Hektoen Enteric Agar (HE Agar) is a selective and differential agar medium used to isolate and identify Enterobacteriaceae, particularly Salmonella and Shigella. It is a widely used medium in clinical and environmental microbiology.
Hektoen Enteric Agar (HE Agar) is a selective and differential agar medium used to isolate and differentiate enteric pathogens, particularly Salmonella and Shigella. It was developed in 1967 by King and Metzger, and is named after the Hektoen Institute in Chicago, where it was developed.
Key Points of Hektoen Enteric Agar:
- Purpose: HE Agar is used to isolate and identify enteric pathogens, particularly those belonging to the family Enterobacteriaceae.
- Selective Medium: It is a selective medium that inhibits the growth of many non-enteric bacteria, making it specific for enteric organisms.
- Composition: HE Agar typically contains bile salts, bromothymol blue, lactose, sucrose, salicin, ferric ammonium citrate, peptone etc.
- Color Indicator: Bromothymol blue is a pH indicator in the medium and changes color from green to blue as the pH becomes more alkaline.
- Lactose Fermentation: Lactose-fermenting enteric bacteria produce acid during fermentation, leading to a yellow or orange color change in the medium.
- Non-lactose Fermenters: Non-lactose fermenters appear green or blue on HE Agar because they do not produce acid from lactose fermentation.
- Sucrose Fermentation: The medium also differentiates enteric bacteria based on their ability to ferment sucrose.
- Salicin Hydrolysis: Some bacteria can hydrolyze salicin in the medium, producing a black precipitate due to the formation of ferric sulfide.
- Isolation: HE Agar allows for the isolation of pathogens like Salmonella and Shigella from mixed cultures.
- Inhibition of Gram-Positive Bacteria: Bile salts in the medium inhibit the growth of Gram-positive bacteria.
- Indicator of Hydrogen Sulfide Production: The formation of a black precipitate from salicin hydrolysis indicates the production of hydrogen sulfide (H2S).
- Colony Characteristics: The size, color, and morphology of bacterial colonies on HE Agar are used for initial identification.
- Orange to Salmon Pink: Lactose-fermenting bacteria typically produce orange to salmon-pink colonies.
- Green or Blue: Non-lactose fermenters usually produce green or blue colonies.
- Blue-Green to Blue-Black: Bacteria capable of salicin hydrolysis can produce blue-green to blue-black colonies.
- pH Range: HE Agar has a pH range of approximately 7.2 to 7.6.
- Enrichment: HE Agar can be used as an enrichment medium for the recovery of Salmonella from clinical specimens.
- Limitations: HE Agar may not differentiate all enteric bacteria, and additional tests may be required for precise identification.
- Quality Control: It is essential to use quality-controlled media to ensure consistent results.
- Sterile Technique: Strict sterile techniques are necessary when streaking samples onto HE Agar to avoid contamination.
- Clinical Application: HE Agar plays a crucial role in clinical microbiology laboratories for diagnosing enteric infections and is used alongside other tests to confirm the identity of specific pathogens causing gastrointestinal illnesses.
Defination of Hektoen Enteric Agar:
Hektoen Enteric Agar (HE Agar) is a specialized microbiological medium used to selectively isolate and differentiate enteric (intestinal) bacteria based on their ability to ferment carbohydrates and produce characteristic colony colors.
History and Modifications of HE Agar:
- Development: HE Agar was developed by Hektoen and Adler in 1967 as a selective and differential medium for enteric bacteria.
- Original Composition: The original formulation included bile salts, lactose, sucrose, salicin, bromthymol blue, and ferric ammonium citrate.
- Differential Features: It was designed to differentiate enteric bacteria based on lactose fermentation, sucrose fermentation, and salicin hydrolysis.
- Selective Properties: Bile salts in HE Agar inhibited the growth of Gram-positive and non-enteric bacteria while allowing enteric bacteria to grow.
- Color Indicators: Bromthymol blue served as a pH indicator to detect pH changes due to carbohydrate fermentation.
- Black Precipitate: Salicin in the medium allowed for the detection of hydrogen sulfide (H2S) production, resulting in a black precipitate.
