Chapter 7 with our Hematology MCQs with Answer and explanations! Test your knowledge and understanding of key concepts with our complete set of multiple choice questions with detailed explanations for each answer.

MCQs:
The exploration of blood and its elements, known as hematology, is vital in diagnosing and treating diverse medical conditions. Professionals in the laboratory focused on hematology conduct a broad spectrum of tests and analyses to assist healthcare practitioners in making precise diagnoses and treatment choices. In order to excel in this field, a profound comprehension of hematology is essential for laboratory personnel, and gaining proficiency in Multiple Choice Questions (MCQs) can prove to be an extremely effective method to attain this objective.
Microbiology MCQs 301 to 350
- Anti-D given to a Rh negative pregnant woman with Rh?positive fetus, before delivery is an example of?
- Artificial active immunity
- Artificial passive immunity
- Natural passive immunity
- Adoptive immunity
Answer and Explanation
Answer: Artificial passive immunity
Administering Anti-D to an Rh-negative pregnant woman prevents her immune system from producing antibodies against Rh-positive blood cells, thereby providing temporary protection for the fetus.
The other options are incorrect:
- Artificial active immunity: This involves stimulating the recipient’s immune system to develop its own antibodies, which takes time. Anti-D provides immediate protection.
- Natural passive immunity: This occurs naturally, like a newborn receiving antibodies from its mother’s breast milk. Anti-D is an injected medication.
- Adoptive immunity: This involves transferring immune cells from another individual, not pre-made antibodies.
- Type of hypersensitivity involved in Rh incompatibility
- Type i hypersensitivity
- Type ii hypersensitivity
- Type iii hypersensitivity
- Type iv hypersensitivity
Answer and Explanation
Answer: Type ii hypersensitivity
In Rh incompatibility, Type II hypersensitivity occurs when maternal antibodies target fetal Rh-positive red blood cells, leading to their destruction.
The other options are incorrect:
- Type I hypersensitivity: Type I hypersensitivity involves immediate allergic reactions mediated by IgE antibodies.
- Type III hypersensitivity: Type III hypersensitivity involves immune complex deposition and inflammation.
- Type IV hypersensitivity: Type IV hypersensitivity involves delayed hypersensitivity reactions mediated by T cells.
- Which of the following cells is not a WBC ?
- Neutrophil
- Basophil
- Manocyte
- Thrombocyte
Answer and Explanation
Answer: Thrombocyte
Thrombocytes, also known as platelets, are not white blood cells. They are small, cell-like fragments derived from megakaryocytes and play a crucial role in blood clotting.
The other options are incorrect:
- Neutrophil: Neutrophils are a type of white blood cell involved in the immune response, particularly in fighting bacterial infections.
- Basophil: Basophils are a type of white blood cell involved in allergic reactions and inflammation.
- Monocyte: Monocytes are a type of white blood cell involved in immune response and can differentiate into macrophages and dendritic cells.
- Name the anticoagulant present in purple coloured vacutainer tube
- Heparin
- EDTA
- Sodium citrate
- None of these
Answer and Explanation
Answer: EDTA (Ethylenediaminetetraacetic acid)
EDTA (Ethylenediaminetetraacetic acid) is used as an anticoagulant in purple-top tubes to prevent blood clotting by chelating calcium ions, which are necessary for the coagulation cascade.
The other options are incorrect:
- Heparin: Heparin is commonly used as an anticoagulant in green-top or blue-top tubes.
- Sodium citrate: Sodium citrate is used as an anticoagulant in blue-top tubes for coagulation studies, not purple-top tubes.
- None of these: There is an anticoagulant present in purple-colored vacutainer tubes, and it is EDTA.
- Which of the following is not an RBC diluting fluid ?
- Normal saline
- Dacies fluid
- Turkes fluid
- Toissons fluid
Answer and Explanation
Answer: Turkes fluid
Turkes fluid is not a commonly used diluting fluid in hematology for RBC counting.
The other options are incorrect:
- Normal saline: Normal saline is a commonly used diluting fluid for RBC counting in hematology.
- Dacies fluid: Dacies fluid is a diluting fluid used for RBC counting.
- Toissons fluid: Toissons fluid is another diluting fluid used for RBC counting.
- Bombay blood group persons have _ antigen in their blood?
- A Ag
- B Ag
- h Ag
- H Ag
Answer and Explanation
Answer: H Ag
The H antigen is the precursor antigen for the ABO blood group system. Individuals with the Bombay blood group lack the H antigen, resulting in the absence of A, B, and H antigens on their red blood cells.
The other options are incorrect:
- A Ag: individuals with the Bombay blood group lack both A and B antigens, but they lack the precursor H antigen.
- B Ag: Individuals with the Bombay blood group lack both A and B antigens, but they lack the precursor H antigen.
- h Ag: The correct term for the antigen is H antigen, not h antigen.
- Depth of improved neubauer counting chamber is
- 0.1 mm
- .01 mm
- .001 mm
- 1 mm
Answer and Explanation
Answer: 0.1 mm
The depth of the counting chamber is crucial for accurate cell counting using a hemocytometer. In the case of an improved Neubauer chamber, the depth is 0.1 mm.
The other options are incorrect:
- 0.01 mm: This depth would be too shallow for accurate cell counting.
