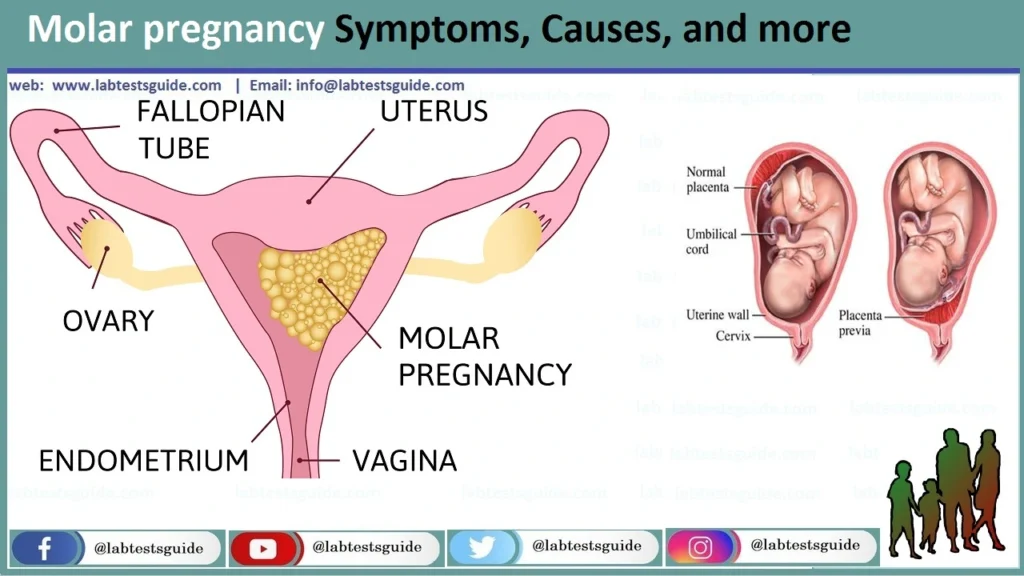
A molar pregnancy, also known as a hydatidiform mole, is a rare complication of pregnancy in which abnormal tissue forms in the uterus instead of a normal embryo. This condition occurs when the fertilization process goes awry, resulting in the growth of abnormal cells instead of a fetus. Molar pregnancies can be classified into two types: complete and partial.
Definition of Molar pregnancy.
A molar pregnancy, also known as a hydatidiform mole, is a rare and abnormal complication of pregnancy characterized by the development of abnormal tissue in the uterus instead of a normal embryo. In a molar pregnancy, the fertilization process goes awry, resulting in the growth of an abnormal mass of cells that typically takes the place of a developing fetus. This abnormal tissue can manifest as grape-like clusters of fluid-filled sacs called vesicles or hydatidiform cysts.
Causes and Risk Factors:
Several factors and risk factors have been associated with molar pregnancies, including.
- Abnormal Fertilization: The most common cause of molar pregnancies is believed to be an abnormal fertilization event.
- A normal egg is fertilized by two sperm (complete molar pregnancy).
- Two sperm fertilize a single egg (partial molar pregnancy).
- These abnormalities in fertilization lead to an excessive proliferation of placental tissue and the formation of vesicles or cysts instead of a normal embryo.
- Maternal Age: Molar pregnancies are more common in women at the extreme ends of the reproductive age spectrum. They are more likely to occur in:
- Women under the age of 20.
- Women over the age of 35.
- Previous Molar Pregnancy: Women who have had one molar pregnancy are at a slightly higher risk of experiencing another molar pregnancy in a subsequent pregnancy.
- Asian Descent: Molar pregnancies are more common in women of Asian descent, particularly those of Southeast Asian or Filipino heritage.
- History of Miscarriage: Women who have a history of multiple miscarriages may have a slightly increased risk of molar pregnancies.
- Nutritional Factors: Some studies suggest that dietary factors, such as a deficiency in certain vitamins and nutrients, may play a role in the development of molar pregnancies. However, this is an area of ongoing research.
Signs and Symptoms:
Here are some symptoms.
- Vaginal Bleeding: The most common and often the first sign of a molar pregnancy is vaginal bleeding. This bleeding can range from light spotting to heavy bleeding and may be accompanied by passage of tissue. The bleeding is usually dark brown or bright red.
