Factors: Hormonal changes, such as those that occur during pregnancy or menopause, can affect weight.
- Sleep Deprivation: Lack of sleep can disrupt the body’s hormones that regulate appetite, potentially leading to weight gain.
Health Consequences:
Here are some of the major health consequences of obesity.
Cardiovascular Complications:
- Heart Disease: Obesity increases the risk of coronary heart disease, characterized by the buildup of plaque in the coronary arteries.
- Hypertension (High Blood Pressure): Obesity is a major risk factor for high blood pressure, which can lead to heart attacks and stroke.
- Stroke: Obesity is associated with an increased risk of ischemic and hemorrhagic strokes.
Metabolic Disorders:
- Type 2 Diabetes: Obesity is a primary risk factor for type 2 diabetes, as excess fat can lead to insulin resistance and impaired glucose metabolism.
- Insulin Resistance: Obesity can result in reduced sensitivity to insulin, making it harder for the body to regulate blood sugar levels.
- Fatty Liver Disease: Non-alcoholic fatty liver disease (NAFLD) is more common in individuals with obesity and can progress to liver inflammation and fibrosis.
Respiratory and Pulmonary Issues:
- Obstructive Sleep Apnea: Obesity is a leading cause of sleep apnea, a condition characterized by interrupted breathing during sleep.
- Asthma: Obesity is associated with an increased risk of asthma and can make asthma symptoms more severe.
Musculoskeletal Challenges:
- Osteoarthritis: Excess body weight puts added stress on the joints, leading to osteoarthritis, particularly in weight-bearing joints like the knees and hips.
- Back Pain: Obesity can contribute to chronic back pain and spinal issues.
Mental Health Implications:
- Depression: Obesity is linked to higher rates of depression and can negatively affect mental well-being.
- Low Self-Esteem: Body image issues and societal stigma related to obesity can lead to low self-esteem and decreased quality of life.
Cancers:
- Obesity is associated with an increased risk of several types of cancer, including breast, colon, and endometrial cancer.
Reproductive Problems:
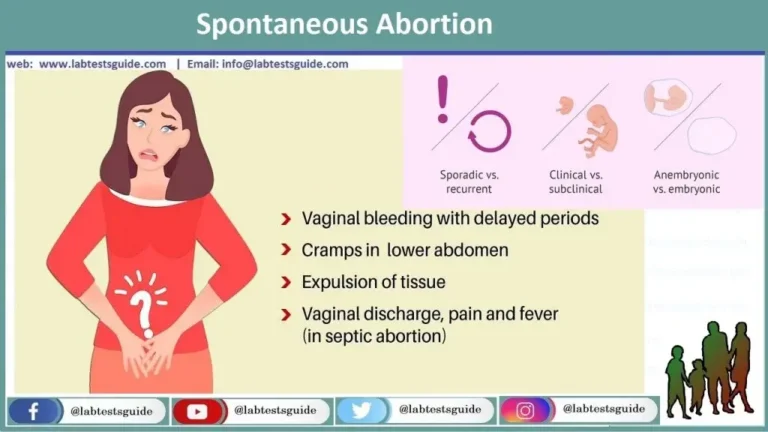
- Infertility: Obesity can lead to hormonal imbalances that impact fertility, and it may reduce the success of fertility treatments.
- Menstrual Irregularities: Obesity can cause irregular menstrual cycles and may increase the risk of polycystic ovary syndrome (PCOS) in women.
Reduced Life Expectancy:
- Obesity is associated with a reduced life expectancy, primarily due to the increased risk of cardiovascular diseases and certain cancers.
Gastrointestinal Issues:
- Gastroesophageal Reflux Disease (GERD): Obesity can contribute to acid reflux and GERD.
- Gallbladder Disease: Obesity is a risk factor for gallstones and gallbladder disease.
Inflammatory and Immune System Changes:
- Obesity is associated with chronic low-grade inflammation, which may contribute to various health problems.
Diagnosis and Assessment:
Here are the key aspects of diagnosing and assessing obesity.
Body Mass Index (BMI):
- Definition: BMI is a commonly used tool to classify obesity. It is calculated by dividing a person’s weight in kilograms by the square of their height in meters. A BMI of 30 or higher is typically considered indicative of obesity.
- Limitations: While BMI provides a quick way to assess weight, it has limitations. It does not take into account body composition (muscle vs. fat), distribution of fat, or other factors that affect health.
Waist Circumference:
- Definition: Measuring waist circumference can provide additional information about the distribution of fat. Excess abdominal fat (central obesity) is associated with a higher risk of health problems.
- Risk Levels: Generally, men with a waist circumference greater than 40 inches (102 cm) and women with a waist circumference greater than 35 inches (88 cm) are considered at increased risk.
Diagnostic Tests and Medical Evaluation:
- Blood Tests: Medical professionals may perform blood tests to measure various markers, including cholesterol levels, triglycerides, and blood sugar, which can provide insight into the individual’s risk of obesity-related health conditions, such as heart disease and diabetes.
- Physical Examination: A comprehensive physical examination by a healthcare provider may include assessments of overall health, joint function, and other factors.
- Assessment of Comorbidities: Identifying and assessing comorbidities (conditions that often accompany obesity) is important, as these conditions may require additional treatment. Common comorbidities include hypertension, type 2 diabetes, sleep apnea, and fatty liver disease.
- Psychosocial Evaluation: Evaluating the individual’s psychological well-being is crucial, as obesity is often associated with mental health issues such as depression and low self-esteem. This evaluation can help inform the treatment plan.
- Family and Medical History: Understanding an individual’s family history and personal medical history can provide insights into the potential genetic and environmental factors contributing to obesity.