- 0.001 mm: This depth would be excessively shallow and impractical for cell counting.
- 1 mm: This depth would be too deep for accurate cell counting and would not be suitable for a Neubauer chamber.
- All the following are examples of blood parasites except?
- Plasmodium
- Brugia malayi
- Leishmania
- Giardia lamblia
Answer and Explanation
Answer: Giardia lamblia
Giardia lamblia is a protozoan parasite that primarily infects the gastrointestinal tract, causing a diarrheal illness called giardiasis.
The other options are incorrect:
- Plasmodium: Plasmodium species are the parasites responsible for causing malaria, a blood-borne disease transmitted by mosquitoes.
- Brugia malayi: Brugia malayi is a filarial worm that causes lymphatic filariasis, a disease affecting the lymphatic system and not directly found in the blood.
- Leishmania: Leishmania parasites are transmitted by sandflies and cause a spectrum of diseases collectively known as leishmaniasis, some of which affect the blood.
- Name the blood cells increased in asthma
- basophil
- neutrophil
- lymphocyte
- Eosinophil
Answer and Explanation
Answer: Eosinophil
Eosinophils are a type of white blood cell that increases in response to allergic conditions such as asthma. They play a role in the inflammation and immune response associated with asthma.
The other options are incorrect:
- Basophil: Basophils may increase in allergic reactions but are not typically associated with asthma.
- Neutrophil: Neutrophils are involved in bacterial infections and acute inflammation but are not specifically increased in asthma.
- Lymphocyte: Lymphocytes are involved in the immune response but are not typically increased in asthma.
- In wintrobes mixture, ammonium oxalate and potassium oxalate is mixed in the ratio?
- 2 : 3
- 3 : 2
- 1 : 4
- 2 : 1
Answer and Explanation
Answer: 2 : 3
Wintrobe’s mixture, used in blood cell sedimentation rate determination (ESR), typically consists of ammonium oxalate and potassium oxalate mixed in the ratio of 2:3.
The other options are incorrect:
- 3:2: This ratio is the reverse of the correct ratio used in Wintrobe’s mixture.
- 1:4: This ratio does not represent the standard composition of Wintrobe’s mixture.
- 2:1: This ratio is not the standard composition used in Wintrobe’s mixture.
- The anticoagulant used in OFT is?
- EDTA
- Citrate
- Heparin
- Sodium flouride-potassium oxalate mixture
Answer and Explanation
Answer: Sodium flouride-potassium oxalate mixture
Sodium fluoride-potassium oxalate mixture is used in OFT to prevent blood clotting and preserve the sample for testing hemoglobin levels.
The other options are incorrect:
- EDTA: EDTA is not commonly used as an anticoagulant in OFT.
- Citrate: Citrate is not typically used as an anticoagulant in OFT.
- Heparin: Heparin is not commonly used as an anticoagulant in OFT.
- Incomplete antibodies are detected using?
- Electrophoresis
- Coombs test
- Agglutination test
- VDRL test
Answer and Explanation
Answer: Coombs test
The Coombs test, also known as the antiglobulin test, is used to detect incomplete antibodies or antibody-coated cells in a patient’s blood.
The other options are incorrect:
- Electrophoresis: Incorrect. Electrophoresis is a technique used to separate molecules based on their size and charge, not specifically for detecting incomplete antibodies.
- Agglutination test: Incorrect. Agglutination tests, such as blood typing tests, detect the presence of specific antibodies or antigens causing the clumping of cells, but they do not specifically target incomplete antibodies.
- VDRL test: Incorrect. The VDRL test is used for detecting antibodies produced in response to Treponema pallidum, the bacterium that causes syphilis. It is not used to detect incomplete antibodies.
- When the entire CBC is suppressed due to either anemia,infection, or hemorrhage is called?
- Erythroplasia
- Thrombocytopenia
- Pancytopenia
- Leukopenia
Answer and Explanation
Answer: Pancytopenia
Pancytopenia refers to a decrease in all three major blood cell types: red blood cells, white blood cells, and platelets, often caused by factors like anemia, infection, or hemorrhage.
The other options are incorrect:
- Erythroplasia: Erythroplasia refers to abnormal red cell production, typically seen in conditions like erythroplakia, a precancerous lesion of the oral mucosa.
- Thrombocytopenia: Thrombocytopenia specifically refers to a decrease in platelet count, not a suppression of the entire CBC.
- Leukopenia: Leukopenia refers to a decrease in white blood cell count, not a suppression of all three blood cell types.
- What is the major metabolically available storage form of iron in the body?
- Hemosiderin
- Ferritin
- Transferrin
- Hemoglobin
Answer and Explanation
Answer: Ferritin
Ferritin serves as the primary storage form of iron in the body, found mainly in the liver, spleen, and bone marrow. It stores iron in a non-toxic, soluble form until it is needed for metabolic processes.
The other options are incorrect:
- Hemosiderin: Hemosiderin is an insoluble form of iron storage, mainly found in cells, and is formed by the breakdown of ferritin.
- Transferrin: Transferrin is a blood plasma glycoprotein that binds to iron and transports it throughout the body, but it is not a storage form of iron.
- Hemoglobin: Hemoglobin is a protein found in red blood cells that carries oxygen, but it is not a storage form of iron.
