An intrauterine pregnancy refers to a pregnancy in which a fertilized egg (zygote) successfully implants and grows within the uterus (womb). In humans, the uterus is the organ where a fertilized egg attaches to the uterine lining and develops into an embryo and later a fetus. Intrauterine pregnancies are the most common and natural type of pregnancies in humans.
Definition of Intrauterine Pregnancy:
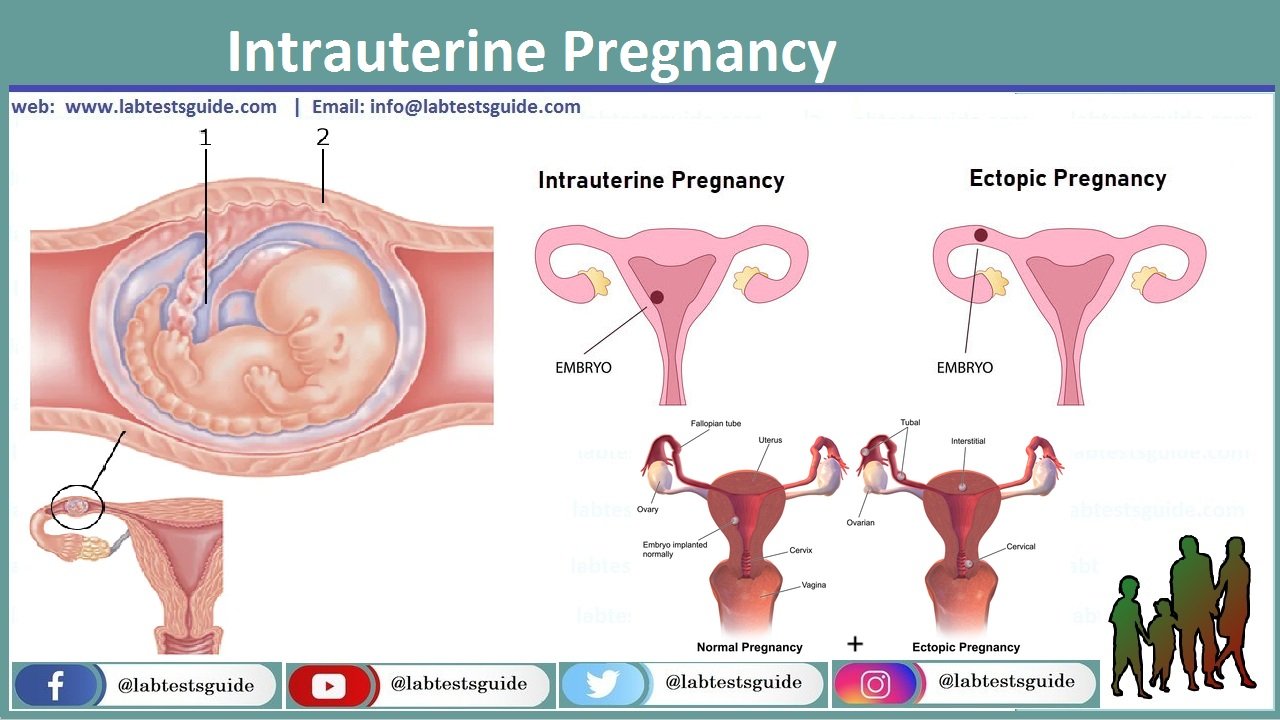
Intrauterine Pregnancy is a medical term that refers to a normal and healthy pregnancy in which a fertilized egg (zygote) successfully implants and develops within the uterus (womb) of a female. In other words, it describes a pregnancy where the developing embryo and later fetus are located and growing inside the uterus as opposed to other locations within the female reproductive system, such as an ectopic pregnancy, where the embryo implants outside the uterus.
Intrauterine pregnancies are the most common and desired type of pregnancies in humans, and they typically follow a natural and healthy course of development, leading to the birth of a healthy baby. Monitoring and appropriate prenatal care are essential to ensure the well-being of both the mother and the developing fetus during an intrauterine pregnancy.
Signs and Symptoms:
Here are some common signs and symptoms associated with intrauterine pregnancy.
- Missed Menstrual Period: One of the earliest signs of pregnancy is a missed period. If you have a regular menstrual cycle and your period is overdue, it could be an indicator of pregnancy.