- Severe Nausea and Vomiting: Some women with molar pregnancies experience extreme nausea and vomiting, a condition known as hyperemesis gravidarum. This severe morning sickness can be more intense than typical morning sickness in pregnancy.
- Uterine Size Abnormalities: Healthcare providers may detect that the uterus is larger than expected for the gestational age based on physical examination or ultrasound findings. This is because the abnormal placental tissue in a molar pregnancy can grow rapidly and enlarge the uterus.
- Pelvic Pain or Discomfort: Women may experience pelvic pain or discomfort, which can vary in intensity.
- Passage of Grape-Like Clusters: In some cases, women may pass grape-like clusters or vesicles through the vagina. These are the characteristic hydatidiform cysts that form in the uterus during a molar pregnancy.
- High Blood Pressure and Preeclampsia: Molar pregnancies are associated with an increased risk of developing preeclampsia, a condition characterized by high blood pressure, protein in the urine, and swelling of the extremities. Women with molar pregnancies may exhibit signs of preeclampsia.
- Ovarian Cysts: In rare cases, molar pregnancies can lead to the development of ovarian cysts, which may cause abdominal pain or discomfort.
Prevention and Awareness:
Here are some key points related to prevention and awareness.
- Early Prenatal Care: One of the most critical aspects of preventing and managing molar pregnancies is early and regular prenatal care. Women should schedule their first prenatal visit as soon as they suspect they may be pregnant. Early detection and monitoring can help identify and manage molar pregnancies promptly.
- Family Planning and Genetic Counseling: If a woman has a history of molar pregnancy or other reproductive issues, she may consider genetic counseling before becoming pregnant again. Genetic counselors can assess family history and provide guidance on potential risks and preventive measures.
- Healthy Lifestyle: Maintaining a healthy lifestyle before and during pregnancy can reduce the risk of complications. This includes having a balanced diet, getting regular exercise, managing stress, and avoiding tobacco, alcohol, and illicit drugs.
- Education and Awareness: Healthcare providers should educate women about the signs and symptoms of molar pregnancies during routine prenatal care. Increased awareness can lead to early recognition and treatment. Women should also be aware of their own bodies and report any unusual symptoms or changes to their healthcare provider promptly.
- Follow-Up Care: After the treatment of a molar pregnancy, it is essential for women to adhere to their healthcare provider’s recommended follow-up schedule. This typically involves monitoring hCG levels to ensure they return to normal and stay there, as well as regular check-ups to detect any potential complications or the development of gestational trophoblastic disease (GTD).
- Support Groups: Joining support groups or seeking emotional support from healthcare professionals and loved ones can be valuable for women who have experienced a molar pregnancy. Coping with the emotional aspects of this condition is an essential part of the healing process.
- Research and Advocacy: Supporting research efforts aimed at understanding the causes and risk factors of molar pregnancies can contribute to better prevention and management strategies in the future. Advocacy for women’s reproductive health and access to healthcare is also important.
Diagnosis of Molar pregnancy:
Clinical Evaluation:
- Medical History: The healthcare provider will take a detailed medical history, including the patient’s pregnancy history, symptoms, and any relevant risk factors.
- Physical Examination: A pelvic examination may be performed to assess the size and condition of the uterus.
Ultrasound Imaging:
- Transvaginal Ultrasound: This is the primary imaging tool used to diagnose a molar pregnancy. A transvaginal ultrasound allows the healthcare provider to visualize the inside of the uterus and detect abnormalities such as the presence of hydatidiform cysts (grape-like clusters) or other signs of molar pregnancy.
- Characteristics: A complete molar pregnancy often shows a “snowstorm” or “bunch of grapes” appearance on ultrasound due to the presence of numerous small cysts within the uterus. In a partial molar pregnancy, both fetal tissue and cysts may be visible.
Blood Tests:
- hCG Levels: Human chorionic gonadotropin (hCG) is a hormone produced by the placenta during pregnancy. In a molar pregnancy, hCG levels tend to be significantly higher than expected for the gestational age. Serial blood tests to monitor hCG levels are essential for diagnosis and management.
- Rate of Rise: In a molar pregnancy, hCG levels may rise more rapidly than in a normal pregnancy.