- The best source of active bone marrow from a 20-year old would be?
- Iliac Crest (hip)
- Femur (thigh)
- Distal radius (forearm)
- Tibia (shin)
Answer and Explanation
Answer: Iliac Crest (hip)
The iliac crest, located on the hipbone, is the most common site for bone marrow aspiration in adults due to its accessibility and abundance of active bone marrow.
The other options are incorrect:
- Femur (thigh): While the femur contains bone marrow, the iliac crest is typically preferred for bone marrow aspiration due to its accessibility and lower risk of complications.
- Distal radius (forearm): The distal radius is not a common site for bone marrow aspiration.
- Tibia (shin): While the tibia contains bone marrow, the iliac crest is generally preferred due to its ease of access and higher concentration of active bone marrow.
- There are 3 classifications of Anemia. What are they?
- In adequate production of Hb
- Decreased RBC production
- Increased Erythrocyte destruction
- Blood loss
Answer and Explanation
Answer: Increased Erythrocyte destruction
Anemia can be classified based on the underlying mechanisms leading to reduced red blood cell count or function. These classifications include inadequate production of hemoglobin, decreased red blood cell production, and increased erythrocyte destruction.
The other options are incorrect:
- Decreased RBC production: This option is partially correct but does not encompass all three classifications of anemia.
- Blood loss: Incorrect. Blood loss is one of the causes of anemia but does not classify anemia itself; it falls under the category of decreased RBC production due to the loss of red blood cells.
- Increased Erythrocyte destruction: This option is partially correct but does not encompass all three classifications of anemia.
- Which test can be used to detect hemolytic anemia?
- Coombs test
- Genetic testing
- Peripheral blood smear (PBS)
- Schilling test
Answer and Explanation
Answer: Coombs test
The Coombs test, also known as the direct antiglobulin test (DAT), detects antibodies or complement proteins that are attached to the surface of red blood cells. This test is valuable in diagnosing autoimmune hemolytic anemia and other forms of hemolytic anemia.
The other options are incorrect:
- Genetic testing: While genetic testing may be useful in some cases of hemolytic anemia, it is not typically used as a primary diagnostic test for this condition.
- Peripheral blood smear (PBS): While a peripheral blood smear can provide information about the morphology of red blood cells, it does not directly detect the presence of antibodies or complement proteins associated with hemolytic anemia.
- Schilling test: The Schilling test is used to evaluate the absorption of vitamin B12 in the digestive tract and is not relevant for diagnosing hemolytic anemia.
- Which anemia is classified as not being able to use iron properly to synthesize hemoglobin because of a inherited cause?
- Iron deficiency anemia
- hypochromic anemia
- aplastic anemia
Answer and Explanation
Answer: hypochromic anemia
Hypochromic anemia refers to a condition where the red blood cells have a reduced amount of hemoglobin, leading to a pale appearance. Inherited disorders affecting hemoglobin synthesis, such as thalassemia and sideroblastic anemia, can result in hypochromic anemia due to the inability to properly utilize iron for hemoglobin production.
The other options are incorrect:
- Iron deficiency anemia: Iron deficiency anemia is characterized by a lack of iron for hemoglobin synthesis, but it is not primarily caused by inherited factors affecting iron utilization.
- Aplastic anemia: Aplastic anemia is a condition where the bone marrow fails to produce enough blood cells, including red blood cells, but it is not primarily caused by inherited factors affecting iron utilization.
- This fatal disorder results from clot/thrombus formation in the blood circulation?
- thromboembolism
- DVT
- PAD
- All of the above
Answer and Explanation
Answer: All of the above
All the listed options (thromboembolism, DVT, PAD) can be fatal disorders resulting from clot/thrombus formation in the blood circulation.
- Thromboembolism: This is a general term for a blood clot (thrombus) that breaks loose from its original location and travels through the bloodstream (embolus). If the embolus lodges in a critical artery, it can block blood flow and cause serious or fatal consequences, such as a stroke or heart attack.
- DVT (Deep Vein Thrombosis): This is a blood clot that forms in a deep vein, usually in the legs. While DVT itself may not be fatal, a complication of DVT is a pulmonary embolism (PE) where the clot breaks loose and travels to the lungs, blocking blood flow and potentially causing death.
- PAD (Peripheral Arterial Disease): This is a condition caused by a buildup of plaque in the arteries that supply blood to the legs and feet. PAD can increase the risk of blood clot formation in these narrowed arteries, which can lead to limb ischemia (tissue death) and potentially be fatal if not treated promptly.
- What is the major metabolically available storage form of iron in the body?
- Hemosiderin
- Ferritin
- Transferrin
- Hemoglobin
Answer and Explanation
Answer: Ferritin
Ferritin acts as the primary intracellular storage protein for iron in the body. It sequesters excess iron and releases it in a controlled manner to meet the body’s needs.
The other options are incorrect:
- Hemosiderin: Hemosiderin is another form of iron storage, primarily found in macrophages as a result of iron overload or breakdown of ferritin, but it is less metabolically available than ferritin.
- Transferrin: Transferrin is a blood plasma protein that transports iron throughout the body but does not store it.