- Breast Changes: Hormonal changes in pregnancy can lead to breast tenderness, soreness, and swelling. The breasts may also become more sensitive.
- Nausea and Morning Sickness: Many pregnant individuals experience nausea, especially in the morning, although it can occur at any time of day. This is often referred to as morning sickness.
- Frequent Urination: Pregnant women may need to urinate more frequently than usual, especially during the first and third trimesters.
- Fatigue: Increased levels of the hormone progesterone can lead to feelings of fatigue and exhaustion during early pregnancy.
- Food Cravings or Aversions: Some individuals develop strong cravings for certain foods, while others may experience aversions to foods they previously enjoyed.
- Mood Swings: Hormonal changes can also affect mood, leading to mood swings and emotional sensitivity.
- Abdominal Cramping: Mild abdominal cramping can be a normal part of early pregnancy as the uterus begins to stretch and expand.
- Vaginal Changes: Hormonal changes can cause changes in vaginal discharge, which may become thicker and milky white.
- Positive Pregnancy Test: Home pregnancy tests, which detect the presence of the hormone hCG (human chorionic gonadotropin) in the urine, can confirm pregnancy.
- Weight Gain: Gradual weight gain is expected during pregnancy, but it varies depending on the individual and the stage of pregnancy.
- Visible Changes: As the pregnancy progresses, physical changes such as a growing belly and the appearance of stretch marks may become more evident.
- Braxton Hicks Contractions: In the later stages of pregnancy, some individuals experience Braxton Hicks contractions, which are often described as practice contractions. These contractions are not usually painful and do not lead to labor.
Fertilization and Implantation:
Fertilization:
- Definition: Fertilization is the process by which a sperm cell from a male and an egg cell (ovum) from a female combine to form a zygote, which is the first cell of a new individual.
- Location: Fertilization typically occurs in one of the fallopian tubes, which are part of the female reproductive system and connect the ovaries to the uterus.
- Process:
- Ovulation: Fertilization generally occurs during or shortly after ovulation, when a mature egg is released from one of the ovaries.
- Sperm Journey: Sperm cells must travel through the female reproductive tract, including the cervix and uterus, to reach the fallopian tube where the egg awaits.
- Fusion of Gametes: When a sperm successfully penetrates the egg’s outer layer, their genetic material combines, forming a zygote.
- Outcome: The zygote contains the full set of genetic instructions (half from the mother and half from the father) needed for the development of a new individual.
Implantation:
- Definition: Implantation is the process by which the fertilized egg, now called a blastocyst, attaches to and embeds itself into the lining of the uterus.
- Location: Implantation occurs in the uterus.
- Timing: It typically occurs around 6-10 days after fertilization.
- Process:
- Blastocyst Formation: After fertilization, the zygote undergoes multiple cell divisions to form a blastocyst, a hollow ball of cells.
- Attachment: The blastocyst travels through the fallopian tube and enters the uterus. It then attaches to the thickened and vascularized uterine lining, known as the endometrium.
- Implantation: The blastocyst burrows into the endometrial lining and becomes firmly embedded. This establishes a connection between the developing embryo and the mother’s bloodstream, allowing for nutrient and oxygen exchange.
- Outcome: Once implantation is successful, pregnancy is established, and the embryo begins to develop and grow within the uterus.
Developmental Stages:
Here are the main developmental stages of an intrauterine pregnancy.
Zygote Stage:
- Timeframe: This stage begins immediately after fertilization when the sperm and egg combine to form a single-cell zygote.
- Description: The zygote contains the combined genetic material from both parents and begins to undergo a series of cell divisions, forming a cluster of cells.
Morula Stage:
- Timeframe: Approximately 3 days after fertilization.
- Description: The cluster of cells continues to divide, forming a solid ball of cells called the morula.
Blastocyst Stage:
- Timeframe: Around 5-6 days after fertilization.
- Description: The morula undergoes further cell division and differentiates into two distinct cell types: the inner cell mass, which will eventually develop into the embryo, and the outer layer of cells, which will become the placenta. The blastocyst is a hollow, fluid-filled structure.
Embryonic Stage:
- Timeframe: This stage begins after implantation, around 6-10 days after fertilization and lasts until the end of the 10th week of pregnancy (around 8 weeks after conception).
- Description: During this stage, the blastocyst becomes an embryo. The embryo’s cells continue to divide and differentiate, forming the foundation for all the major organs and body systems.