- Clinical Significance: HE Agar became a crucial tool in clinical laboratories for diagnosing enteric infections, especially Salmonella and Shigella.
- Modifications: Various modifications have been made to enhance the medium’s performance, selectivity, and ease of use over the years.
- Ingredient Concentrations: Adjustments in ingredient concentrations have been made to optimize its differential properties.
- Selective Agents: Additional selective agents or inhibitors have been incorporated to improve its specificity for certain applications.
- Clinical Relevance: Modifications aim to ensure accurate and efficient isolation and identification of enteric pathogens in clinical and diagnostic settings.
- Quality Control: Quality control measures are implemented to maintain consistent results and reliability in laboratories.
Purpose and Significance of HE Agar:
Purpose:
- Isolation: HE Agar is used for the isolation of enteric (intestinal) bacteria from clinical and environmental samples.
- Selective Medium: It serves as a selective medium by inhibiting the growth of many non-enteric bacteria while allowing the growth of enteric bacteria.
- Differentiation: HE Agar is a differential medium that helps differentiate enteric bacteria based on their ability to ferment specific carbohydrates and produce characteristic colony colors.
- Detection of Pathogens: It is particularly valuable for the isolation and identification of enteric pathogens responsible for gastrointestinal infections, such as Salmonella and Shigella.
- Detection of Hydrogen Sulfide Production: The medium also allows for the detection of hydrogen sulfide (H2S) production by certain bacteria through the formation of a black precipitate when salicin is hydrolyzed.
Significance:
- Clinical Diagnosis: HE Agar plays a crucial role in clinical microbiology laboratories for diagnosing enteric infections, aiding in the selection and identification of potential pathogens.
- Treatment Guidance: It helps guide appropriate treatment decisions by identifying specific enteric bacteria responsible for infections.
- Epidemiological Studies: HE Agar is used in epidemiological studies to track and trace the sources of outbreaks of enteric infections.
- Food Safety: It is employed in food safety testing to detect enteric pathogens in food samples, ensuring the safety of food products.
- Public Health: By identifying enteric pathogens, HE Agar contributes to public health efforts in monitoring and controlling the spread of infectious diseases.
- Research: It is used in research settings to isolate and study enteric bacteria, facilitating a better understanding of their biology and virulence factors.
- Quality Control: HE Agar undergoes quality control measures to ensure reliable and consistent results in microbiological testing.
- Infection Control: Identifying and characterizing enteric pathogens is essential for infection control and prevention in healthcare facilities.
- Monitoring Water Quality: In environmental microbiology, HE Agar can be used to assess water quality and detect fecal contamination by enteric bacteria.
- Teaching and Training: HE Agar is used as an educational tool in microbiology courses to teach students about selective and differential media and bacterial identification.
- Identification of Atypical Strains: It can help identify atypical strains of enteric bacteria that may have unique characteristics or variations in their ability to ferment carbohydrates.
Importance of HE Agar in Microbiology:
- Isolation of Enteric Pathogens: HE Agar is crucial for isolating and culturing enteric (intestinal) pathogens, including Salmonella and Shigella species, from various clinical and environmental samples.
- Selective Medium: It serves as a selective medium by inhibiting the growth of many non-enteric bacteria, ensuring the isolation of target enteric organisms.
- Differential Medium: HE Agar allows for the differentiation of enteric bacteria based on their ability to ferment specific carbohydrates, facilitating the identification of different species and strains.
- Detection of Lactose Fermentation: The medium helps identify lactose-fermenting enteric bacteria, which produce acid and result in colonies with characteristic yellow or orange colors.
- Identification of Non-Lactose Fermenters: Non-lactose fermenters appear as green or blue colonies on HE Agar due to the lack of acid production.
- Salicin Hydrolysis Detection: HE Agar allows for the detection of hydrogen sulfide (H2S) production through the formation of a black precipitate when salicin is hydrolyzed.
- Clinical Diagnosis: It is a vital tool in clinical microbiology for diagnosing enteric infections, guiding appropriate treatment, and providing essential epidemiological information.
- Public Health: By identifying and characterizing enteric pathogens, HE Agar contributes to public health efforts in monitoring and controlling infectious diseases and outbreaks.