- Hemoglobin: Hemoglobin is the protein in red blood cells responsible for carrying oxygen, but it does not store iron.
- absolute lymphocytosis 5000/mm^3) without adenopathy, hepatosplenomegaly, anemia, thrombocytopenia is what stage in CLL prognosis Scoring-Rai Staging System?
- Stage 0
- Stage I
- Stage II
- Stage III
Answer and Explanation
Answer: Stage 0
Stage 0 in the Rai Staging System indicates early-stage CLL with lymphocytosis but without other signs or symptoms such as lymph node enlargement, hepatosplenomegaly, anemia, or thrombocytopenia.
The other options are incorrect:
- Stage I: Incorrect. Stage I CLL involves lymphocytosis with lymphadenopathy.
- Stage II: Incorrect. Stage II CLL involves lymphocytosis with lymphadenopathy and hepatosplenomegaly.
- Stage III: Incorrect. Stage III CLL involves lymphocytosis with anemia.
- Chronic lymphocytic leukemia is most common leukemia in what kind of people? Slide 4
- young adults
- older adults
- None
Answer and Explanation
Answer: older adults
Chronic lymphocytic leukemia (CLL) is most prevalent in older adults. While it can occur at any age, the incidence increases significantly with age. On average, people are diagnosed with CLL in their seventies.
The other options are incorrect:
- Young adults: CLL is uncommon in young adults.
- None: CLL does have a clear association with older age groups.
- absolute lymphocytosis and thrombocytopenia( < 100,000/mm^3) with or without lymphadenopathy, hepatomegaly, splenomegaly, or anemia is what stage in CLL prognosis Scoring-Rai Staging System?
- Stage 0
- Stage I
- Stage II
- Stage IV
Answer and Explanation
Answer: Stage IV
Stage IV CLL indicates advanced disease with both absolute lymphocytosis and thrombocytopenia, often accompanied by other signs and symptoms such as lymphadenopathy, hepatomegaly, splenomegaly, or anemia.
The other options are incorrect:
- Stage 0: Stage 0 CLL refers to early-stage disease with only lymphocytosis, without other signs or symptoms.
- Stage I: Stage I CLL involves lymphocytosis with lymphadenopathy.
- Stage II: Stage II CLL involves lymphocytosis with lymphadenopathy and hepatosplenomegaly.
- Chronic Lymphocytic Leukemia is characterized by peripheral blood and bone marrow?
- lymphocytopenia
- lymphocytosis
Answer and Explanation
Answer: lymphocytosis
Chronic Lymphocytic Leukemia (CLL) is a type of leukemia characterized by the proliferation of mature, monoclonal B lymphocytes, resulting in elevated lymphocyte counts in the peripheral blood and bone marrow.
The other options are incorrect:
- Lymphocytopenia: CLL is characterized by lymphocytosis, an increase in the number of lymphocytes, rather than lymphocytopenia, which is a decrease in lymphocyte count.
- absolute lymphocytosis with either hepatomegaly or splenomegaly with or without lymphadenopathy is what stage in CLL prognosis Scoring-Rai Staging System?
- Stage 0
- Stage II
- Stage II
- Stage II
Answer and Explanation
Answer: Stage II
Stage II CLL involves lymphocytosis with either hepatomegaly or splenomegaly, with or without lymphadenopathy. This stage signifies more advanced disease compared to Stage 0, but it is less advanced than Stage III or IV.
The other options are incorrect:
- Stage 0: Stage 0 CLL refers to early-stage disease with only lymphocytosis, without other signs or symptoms.
- Stage II: This option is listed twice and does not accurately represent the stages in the Rai Staging System.
- absolute lymphocytosis without lymphadenopathy without hepatosplenomegaly, anemia, or thrombocytopenia is what stage in CLL prognosis Scoring Rai Staging System?
- Stage 0
- Stage I
- Stage II
- Stage II
Answer and Explanation
Answer: Stage 0
Stage 0 CLL indicates early-stage disease characterized solely by absolute lymphocytosis without the presence of other signs or symptoms such as lymphadenopathy, hepatosplenomegaly, anemia, or thrombocytopenia.
The other options are incorrect:
- Stage I: Incorrect. Stage I CLL involves lymphocytosis with lymphadenopathy.
- Stage II: Incorrect. This option is listed twice and does not accurately represent the stages in the Rai Staging System.
- Which of the following forms of Hh molecule has the lowest affinity for oxygen?
- Tense
- Relaxed
- Arterial
- Venous
Answer and Explanation
Answer: Tense
In the tense form of the hemoglobin (Hb) molecule, oxygen affinity is reduced, meaning it has a lower tendency to bind oxygen molecules. This property is essential for efficient oxygen release to tissues in regions with low oxygen concentration.
The other options are incorrect:
- Relaxed: The relaxed form of the Hb molecule has a higher affinity for oxygen, facilitating oxygen binding in the lungs.
- Arterial: Arterial blood contains oxygenated hemoglobin, which typically exists in the relaxed form with high oxygen affinity.
- Venous: Venous blood contains deoxygenated hemoglobin, which can exist in the tense form with reduced oxygen affinity but is not inherently associated with it.