Fetal Stage:
- Timeframe: The fetal stage begins at the end of the 10th week of pregnancy and continues until birth.
- Description: During this stage, the embryo is referred to as a fetus. Major organ systems continue to develop and mature, and the fetus grows significantly in size. The fetus becomes capable of movement, and features such as facial expressions become more pronounced.
Prenatal Care:
Here are key aspects of prenatal care.
Initial Prenatal Visit:
- The first prenatal visit typically occurs early in pregnancy, ideally during the first trimester. During this visit, the healthcare provider gathers essential information about the mother’s medical history, performs a physical examination, and confirms the pregnancy.
- A baseline assessment includes blood pressure, weight measurement, and routine blood tests.
Regular Check-ups:
- Prenatal care involves a series of scheduled check-ups throughout the pregnancy, typically once a month during the first and second trimesters and more frequently during the third trimester.
- During these visits, the healthcare provider monitors the mother’s health and the baby’s growth, checks for signs of complications, and provides guidance on nutrition, exercise, and lifestyle.
Ultrasound Examinations:
- Ultrasound scans are commonly used to visualize the fetus’s development and assess its growth and health. These scans can also provide valuable information about the baby’s anatomy and any potential abnormalities.
- Ultrasounds may be performed at various stages of pregnancy, including the first trimester for dating the pregnancy and detecting multiple pregnancies, and the second trimester for a detailed fetal anatomy scan.
Blood Tests and Screenings:
- Routine blood tests are conducted to monitor the mother’s blood count, blood type, and immunity to certain infections.
- Specialized screenings, such as prenatal genetic testing and screening for conditions like gestational diabetes or preeclampsia, may be recommended based on the mother’s medical history and risk factors.
- Nutritional Guidance: Healthcare providers offer advice on maintaining a balanced diet and taking prenatal vitamins with folic acid to support fetal development.
Weight gain during pregnancy is monitored to ensure it falls within recommended guidelines. - Exercise and Lifestyle Recommendations: Guidance on safe exercise during pregnancy and recommendations for lifestyle adjustments, including avoiding tobacco, alcohol, and certain medications, are provided.
- Education and Counseling: Prenatal care includes educational sessions and counseling on various aspects of pregnancy, childbirth, and postpartum care.
Expectant mothers are encouraged to ask questions and discuss any concerns with their healthcare providers.
- Childbirth Preparation: Prenatal care often includes discussions about birth plans, labor options, and pain management during childbirth.
- Monitoring for Complications: Healthcare providers closely monitor for any signs of complications, such as high blood pressure, gestational diabetes, or preterm labor, and take appropriate actions if needed.
- Emotional Support: Prenatal care may also involve addressing emotional and psychological aspects of pregnancy and providing resources for emotional support.
Complications and Risk Factors:
Here are some common complications and risk factors associated with pregnancy.
Common Pregnancy Complications:
- Gestational Diabetes: Some women develop high blood sugar levels during pregnancy, known as gestational diabetes. It usually resolves after childbirth but requires careful management during pregnancy to prevent complications.
- Preeclampsia: This condition involves high blood pressure and damage to organs such as the liver and kidneys. It typically occurs in the second half of pregnancy and can be serious if left untreated.
- Preterm Birth: Babies born before 37 weeks of gestation are considered preterm. Premature birth can lead to various health challenges for the infant.
- Miscarriage: A miscarriage is the loss of a pregnancy before 20 weeks of gestation. It can occur for various reasons, often related to genetic abnormalities or developmental issues.
- Ectopic Pregnancy: In an ectopic pregnancy, the fertilized egg implants outside the uterus, most commonly in the fallopian tube. This condition is not viable and requires immediate medical attention.
- Placental Problems: Complications related to the placenta, such as placenta previa (when the placenta partially or completely covers the cervix) or placental abruption (when the placenta detaches from the uterus prematurely), can lead to bleeding and other issues.
- Multiple Pregnancy: Carrying twins, triplets, or more can increase the risk of complications such as preterm birth, low birth weight, and preeclampsia.
- Gestational Hypertension: Some women develop high blood pressure during pregnancy, which may not reach the level of preeclampsia but still requires monitoring and management.
Common Risk Factors for Pregnancy Complications:
- Maternal Age: Teenage pregnancies and pregnancies in women over 35 are associated with a higher risk of certain complications.