- Plateau or Decline: After the removal of molar tissue, hCG levels should return to normal. A plateau or a rise in hCG levels after treatment indicates the presence of persistent molar tissue and the need for further intervention.
- Differential Diagnosis: In some cases, the symptoms of a molar pregnancy, such as vaginal bleeding and uterine enlargement, can overlap with other pregnancy-related conditions or gynecological disorders. Healthcare providers will consider these possibilities and use diagnostic tests to rule out other conditions.
- Confirmation: Once the clinical evaluation, ultrasound imaging, and blood tests support the diagnosis of a molar pregnancy, the healthcare provider will typically proceed with treatment. The definitive confirmation of a molar pregnancy often occurs after the removal of the abnormal tissue through a procedure called dilation and curettage (D&C). Tissue samples obtained during the D&C are sent to a pathology laboratory for examination, which can confirm the diagnosis.
Types of Molar Pregnancy:
There are two primary types of molar pregnancies.
Complete Molar Pregnancy (Complete Hydatidiform Mole):
- In a complete molar pregnancy, there is an empty egg (ovum) that has been fertilized by either one or two sperm. As a result, there is no viable embryo or fetal development.
- Instead of a fetus, the placental tissue grows abnormally and forms a mass of cystic structures within the uterus. These cysts are often described as resembling grape-like clusters or vesicles.
- Complete molar pregnancies typically have a complete absence of fetal tissue, and the entire pregnancy consists of abnormal placental tissue.
Partial Molar Pregnancy (Partial Hydatidiform Mole):
- In a partial molar pregnancy, two sperm fertilize a single egg, resulting in an embryo with an abnormal number of chromosomes (triploid). This leads to the presence of some fetal tissue, but it is not viable and cannot develop into a normal pregnancy.
- Alongside the abnormal fetal tissue, the placental tissue also grows abnormally and may form cystic structures similar to those seen in complete molar pregnancies.
- Partial molar pregnancies have both fetal tissue and abnormal placental tissue.
Treatment and Management:
Dilation and Curettage (D&C):
- D&C is the standard procedure used to remove the abnormal tissue from the uterus. It is usually performed under general anesthesia or local anesthesia with sedation.
- During the procedure, the cervix is dilated (widened), and a curette (a spoon-shaped instrument) is used to gently scrape away the molar tissue from the uterine lining.
- The tissue samples obtained during the D&C are sent to a pathology laboratory for examination to confirm the diagnosis and determine if there are any signs of invasive mole or cancer.
- After the D&C, women may experience some bleeding and cramping, which typically subside in a few days.
Follow-Up Care and Monitoring:
- After the removal of the molar tissue, close monitoring is crucial to ensure that human chorionic gonadotropin (hCG) levels return to normal and stay there.
- Patients will have regular blood tests to measure hCG levels. A sustained decrease and normalization of hCG levels are indicative of successful treatment.
- Follow-up appointments with the healthcare provider are scheduled to monitor the patient’s progress and assess for any potential complications or signs of GTD.
- Contraception: To allow for complete recovery and to avoid another pregnancy during the monitoring period, healthcare providers often recommend contraception for a certain period after the molar pregnancy. Contraceptive methods may include birth control pills, barrier methods, or intrauterine devices (IUDs).
- Preventing Pregnancy: Women are usually advised to delay attempting pregnancy until their healthcare provider confirms that hCG levels have returned to normal and remain so for a specific period. The waiting period can vary depending on individual cases but is typically around 6-12 months.
- Counseling and Emotional Support: Coping with a molar pregnancy can be emotionally challenging. Healthcare providers may offer counseling or refer patients to support groups to help them navigate the emotional aspects of this experience.
- Future Pregnancy Planning: Once a woman has recovered from a molar pregnancy, she can generally plan for future pregnancies. The risk of recurrence is relatively low, but close monitoring during subsequent pregnancies is advisable.
Prognosis and Outcomes:
Here are some key points regarding the prognosis and outcomes.
Complete Molar Pregnancy:
- Complete molar pregnancies, which lack any normal fetal tissue, tend to have a lower risk of complications compared to partial molar pregnancies.
- In most cases, complete molar pregnancies can be effectively treated with a dilation and curettage (D&C) procedure to remove the abnormal tissue.
- The prognosis for complete molar pregnancies is typically excellent, with the vast majority of cases resolving without further issues.