- Intravascular hemolysis is the result of trauma to RBCs while in the circulation
- True
- FALSE
Answer and Explanation
Answer: True
Intravascular hemolysis occurs when red blood cells are damaged or destroyed while circulating within blood vessels. This can happen due to various factors such as mechanical trauma, complement activation, or exposure to toxins.
The other options are incorrect:
- FALSE: The statement is true. Intravascular hemolysis does indeed result from trauma to red blood cells while they are in circulation.
- Blood Hb level changes in mornging and evening Time?
- 1gm%
- 2gm%
- 1.5Gm%
- 2.5gm%
Answer and Explanation
Answer: 1.5Gm%
Hemoglobin levels can vary slightly throughout the day due to factors like hydration status, physical activity, and circadian rhythm. However, the typical range for blood hemoglobin levels is around 1.5 grams per deciliter (gm%) in healthy adults.
The other options are incorrect:
- 1gm%: This value is too low for typical blood hemoglobin levels in healthy adults.
- 2gm%: This value is too high for typical blood hemoglobin levels in healthy adults.
- 2.5gm%: This value is too high for typical blood hemoglobin levels in healthy adults.
- At which month of fetal development does the bone marrow become the primary site of hematopoiesis?
- 2nd
- 5th
- End of 6th month
- End of 7th month
Answer and Explanation
Answer: End of 5th month
During fetal development, hematopoiesis initially occurs in the yolk sac, then shifts to the liver and spleen. By the end of the 5th month, hematopoiesis transitions to the bone marrow, which becomes the primary site for blood cell production.
The other options are incorrect:
- 2nd: Hematopoiesis does not occur in the bone marrow during the 2nd month of fetal development.
- End of 6th month: Hematopoiesis transitions to the bone marrow earlier, by the end of the 5th month, not the end of the 6th month.
- End of 7th month: Hematopoiesis transitions to the bone marrow earlier, by the end of the 5th month, not the end of the 7th month.
- Normal Adult Hb A contains the following polypeptide chains?
- alpha and beta
- alpha and epsilon
- alpha and delta
- alpha and brotherton
Answer and Explanation
Answer: alpha and beta
Hemoglobin A (Hb A) is the predominant type of hemoglobin in adults, composed of two alpha globin chains and two beta globin chains.
The other options are incorrect:
- alpha and epsilon: Epsilon globin chains are characteristic of fetal hemoglobin (Hb F), not adult hemoglobin (Hb A).
- alpha and delta: Delta globin chains are associated with hemoglobin A2 (Hb A2), a minor component of adult hemoglobin, but not with Hb A.
- alpha and brotherton: There is no known globin chain called “brotherton” associated with hemoglobin.
- What is the function of blood?
- to store lipid and cushion organs
- to protect and support organs
- to transport a variety of substances
- to protect and support the body and assist in motion
Answer and Explanation
Answer: to transport a variety of substances
The primary function of blood is to transport oxygen, nutrients, hormones, and waste products throughout the body.
The other options are incorrect:
- To store lipid and cushion organs: While adipose tissue does store lipids and cushions organs, this is not the primary function of blood.
- To protect and support organs: Blood does play a role in protecting organs through immune responses, but its primary function is not to support organs directly.
- To protect and support the body and assist in motion: While blood does contribute to the body’s support and motion through oxygen delivery to muscles and tissues, its primary function is the transportation of substances.
- Which of the following cells is not a WBC ?
- Neutrophil
- Basophil
- Manocyte
- Thrombocyte
Answer and Explanation
Answer: Thrombocyte
Thrombocytes, also known as platelets, are not white blood cells (WBCs); they are fragments of large cells called megakaryocytes and are involved in blood clotting.
The other options are incorrect:
- Neutrophil: Neutrophils are a type of white blood cell involved in immune responses, particularly against bacterial infections.
- Basophil: Basophils are a type of white blood cell involved in allergic reactions and immune responses to parasites.
- Monocyte: Monocytes are a type of white blood cell that can differentiate into macrophages and dendritic cells, playing roles in immune responses and tissue repair.
- Name the anticoagulant present in purple coloured vacutainer tube?
- Heparin
- EDTA
- Sodium citrate
- None of these
Answer and Explanation
Answer: EDTA
The purple top vacutainer tube contains EDTA (Ethylenediaminetetraacetic acid) as the anticoagulant. EDTA chelates calcium ions in the blood, preventing the formation of fibrin clots and allowing for analysis of whole blood or preparation of blood plasma for various tests.
The other options are incorrect:
- Heparin: Heparin is another common anticoagulant, but it’s typically used in light green vacutainer tubes.
- Sodium citrate: Sodium citrate is an anticoagulant used in blue top tubes for tests requiring plasma, such as coagulation studies.pen_spark
- None of these: EDTA is the standard anticoagulant used in purple top tubes.
- HDN due to Rh incompatibility can be prevented by giving anti-D antibody to Rh negative mother within __ hours of delivery of Rh positive infant.
- 48 hrs
- 72 hrs
- 24 hrs
- 36 hrs
Answer and Explanation
Answer: 72 hrs
Administering anti-D antibody to Rh-negative mothers within 72 hours of delivery of an Rh-positive infant helps prevent hemolytic disease of the newborn (HDN) due to Rh incompatibility.
The other options are incorrect:
- 48 hrs: Administration of anti-D antibody within 48 hours may not provide sufficient time to prevent the sensitization of the mother’s immune system.