- Previous Pregnancy Complications: A history of complications in previous pregnancies, such as preterm birth or preeclampsia, may increase the risk of recurrence.
- Medical Conditions: Pre-existing medical conditions like diabetes, hypertension, or autoimmune disorders can increase the risk of pregnancy complications.
- Multiple Pregnancies: Carrying more than one fetus (e.g., twins or triplets) increases the risk of complications.
- Infections: Infections during pregnancy, such as urinary tract infections or sexually transmitted infections, can pose risks to both the mother and the baby.
- Obesity: Being overweight or obese before pregnancy is associated with an increased risk of gestational diabetes, preeclampsia, and other complications.
- Smoking, Alcohol, and Substance Use: These behaviors can harm fetal development and increase the risk of complications.
- Inadequate Prenatal Care: Lack of or infrequent prenatal care can result in undetected complications and inadequate management.
Medical Interventions:
Here are some common medical interventions that may be employed during pregnancy.
Prenatal Screening and Diagnostic Tests:
- Ultrasound: Ultrasound scans are used to visualize the fetus, assess its growth and development, and detect any potential abnormalities.
- Prenatal Genetic Testing: These tests can identify genetic conditions or chromosomal abnormalities in the fetus. Examples include amniocentesis and chorionic villus sampling (CVS).
Management of Pregnancy Complications:
- Gestational Diabetes Management: If a pregnant woman develops gestational diabetes, her healthcare provider may recommend dietary changes, blood sugar monitoring, and, in some cases, insulin therapy.
- Preeclampsia Management: If preeclampsia is diagnosed, management may involve close monitoring of blood pressure, bed rest, medication, or early delivery depending on the severity.
Medications and Treatments:
Medications: In some cases, medications may be prescribed to manage specific conditions during pregnancy, such as antibiotics for infections or anticoagulants for blood clotting disorders.
Rh Incompatibility: Rh-negative mothers carrying Rh-positive fetuses may receive Rh immunoglobulin (RhoGAM) to prevent Rh sensitization, which could affect future pregnancies.
Monitoring and Surveillance:
- Fetal Monitoring: Continuous or intermittent monitoring of the baby’s heart rate may be used during labor to ensure the fetus is tolerating the process.
- Amniotic Fluid Assessment: If there are concerns about amniotic fluid levels, an amniotic fluid index (AFI) may be measured through ultrasound to assess the baby’s environment.
- Cervical Ripening and Induction of Labor: If there are medical reasons for delivering the baby before the onset of spontaneous labor, healthcare providers may recommend cervical ripening methods and induction of labor.
- Cesarean Section (C-Section): A C-section is a surgical procedure in which the baby is delivered through an incision in the mother’s abdomen and uterus. It is performed when vaginal delivery is not safe or feasible due to various reasons, such as fetal distress, breech presentation, or maternal health concerns.
- Neonatal Intensive Care Unit (NICU) Care: In cases where the baby is born prematurely or with certain medical conditions, neonatal intensive care may be necessary to provide specialized medical care and support.
- Postpartum Care: Medical interventions continue after childbirth to ensure that the mother’s recovery is proceeding well and to address any postpartum complications.
Emotional and Psychological Aspects:
Here are some key emotional and psychological aspects associated with pregnancy:
- Anticipation and Excitement: Many expectant parents feel excitement and anticipation as they prepare for the arrival of their baby. This includes setting up the nursery, choosing baby names, and imagining life with a new family member.
- Anxiety and Worry: Pregnancy can bring about concerns and worries about the health of the baby, the labor and delivery process, and the responsibilities of parenthood.
Anxiety may also arise due to uncertainties about pregnancy complications or the challenges of parenting. - Hormonal Changes: Hormonal fluctuations during pregnancy can impact mood and emotions. Some individuals may experience mood swings, increased irritability, or heightened emotional sensitivity.
- Body Image and Self-esteem: Changes in the body’s appearance and weight gain during pregnancy can affect self-esteem and body image. Some individuals may struggle with body image issues or concerns about postpartum changes.
- Fear of Labor and Delivery: Fear of labor and delivery is common among expectant mothers, especially first-time mothers. Education and support can help alleviate these fears.
