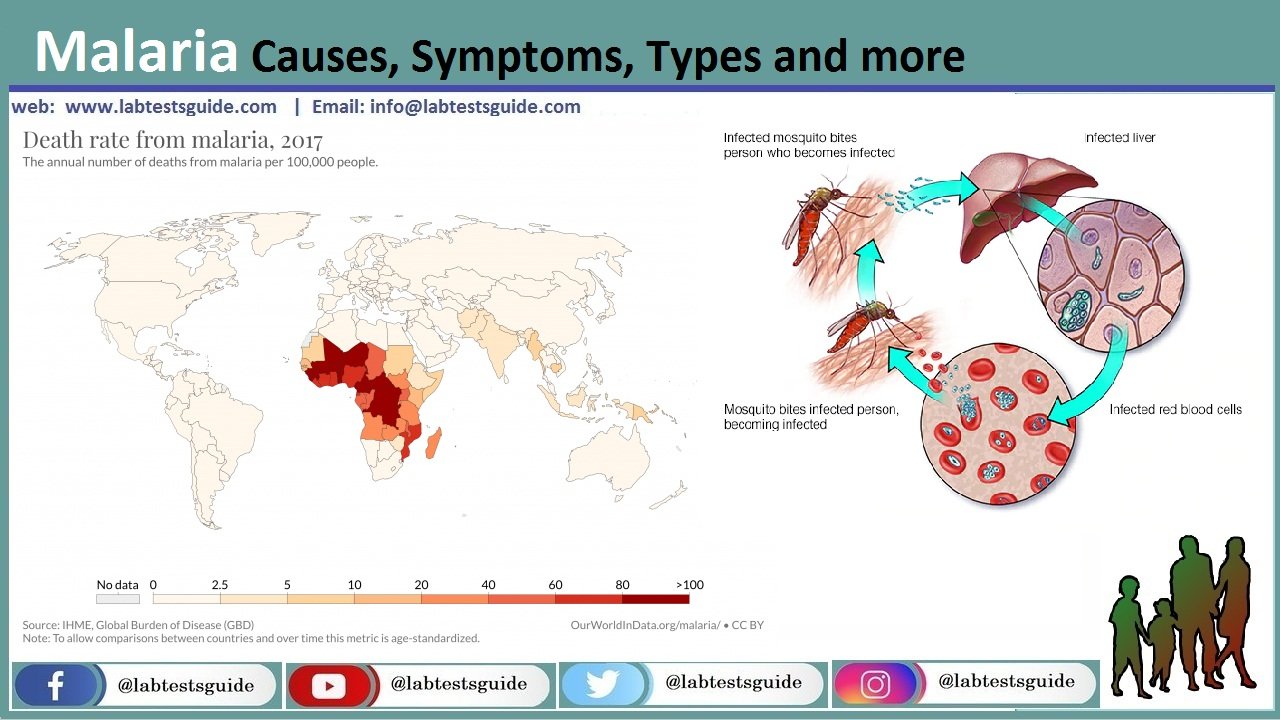
Malaria is a life-threatening disease. It is usually transmitted through the bite of an infected Anopheles mosquito. Infected mosquitoes carry the Plasmodium parasite. When this mosquito bites you, the parasite is released into the bloodstream.
It is important that people who intend to travel to areas where malaria is endemic talk to their healthcare provider about malaria protection before they travel. Their risk of exposure to malaria can be evaluated and proper precautions taken before, during, and after their trip. Even people who have had malaria previously can become reinfected. Similarly, people who originally come from endemic areas are at risk when they return for a visit.
Types:
- P. falciparum.
- P. vivax.
- P. ovale.
- P. malariae.
- A fifth one, P. knowlesi.