- 24 hrs: 24 hours may not be adequate for the full effect of the anti-D antibody to be realized in preventing sensitization.
- 36 hrs: While administering anti-D antibody within 36 hours may offer some protection, 72 hours is the recommended timeframe for maximum effectiveness.
- Which of the following is not an RBC diluting fluid ?
- Normal saline
- Dacies fluid
- Turkes fluid
- Toissons fluid
Answer and Explanation
Answer: The other options are incorrect:
Turkes fluid is not an RBC diluting fluid commonly used in hematology.
The other options are incorrect:
- Normal saline: Normal saline is used as an RBC diluting fluid for various purposes in hematology.
- Dacies fluid: Dacies fluid is used as an RBC diluting fluid in certain laboratory procedures.
- Toissons fluid: Toissons fluid is used as an RBC diluting fluid in certain laboratory procedures.
- Which of the following hemoglobins migrates to the same position as Hgb A2 at pH 8.6?
- Hgb H
- Hgb F
- Hgb C
- Hgb S
Answer and Explanation
Answer: Hgb C
At a pH of 8.6, hemoglobin C (Hgb C) migrates to the same electrophoretic position as hemoglobin A2 (Hgb A2) during hemoglobinopathy testing.
The other options are incorrect:
- Hgb H: This type of hemoglobin is caused by alpha chain deletions and typically migrates faster than Hgb A2 at alkaline pH.
- Hgb F: Fetal hemoglobin has a higher affinity for oxygen compared to adult hemoglobin (Hb A). At pH 8.6, it migrates slower than Hgb A2.
- Hgb S: Sickle cell hemoglobin (Hgb S) has a slower migration pattern compared to Hgb A2 at this alkaline pH.
- RBC indices obtained on a patient are as follows: MCV: 88 um^3 MCH: 30 pg MCHC: 34% The RBC on the peripheral smear would appear:
- Microcytic, hypochromic
- Microcytic, normochromic
- Normocytic, normochromic
- Normocytic, hypochromic
Answer and Explanation
Answer: Normocytic, normochromic
With MCV within the normal range and MCHC indicating normochromia, the RBCs would appear normocytic (normal size) and normochromic (normal color) on the peripheral smear.
The other options are incorrect:
- Microcytic, hypochromic: Microcytic RBCs are smaller than normal, and hypochromic RBCs have reduced hemoglobin content. However, the MCV is not suggestive of microcytosis, and the MCHC is within the normal range.
- Microcytic, normochromic: Microcytic RBCs are smaller than normal, but normochromic RBCs have normal hemoglobin content. The MCV is not indicative of microcytosis in this case.
- Normocytic, hypochromic: Normocytic RBCs are of normal size, but hypochromic RBCs have reduced hemoglobin content. However, the MCHC is within the normal range, indicating normochromia.
- A 7.0 mL etheylenediaminetetraacetic acid (EDTA) tube is received in teh lab containing only 2.0 mL of blood. If the lab is using manual techniques, which of the following tests will most likely be erroneous?
- RBC count
- Hemoglobin
- Hct
- WBC count
Answer and Explanation
Answer: Hct
Hct (hematocrit) measures the volume percentage of red blood cells in whole blood. If the tube contains less blood, the Hct result could be falsely elevated due to an increased ratio of red blood cells to plasma.
The other options are incorrect:
- RBC count: While a low blood volume might affect the accuracy of the RBC count, it’s less likely to result in significant error compared to Hct.
- Hemoglobin: Hemoglobin measurement might be affected by the blood volume, but it’s less prone to significant error compared to Hct.
- WBC count: WBC count could be affected by the blood volume, but it’s less likely to be as erroneous as Hct.
- A manual white blood cell count was performed. A total of 36 cells were counted in all 9-mm^2 squares of a Neubauer-ruled hemacytometer. A 1:10 dilution was used. White is the WBC?
- 0.4×10^9/L
- 2.5×10^9/L
- 4.0×10^9/L
- 8.0×10^9/L
Answer and Explanation
Answer: 4.0×10^9/L
With a 1:10 dilution and counting 36 cells in a Neubauer chamber, you’d multiply by 10 (dilution factor) and then by 10 (area correction factor for Neubauer chamber) to get cells per microliter.
The other options are incorrect:
- 0.4×10^9/L: This value is too low; it’s important to account for the dilution and area correction factor.
- 2.5×10^9/L: This value is too low; it’s important to account for the dilution and area correction factor.
- 8.0×10^9/L: This value is too high; it’s important to account for the dilution and area correction factor.
- Which type of antibodies will associate in blood cell coagulation?
- IgE
- IgA
- IgM
- IgG
Answer and Explanation
Answer: IgM
IgM antibodies can associate in blood cell coagulation, particularly in the process known as agglutination, where they can bind to antigens on multiple cells, leading to their clumping together.
The other options are incorrect:
- IgE: IgE antibodies are primarily involved in allergic reactions and defense against parasites, not blood cell coagulation.
- IgA: IgA antibodies are primarily found in mucosal secretions and help prevent pathogens from adhering to mucosal surfaces, not involved in blood cell coagulation.
- IgG: IgG antibodies are involved in various immune responses, including opsonization, but they are not directly associated with blood cell coagulation.