Partial Molar Pregnancy:
- Partial molar pregnancies, which involve both abnormal fetal tissue and abnormal placental tissue, may have a slightly higher risk of complications compared to complete molar pregnancies.
- Treatment for partial molar pregnancies involves D&C as well, but closer monitoring may be necessary to ensure that hCG levels return to normal.
- The prognosis for partial molar pregnancies is generally good, but there may be a slightly higher risk of complications or persistent disease compared to complete molar pregnancies.
Gestational Trophoblastic Disease (GTD):
- In some cases, molar pregnancies can lead to the development of GTD, which includes conditions like invasive mole and choriocarcinoma.
- GTD is rare but can be a serious complication of molar pregnancies. However, with early diagnosis and appropriate treatment, the majority of women with GTD achieve a complete cure and have favorable outcomes.
Recurrence Risk:
- The risk of having a second molar pregnancy in a subsequent pregnancy is generally low, but it may be slightly increased for women who have had one molar pregnancy before.
- Close monitoring and early prenatal care can help detect any signs of a recurrent molar pregnancy.
- Subsequent Pregnancy: Most women who have experienced a molar pregnancy can go on to have healthy pregnancies in the future. It’s essential to delay pregnancy until the healthcare provider confirms that hCG levels have returned to normal and remain stable.
- Emotional Support: Coping with a molar pregnancy and its treatment can be emotionally challenging. Emotional support, counseling, or participation in support groups can be valuable for patients and their families.
Complications:
Here are some of the potential complications associated with molar pregnancies.
Gestational Trophoblastic Disease (GTD):
- GTD is a group of rare conditions that can develop from molar pregnancies. It includes.
- Invasive Mole: In some cases, the molar tissue may invade into the uterine wall or other nearby structures. This condition requires more extensive treatment, often including chemotherapy.
- Choriocarcinoma: Choriocarcinoma is a type of cancer that can develop from the cells of a molar pregnancy. It is highly treatable with chemotherapy, but early detection and treatment are essential.
- Placental Site Trophoblastic Tumor (PSTT): PSTT is another rare type of GTD that can develop from molar pregnancies or other pregnancy-related conditions. It may require chemotherapy or other treatments.
Persistent Trophoblastic Disease (PTD):
- Some women may experience persistently elevated human chorionic gonadotropin (hCG) levels after the removal of molar tissue. This is known as persistent trophoblastic disease.
- PTD may require additional treatment, such as chemotherapy, to eliminate the remaining abnormal cells.
Recurrent Molar Pregnancy:
- While the risk is relatively low, some women who have had one molar pregnancy may experience a second molar pregnancy in a subsequent pregnancy. Close monitoring and early detection are essential to manage any recurrence.
Uterine Rupture:
- In rare cases, molar pregnancies can lead to uterine rupture, a serious medical emergency. Uterine rupture can cause severe bleeding and maternal complications.
Hyperemesis Gravidarum:
- Severe nausea and vomiting, known as hyperemesis gravidarum, can occur in molar pregnancies and may require treatment to manage dehydration and nutritional deficiencies.
Preeclampsia:
- Molar pregnancies are associated with an increased risk of preeclampsia, a condition characterized by high blood pressure and other symptoms. Prompt management of preeclampsia is essential to protect the health of the mother.
Psychological and Emotional Impact:
- Coping with the diagnosis and treatment of a molar pregnancy can be emotionally challenging for both the patient and her family. Emotional support and counseling may be necessary to address the psychological impact.
Research and Advances:
Here are some areas of research and potential advances related to molar pregnancies.
- Genetic Research: Understanding the genetic factors involved in molar pregnancies can help identify individuals at higher risk and potentially lead to preventive measures. Researchers are exploring genetic markers and mutations associated with molar pregnancies.
- Diagnostic Biomarkers: Scientists are investigating new biomarkers and diagnostic tools that could improve the early detection and differentiation of molar pregnancies from other pregnancy-related conditions. This includes the use of molecular markers and advanced imaging techniques.
- Treatment Protocols: Researchers are working to refine treatment protocols for molar pregnancies and GTD. This includes investigating new chemotherapy agents, treatment regimens, and targeted therapies to improve outcomes while minimizing side effects.
