The presence of two or more embryos in the uterus. Twin and higher gestations have increased considerably in the last two decades due to the increased use of ovulation induction agents and assisted reproductive technologies. Currently, 3% of all births are multiple gestations. When twins are diagnosed by ultrasound at the beginning of the first trimester, in about half of these cases one of the twins will abort silently, and this may or may not be accompanied by bleeding. This phenomenon has been called the missing twin. The incidence of birth defects in each fetus of a twin pregnancy is twice that of single pregnancies. Triplets, quadruplets, and higher gestations are often the result of commonly used fertility drugs. Multiple gestations are associated with an increased risk of perinatal morbidity and mortality.
Definitions
- Dizygotic Twins (66% U.S. twins)
- Fertilization of 2 ova (egg) by 2 sperm
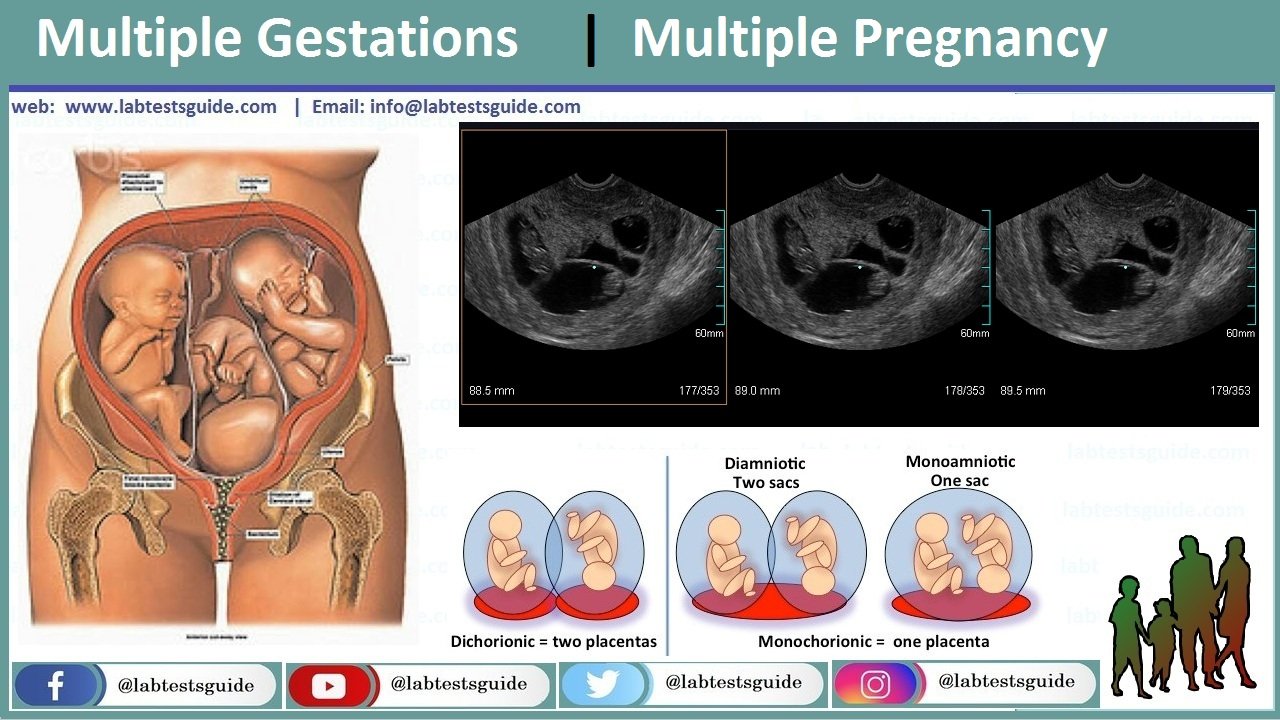
- Dichorionic: Separate chorion (placenta)
- Diamniotic: Separate amnion (amniotic sac)
- Monozygotic Twins (33% U.S twins, identical)
- Division of 1 ova (eggs) fertilized by same sperm
- Ova division <72 hours: Dichorionic, diamniotic
- Ova division 4-8 days: monochorionic, diamniotic
- Ova division 8-13 days: monochorionic, monoamniotic
- Ova division >13 days: Conjoined twins
- Fetus Papyraceous
- One twin does not develop
- Amorphous, shriveled, and flattened twin
Risk factors for Dizygotic twins:
- Older mother
- Multiparous mother
- Family History of dizygotic Twin Gestation
Differential Diagnosis Multiple Gestation (early)
- Misdated pregnancy
- Polyhydramnios
- Uterine Fibroid tumors
- Cyst
- Hydatiform mole
Intrapartum Associated Complications:
- Large Placenta
- Placenta Previa
- Postpartum Hemorrhage
- Large Fetal Demand
- Iron Deficiency Anemia
- Megaloblastic Anemia
- Large bulk or polyhydramnios
- Preterm Labor or Premature Infant
- Pyelonephritis
- Placental Insufficiency
- Growth retardation
- Miscellaneous associated conditions
- Pregnancy Induced Hypertension
- Conjoined twins
- Hyperemesis Gravidarum
- Congenital defect risk doubles in twins
Peripartum Complications
- Umbilical Cord Prolapse
- Fetal Malpresentation
- Placental Abruption
- Postpartum Hemorrhage
- Locked twins
- Description: Twins lock heads
- First twin Breech
- Second twin vertex
- Management
- Push second twin’s head from Pelvis
- Frees first fetus
- Description: Twins lock heads
- Transfusion Syndrome
- Placental AV shunt in monozygotic twins
- Arterial twin
- Pumps blood to other twin
- Starves self
- Other twin
- Bulky and plethoric
- Polycythemic
Management: Pregnancy
- General Measures
- Good diet
- Supplement iron and Folic Acid
- Reduce activity and increase rest
- Clinic visits at least every 2 weeks after 24 weeks
- Cervical checks each visit after 24 weeks
- Preterm Labor Education
- Fetal Movement Counts daily after 32 weeks
- Obstetric Ultrasound every 4-6 weeks after diagnosis
- Assess for Placenta Previa
- Assess Fetal Growth
- Follow Fetal Presentation
- Weekly Nonstress Tests after 32 weeks
- Assess fetal well-being
- Predict cord compression
- Perinatology Consultation as needed
Possible References Used