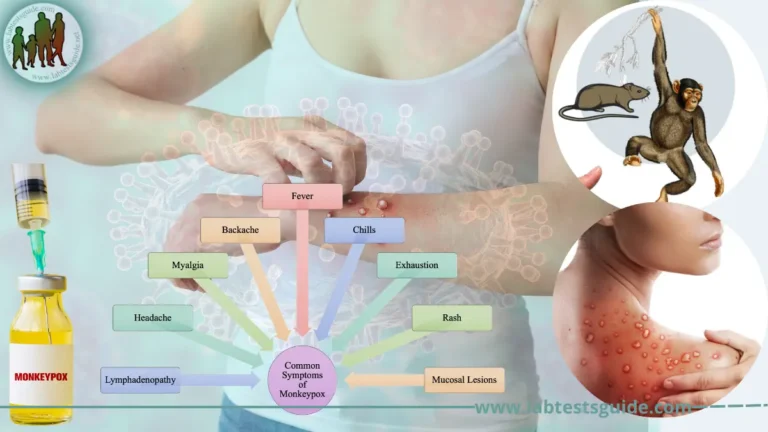
Symptoms:
Common symptoms of malaria include:
- shaking chills that can range from moderate to severe
- high fever
- profuse sweating
- headache
- nausea
- vomiting
- abdominal pain
- diarrhea
- anemia
- muscle pain
- convulsions
- coma
- bloody stools
- How is ma
Causes:
Malaria can occur if a mosquito infected with the Plasmodium parasite bites you. There are four types of malaria parasites that can infect humans: Plasmodium vivax, P. ovale, P. malariae, and P. falciparum.
- Sporozoites from the saliva of a biting female mosquito are transmitted to either the blood or the lymphatic system of the recipient.
- Malaria spreads through:
- Mosquito bite.
- Transfusion malaria from the contaminated transfused blood.
- By sharing contaminated needle and syringes mostly in the drug abusers.
- Congenital malaria which is rare.
Complications Of Malaria:
- The patient may have :
- Cerebral malaria.
- Anemia.
- Organ failure.
- Some patients may have respiratory difficulty.
- Rarely there may be low blood sugar levels.
Diagnosis:
- History of the patient in suspected areas.
- Blood smear:
- Make a blood smear when the patient has a fever. Thin and Thick smears are made.
- The thick smear is more helpful to find M.Parasites.
- The thin smear is good to identify the type of malarial parasite.
- Collect blood 6 to 8 hourly till 48 hours to declare negative for malaria.
- Giemsa stain is the best choice.
- Serologic methods are based on immunochromatic techniques. Tests most often use a dipstick or cassette format and provide results in 2-15 minutes.
- Polymerase chain reaction (PCR): Parasite nucleic acids are detected using the PCR technique. This is more sensitive than smear microscopy. This is of limited value for the diagnosis of acutely ill patients because of the time needed for this procedure.
Prevention:
- No vaccine is available.
- Give prophylactic anti-malarial drugs.
- Use a mosquito net.
- Use mosquito repellant.
Treatment:
- Antimalarial drugs used are quinidine, chloroquine, primaquine, pyrimethamine, sulfadoxine, mefloquine, tetracyclines and proguanil.
- Chloroquine is the drug of choice and best for P. falciparum.
- This is effective for the erythrocytic stage and not for the liver stage.
- Must use primaquine to eradicate P. ovale and P. vivax.
- there are chloroquine resistant cases of P. falciparum.
- Amodiaquin, piperaquin and pyronaridine are close to chloroquin.
- Amodiaquine is less toxic, cheap and in some areas effective against chloroquine-resistant P. falciparum.
- Mefloquine is effective against choloquin resistant P. falciparum.
- Quinine and quinidine are still the first line of therapy against P.falciparum.
- Primaquine is a synthetic drug and is the drug of choice for the eradication of the liver stage from P. vivax and P. ovale.
- Antibiotics and Inhibitors of folate synthesis are slow-acting antimalarial drugs.
- Halofantrine and Lumefantrine are related to quinine and effective against the erythrocytic stage.
- Malaria drug-resistant strains are emerging.
Possible References Used