- Fertility Preservation: Fertility preservation is a significant concern for many women who undergo treatment for molar pregnancies. Advances in fertility preservation techniques, such as oocyte and embryo cryopreservation, can help individuals preserve their fertility for future pregnancies.
- Patient Education and Support: Research on the psychological and emotional impact of molar pregnancies and GTD is ongoing. Understanding the psychosocial aspects of these conditions can lead to improved patient education, counseling, and support services.
- Telemedicine and Remote Monitoring: Telemedicine and remote monitoring technologies are being explored to facilitate follow-up care for patients, especially those in remote or underserved areas. This can help patients access necessary care and support more conveniently.
- Global Collaboration: Collaboration among healthcare professionals and researchers from around the world is essential to advance our understanding of molar pregnancies and GTD. Sharing knowledge and data can lead to more comprehensive research and better outcomes for patients.
- Preventive Measures: Researchers continue to explore preventive measures for molar pregnancies, especially for individuals with known risk factors. This may include lifestyle modifications or interventions to reduce the risk of recurrence.
- Public Awareness Campaigns: Increased public awareness and education about molar pregnancies can lead to earlier diagnosis and treatment. Efforts to raise awareness and disseminate information about these conditions are ongoing.
- Registry and Data Collection: The establishment of comprehensive registries and databases to collect and analyze information on molar pregnancies and GTD can provide valuable insights for researchers and healthcare providers.
FAQs:
What is a molar pregnancy?
A molar pregnancy is a rare abnormality of pregnancy in which a mass of abnormal tissue grows in the uterus instead of a normal embryo. It is also known as a hydatidiform mole.
What causes a molar pregnancy?
Molar pregnancies are typically caused by abnormal fertilization of an egg. In complete molar pregnancies, the egg is usually empty, and in partial molar pregnancies, two sperm fertilize the egg.
What are the types of molar pregnancies?
There are two primary types: complete molar pregnancies (no fetal tissue) and partial molar pregnancies (some fetal tissue).
What are the common signs and symptoms of a molar pregnancy?
Common signs and symptoms include vaginal bleeding, severe nausea and vomiting (hyperemesis gravidarum), uterine enlargement, and the passage of grape-like clusters or vesicles.
How is a molar pregnancy diagnosed?
Diagnosis typically involves a combination of clinical evaluation, ultrasound imaging, and blood tests to measure human chorionic gonadotropin (hCG) levels.
What is the treatment for a molar pregnancy?
The primary treatment is the removal of the abnormal tissue through a dilation and curettage (D&C) procedure. Chemotherapy may be required in cases of persistent or invasive molar tissue.
What is the prognosis for women with molar pregnancies?
The prognosis is generally good, especially with early diagnosis and appropriate treatment. Most women can go on to have healthy pregnancies in the future.
What are the potential complications of molar pregnancies?
Complications can include the development of gestational trophoblastic disease (GTD), uterine rupture, and, rarely, the persistence of abnormal tissue.
Is it possible to prevent a molar pregnancy?
Molar pregnancies often occur sporadically and are not entirely preventable. Early prenatal care and genetic counseling for high-risk individuals can be beneficial.
Can a woman have a healthy pregnancy after a molar pregnancy?
Yes, most women can have healthy pregnancies in the future after a molar pregnancy, but close monitoring and follow-up care are essential.
Is a molar pregnancy a form of cancer?
No, a molar pregnancy is not a type of cancer, but it can develop into a related condition called gestational trophoblastic disease (GTD), which includes cancerous forms.
Are there support groups or resources for women who have had molar pregnancies?
Yes, there are support groups and organizations that provide information, resources, and emotional support for individuals who have experienced molar pregnancies or GTD.
Conclusion:
In conclusion, a molar pregnancy, characterized by the abnormal growth of tissue in the uterus instead of a normal embryo, is a rare but manageable condition. Early diagnosis, often involving clinical evaluation, ultrasound imaging, and hCG level monitoring, is essential for prompt and effective treatment, which usually entails a dilation and curettage procedure. While complications such as gestational trophoblastic disease can arise, the overall prognosis is favorable, and most women can have healthy pregnancies following appropriate management. Awareness, education, and ongoing research efforts are key to improving outcomes and supporting individuals affected by molar pregnancies.
Possible References Used