- Bonding with the Baby: Developing a connection with the unborn baby is a significant emotional aspect of pregnancy. Many parents talk to and play music for the baby in utero as a way to bond.
- Support System: Having a strong support system in the form of a partner, family, friends, or support groups can greatly impact emotional well-being during pregnancy. Emotional support is crucial for expectant mothers.
- Coping with Physical Discomfort: Physical discomforts such as nausea, fatigue, and back pain can have emotional repercussions. Learning to cope with these discomforts is an important aspect of emotional well-being.
- Postpartum Concerns: Anticipating the postpartum period and the emotional changes that may occur after childbirth is important. Postpartum depression and anxiety are conditions that can affect new mothers.
- Preparing for Parenting: Expectant parents may have questions and concerns about their ability to parent effectively. Attending parenting classes and seeking guidance can help with these concerns.
- Emotional Support and Mental Health: Access to emotional support and mental health resources is critical. If expectant parents experience symptoms of depression, anxiety, or other mental health issues, seeking professional help is important.
- Birth Plan and Preferences: Expectant parents often have preferences for their birth experience, such as the type of birth setting (home, hospital, birthing center) and pain management options. These preferences can evoke strong emotions and require careful consideration.
FAQs:
What is the earliest sign of pregnancy?
The earliest sign of pregnancy is often a missed menstrual period. Other early signs can include breast tenderness, nausea, and frequent urination.
When should I take a pregnancy test?
You can take a home pregnancy test about a week after your missed period. Some tests claim to provide accurate results even a few days before your expected period.
What is the difference between prenatal care and postnatal care?
Prenatal care refers to the healthcare and support received during pregnancy, while postnatal care (or postpartum care) is the healthcare and support provided after childbirth to monitor the health of both the mother and the baby.
What is an ultrasound, and when is it typically performed during pregnancy?
An ultrasound is a medical imaging technique that uses sound waves to visualize the developing fetus in the womb. It is performed during pregnancy to monitor the baby’s growth and development. Typically, there are several ultrasound scans during pregnancy, with the first usually occurring around the 8th to 12th week.
What is the difference between a midwife and an obstetrician?
A midwife is a trained healthcare provider who specializes in low-risk pregnancies and natural childbirth. An obstetrician is a medical doctor who specializes in pregnancy, childbirth, and postpartum care, and they are equipped to handle both low-risk and high-risk pregnancies.
How can I manage morning sickness during pregnancy?
Managing morning sickness can include eating small, frequent meals, staying hydrated, getting enough rest, avoiding strong odors or triggers, and, in some cases, using medications recommended by a healthcare provider.
What is the due date, and how is it calculated?
The due date is an estimated date when the baby is expected to be born. It is typically calculated based on the first day of the woman’s last menstrual period (LMP) and adjusted if necessary using ultrasound measurements.
What is a birth plan, and why is it important?
A birth plan is a document that outlines your preferences and wishes for labor, childbirth, and postpartum care. It helps communicate your desires to healthcare providers and ensures you have a voice in your birth experience.
What are common signs of labor?
Common signs of labor include regular contractions, lower back pain, the rupture of the amniotic sac (water breaking), and a bloody show (mucus plug discharge). If you suspect you’re in labor, it’s important to contact your healthcare provider.
What are the different stages of labor?
Labor is typically divided into three stages:
First stage: Contractions begin and the cervix starts to dilate.
Second stage: The baby is born.
Third stage: The placenta is delivered.
What is postpartum depression, and how is it treated?
Postpartum depression is a form of depression that occurs after childbirth. Treatment may include therapy, support groups, and, in some cases, medication prescribed by a healthcare provider.
How long should I wait before getting pregnant again after childbirth?
The ideal time to wait before conceiving again varies from person to person, but most healthcare providers recommend waiting at least 18-24 months after childbirth to allow the body to recover.
Conclusion:
In conclusion, pregnancy is a transformative journey marked by physical, emotional, and psychological changes. From the miraculous processes of fertilization and implantation to the various stages of fetal development, pregnancy is a time of anticipation, growth, and preparation for parenthood. Effective prenatal care, emotional support, and awareness of potential complications are vital for ensuring a healthy pregnancy and safe delivery. Addressing the emotional and psychological aspects, along with seeking medical guidance when needed, contributes to a positive pregnancy experience and sets the stage for a healthy start in the journey of parenthood.
Possible References Used