- Blood group antigens are
- Species specific
- Isospecific
- Autospecific
- Organ specific
Answer and Explanation
Answer: Isospecific
Blood group antigens are ispecific. This means they are specific to different blood groups within a single species. For example, the A and B antigens of the ABO blood group system are specific to humans and differentiate between blood types A, B, AB, and O.
The other options are incorrect:
- Species specific: Blood group antigens can differentiate between individuals within a species, not limited to different species entirely.
- Autospecific: This term doesn’t typically apply to blood group antigens. It might be used in autoimmunity, where the immune system attacks the body’s own tissues, but not in blood group systems.
- Organ specific: Blood group antigens are present on red blood cells, and while their expression might vary slightly in some tissues, they are not strictly limited to specific organs.
- T-cells are produced from
- Bonemarrow
- Thymus
- Spleen
- None of these
Answer and Explanation
Answer: Thymus
T-cells undergo maturation and selection in the thymus gland, where they differentiate into various functional subsets.
The other options are incorrect:
- Bone marrow: While bone marrow produces hematopoietic stem cells, which give rise to all blood cells, including T-cell precursors, T-cell maturation occurs primarily in the thymus.
- Spleen: The spleen plays a role in the immune response by filtering blood and removing old or damaged cells, but it is not involved in T-cell production.
- The primary cells involved in immune response are
- NK-cells
- K-cells
- Lymphocytes
- None of these
Answer and Explanation
Answer: Lymphocytes
Lymphocytes, including T cells, B cells, and natural killer (NK) cells, are the primary cells involved in the immune response, responsible for recognizing and targeting pathogens.
The other options are incorrect:
- NK-cells: NK cells are a subset of lymphocytes and are indeed involved in the immune response, but they are not the only primary cells involved.
- K-cells: K-cells are not a recognized term in immunology, so they are not considered primary cells involved in the immune response.
- None of these: Lymphocytes, including NK cells, are indeed primary cells involved in the immune response, so “None of these” is not the correct option.
- Plasma cells are the end cells of
- T-cells
- ß-cells
- Killer cells
- Nk-cells
Answer and Explanation
Answer: ß-cells
Plasma cells are the end cells of B-cells, which differentiate and mature upon encountering antigens, producing antibodies.
The other options are incorrect:
- T-cells: T-cells do not differentiate into plasma cells; they differentiate into various subsets such as helper T cells, cytotoxic T cells, and regulatory T cells.
- Killer cells: “Killer cells” is a general term that can refer to cytotoxic T cells or natural killer (NK) cells, neither of which differentiate into plasma cells.
- NK-cells: NK cells are a type of lymphocyte that is not involved in the production of antibodies or plasma cells.
- Basophils have receptors for antibodies
- IgG
- IgA
- IgM
- IgE
Answer and Explanation
Answer: IgE
Basophils have receptors for IgE antibodies, which play a key role in allergic responses and defense against parasites.
The other options are incorrect:
- IgG: While IgG antibodies are important in various immune responses, basophils primarily have receptors for IgE antibodies.
- IgA: IgA antibodies are mainly found in mucosal secretions and do not typically bind to basophils.
- IgM: IgM antibodies are involved in the primary immune response, but basophils primarily interact with IgE antibodies in allergic reactions.
- In AIDS, Kaposis sarcoma may respond to
- Interleukin – 2 infusion
- Azathioprine
- Alpha interferon
- None of these
Answer and Explanation
Answer: Alpha interferon
In AIDS-related Kaposi’s sarcoma, treatment with alpha interferon has shown some efficacy in managing the disease.
The other options are incorrect:
- Interleukin – 2 infusion: Interleukin-2 has been explored in immunotherapy but is not a primary treatment for AIDS-related Kaposi’s sarcoma.
- Azathioprine: Azathioprine is an immunosuppressive drug used in conditions like organ transplantation or autoimmune diseases, but it is not typically used in the treatment of AIDS-related Kaposi’s sarcoma.
- None of these: Alpha interferon is a known treatment option for AIDS-related Kaposi’s sarcoma, so “None of these” is not the correct option.
- A blood specimen collected in a heparinized tube is centrifuged. It will separate into?
- serum and clot
- plasma and clot
- serum and plasma
- plasma, buffy coat, RBC
Answer and Explanation
Answer: plasma, buffy coat, RBC
When a blood specimen collected in a heparinized tube is centrifuged, it separates into three main layers:
- Plasma: The liquid layer on top, containing all the blood components except cells and platelets. Heparin prevents blood clotting, so fibrin (a component of clots) is not present.
- Buffy coat: A thin middle layer containing white blood cells and platelets.
- RBC (Red Blood Cells): The densest layer at the bottom, consisting of red blood cells.
The other options are incorrect:
- Serum and clot: Heparin prevents clotting, so there won’t be a clot formation. Serum is obtained from blood that has clotted without an anticoagulant like heparin.
- Serum and plasma: Heparinized blood separates into plasma, not serum. Serum is derived from clotted blood.
111
- The test procedure that uses a Westergren tube is?