- Patient’s Perspective: Listening to the patient’s experiences, challenges, and goals is essential. This patient-centered approach helps create a tailored treatment plan.
- Nutritional Assessment: Assessing the individual’s dietary habits can provide important information for designing a personalized nutrition plan.
- Physical Activity Assessment: Understanding the individual’s physical activity level and exercise habits is crucial for developing an effective weight management plan.
- Body Composition Analysis: In some cases, advanced techniques like dual-energy X-ray absorptiometry (DXA), bioelectrical impedance analysis (BIA), or underwater weighing can be used to assess body composition and the distribution of fat and muscle.
- Long-term Monitoring: Obesity management involves ongoing monitoring of weight, health markers, and progress to adjust treatment plans as needed.
Management and Treatment:
Here are key components of managing and treating obesity.
Lifestyle Modifications:
- Dietary Changes: A registered dietitian or nutritionist can help develop a balanced and sustainable meal plan that focuses on reducing calorie intake and promoting a healthy, nutrient-rich diet. This may involve portion control, reducing sugary and high-fat foods, and increasing consumption of fruits, vegetables, and whole grains.
- Physical Activity: Developing an exercise routine that includes both aerobic (cardiovascular) and strength training exercises can help burn calories and improve overall fitness. A healthcare provider or fitness professional can assist in creating an appropriate exercise plan.
- Behavioral Changes: Behavioral therapy can help individuals identify and address emotional or habitual eating patterns. Techniques such as goal setting, self-monitoring, and stress management can be incorporated into a treatment plan.
Medical Interventions:
- Weight-Loss Medications: In some cases, healthcare providers may prescribe weight-loss medications to assist in weight management. These medications work in different ways, such as suppressing appetite or interfering with the absorption of fat.
- Bariatric Surgery: Surgical interventions may be considered for individuals with severe obesity or those who have not had success with other treatments. Common bariatric procedures include gastric bypass, sleeve gastrectomy, and adjustable gastric banding (e.g., Lap-Band). These surgeries can lead to significant weight loss and may also improve or resolve associated health conditions.
- Multidisciplinary Approach: A team of healthcare professionals, including doctors, dietitians, exercise specialists, and psychologists, may collaborate to provide comprehensive care. This approach addresses the physical, psychological, and nutritional aspects of obesity.
- Support and Education: Education and support are essential components of obesity management. Patients can benefit from understanding the causes of obesity, the importance of making healthy choices, and strategies for maintaining long-term weight loss.
- Monitoring and Follow-up: Regular check-ups with healthcare providers are crucial for tracking progress, adjusting treatment plans, and addressing any potential complications.
- Behavioral Therapy and Counseling: Mental health professionals can help individuals develop strategies to cope with emotional eating, address body image concerns, and manage stress, depression, or anxiety associated with obesity.
- Support Groups and Peer Support: Joining support groups or participating in programs with peers who share similar challenges can provide encouragement and a sense of community.
- Preventive Measures: Encouraging preventive measures at a societal level, including promoting healthier food environments, increasing opportunities for physical activity, and implementing public health policies, can help reduce the prevalence of obesity.
FAQs:
What is obesity?
Obesity is a medical condition characterized by the excessive and unhealthy accumulation of body fat, typically defined using the body mass index (BMI).
What causes obesity?
Obesity results from a combination of genetic, environmental, and lifestyle factors, including genetics, diet, physical activity, and socioeconomic influences.
How is obesity diagnosed?
Obesity is often diagnosed using the BMI, but other factors like waist circumference, body composition, and medical evaluation are considered.
What are the health consequences of obesity?
Obesity is associated with numerous health problems, including heart disease, diabetes, sleep apnea, joint pain, mental health issues, and an increased risk of certain cancers.
How can obesity be treated?
Obesity can be managed through lifestyle modifications, including dietary changes, increased physical activity, and behavioral therapy. In some cases, medical interventions or bariatric surgery may be considered.
What are the best ways to prevent obesity?
Preventing obesity involves promoting a healthy diet, regular physical activity, and creating environments that support these behaviors. Education, community initiatives, and public policies play a role in prevention.
Is there a genetic component to obesity?
Yes, genetics can influence an individual’s susceptibility to obesity, but lifestyle factors and the environment also play a significant role.
What role does the gut microbiome play in obesity?
Research suggests that the composition of the gut microbiome can affect metabolism and weight regulation. Imbalances in the microbiome may contribute to obesity.
Are there effective medications for obesity?
Some medications are available to aid in weight loss, but their use is typically recommended in conjunction with lifestyle changes and under medical supervision.
Is bariatric surgery a common treatment for obesity?
Bariatric surgery is considered for individuals with severe obesity or those who have not had success with other treatments. It can lead to significant weight loss and health improvements.
Can children develop obesity?
Yes, childhood obesity is a significant concern. It can result from a combination of genetic, lifestyle, and environmental factors. Preventing childhood obesity is crucial.
What is the impact of obesity on mental health?
Obesity is associated with an increased risk of mental health issues, including depression and low self-esteem. Body image concerns can also affect mental well-being.
Conclusion
In conclusion, obesity is a complex and pervasive health issue with far-reaching consequences, affecting not only an individual’s physical health but also their mental and emotional well-being. Its multifaceted nature underscores the importance of a comprehensive approach that combines lifestyle changes, medical interventions, and supportive environments. Prevention remains a crucial focus, emphasizing education, policy initiatives, and public health strategies to curb the growing obesity epidemic. As ongoing research provides insights into the causes and management of obesity, it is essential to continue working toward healthier lifestyles, individual well-being, and the reduction of obesity-related health risks on a global scale.
Possible References Used



6 Comments