- erythrocyte sedimentation rate
- hematocrit
- reticulocyte count
- microhematocrit
Answer and Explanation
Answer: erythrocyte sedimentation rate
A Westergren tube is used for the measurement of erythrocyte sedimentation rate, which indicates the rate at which red blood cells settle in a vertical tube of blood over time.
The other options are incorrect:
- Hematocrit: Hematocrit measures the volume percentage of red blood cells in whole blood and is typically determined using a microhematocrit capillary tube or automated analyzer, not a Westergren tube.
- Reticulocyte count: Reticulocyte count measures the percentage of immature red blood cells in the blood and is not performed using a Westergren tube.
- Microhematocrit: Microhematocrit involves centrifuging a capillary tube containing blood to separate its components, particularly to measure hematocrit, but it does not use a Westergren tube.
- Which statement is false when setting up an ESR?
- it must be read in exactly one hour
- it should be set up near a centrifuge
- the blood level must be at exactly zero
- it should be performed on fresh blood
Answer and Explanation
Answer: it should be set up near a centrifuge
The statement that setting up an ESR near a centrifuge is false. ESR should not be set up near a centrifuge to avoid vibration interference.
The other options are incorrect:
- It must be read in exactly one hour: True, ESR should be read precisely one hour after setup.
- The blood level must be at exactly zero: True, the blood level should be at zero before starting the test.
- It should be performed on fresh blood: True, ESR is typically performed on fresh blood samples to ensure accuracy and reliability.
FAQs:
What is Haematology?
Haematology is the branch of medicine that deals with the study of blood and blood-forming tissues.
Why are Haematology MCQs important?
MCQs in Haematology help assess and reinforce understanding of key concepts in blood-related diseases and disorders.
What are the common topics covered in Haematology MCQs?
Topics include anemia, leukemia, coagulation disorders, blood cell morphology, transfusion medicine, and more.
How can I prepare for Haematology MCQs?
Regular study, reviewing textbooks, attending lectures, and practicing with MCQs are effective preparation methods.
What are the types of anemias discussed in Haematology MCQs?
Common types include iron-deficiency anemia, megaloblastic anemia, sickle cell anemia, and thalassemia.
What is the role of coagulation in Haematology?
Coagulation is the process by which blood forms clots, and it is crucial for preventing excessive bleeding.
How are blood disorders diagnosed in Haematology?
Diagnosis involves blood tests, bone marrow examination, and sometimes genetic testing.
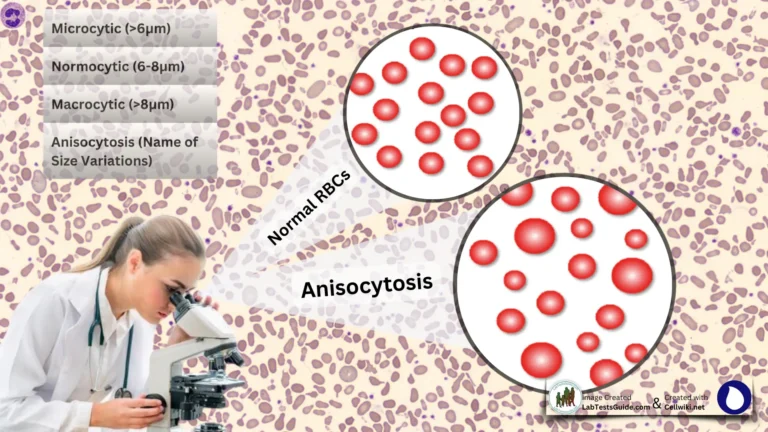
What is the significance of blood cell morphology in Haematology?
Blood cell morphology helps identify and classify various blood disorders based on the appearance of blood cells under the microscope.
Are there any advancements in Haematology that I should be aware of?
Stay updated on new diagnostic techniques, treatment modalities, and research findings in Haematology.
What are the key components of a complete blood count (CBC)?
CBC includes red blood cell count, white blood cell count, hemoglobin level, hematocrit, and platelet count.
How are transfusions managed in Haematology?
Transfusions involve the administration of blood or blood products to patients with certain medical conditions, such as anemia or clotting disorders.
What is the significance of bone marrow in Haematology?
Bone marrow is responsible for the production of blood cells, and abnormalities in the bone marrow can lead to various blood disorders.
What are the major challenges in treating blood cancers?
Challenges include the heterogeneity of blood cancers, the need for personalized therapies, and potential complications from treatment.
How does the immune system relate to Haematology?
The immune system plays a role in conditions such as autoimmune hemolytic anemia and immune thrombocytopenia.
What are the risk factors for developing blood clotting disorders?
Risk factors include genetic predisposition, age, obesity, and certain medical conditions.
Can you recommend any resources for Haematology MCQ practice?
Textbooks, online question banks, and practice exams from reputable sources are useful for MCQ preparation.
How is the management of hemophilia approached in Haematology?
Treatment includes clotting factor replacement therapy, and management plans are tailored to the severity of the condition.
What are some preventive measures for blood disorders?
Preventive measures may include a healthy lifestyle, genetic counseling, and vaccinations.
How does Haematology intersect with other medical specialties?
Haematology is closely related to oncology, immunology, and internal medicine, among other specialties.
What are the future trends in Haematology research?
Keep an eye on advancements in gene therapy, targeted therapies, and precision medicine in the field of Haematology.
Possible References Used