- Epidemiological Studies: The medium aids in epidemiological investigations, helping trace the sources and transmission routes of enteric infections.
- Food Safety: HE Agar is used in food safety testing to detect enteric pathogens in food products, ensuring consumer safety.
- Environmental Microbiology: It can be employed in environmental microbiology to assess water quality, detect fecal contamination, and monitor microbial populations in various ecological settings.
- Research: HE Agar is used in research settings to isolate, study, and characterize enteric bacteria, contributing to our understanding of their virulence factors and biology.
- Quality Control: In microbiological laboratories, HE Agar undergoes stringent quality control to ensure consistency and reliability in bacterial identification and isolation.
- Infection Control: Identifying and characterizing enteric pathogens is essential for infection control and prevention in healthcare settings.
- Teaching and Training: HE Agar is used as an educational tool in microbiology courses to teach students about selective and differential media and bacterial identification.
- Identification of Atypical Strains: It can help identify atypical strains of enteric bacteria that may have unique characteristics or variations in their ability to ferment carbohydrates.
Short Overview about Enterobacteriaceae Family:
The Enterobacteriaceae family is a diverse group of Gram-negative bacteria that includes many significant pathogens and commensal organisms. Here’s a short overview:
- Gram-Negative: Enterobacteriaceae are characterized by their Gram-negative cell wall structure, which includes an outer membrane.
- Rod-Shaped: They are typically rod-shaped bacteria, but their size and shape can vary within the family.
- Facultative Anaerobes: Many members of this family can grow both in the presence and absence of oxygen, making them versatile in various environments.
- Fermenters: Enterobacteriaceae are often fermentative, meaning they can metabolize sugars and produce acid and gas as metabolic byproducts.
- Habitat: They inhabit various ecological niches, including the human gastrointestinal tract, soil, water, and plants.
- Pathogenic Species: Several Enterobacteriaceae species are important human pathogens, such as Escherichia coli (E. coli), Salmonella, Shigella, and Yersinia species, which can cause gastrointestinal infections.
- Antibiotic Resistance: Some members of this family have developed antibiotic resistance, posing challenges in healthcare settings.
- Commensal Microbiota: Many Enterobacteriaceae species are part of the commensal microbiota in the human gut, contributing to digestion and other physiological processes.
- Diversity: The family is incredibly diverse, with over 30 genera and hundreds of species, each with its own unique characteristics.
- Clinical Significance: Enterobacteriaceae are significant in clinical microbiology due to their role in various infections, including urinary tract infections, pneumonia, sepsis, and foodborne illnesses.
- Diagnostic Tests: They are identified through various microbiological tests, including biochemical assays and selective/differential agar media like MacConkey Agar and Hektoen Enteric Agar.
- Research: Enterobacteriaceae are subjects of extensive research in microbiology, genetics, and epidemiology, contributing to our understanding of bacterial pathogenesis and evolution.
- Public Health: Monitoring and controlling the spread of Enterobacteriaceae pathogens are essential for public health, especially in outbreak situations.
Principles of HE Agar:
- Selective Medium: HE Agar is a selective medium that inhibits the growth of many non-enteric bacteria while permitting the growth of enteric bacteria. It accomplishes this selectivity primarily through the inclusion of bile salts.
- Differential Medium: In addition to being selective, HE Agar is differential, meaning it allows for the differentiation of various enteric bacteria based on their metabolic activities.
- Carbohydrate Fermentation: One of the key principles of HE Agar is the detection of carbohydrate fermentation by enteric bacteria. It contains carbohydrates like lactose, sucrose, and salicin that can be metabolized by certain bacteria.
- pH Indicator: HE Agar incorporates bromothymol blue as a pH indicator. As bacteria ferment carbohydrates, they produce acid, which leads to a change in the pH of the medium. Bromothymol blue changes color from green to blue as the pH becomes more alkaline.
- Lactose Fermentation: Lactose-fermenting enteric bacteria produce acid as a result of lactose metabolism. This acid production is indicated by colonies with yellow or orange coloration on HE Agar.
- Non-Lactose Fermenters: Enteric bacteria that do not ferment lactose do not produce acid, and their colonies appear green or blue on HE Agar.
- Sucrose Fermentation: HE Agar also contains sucrose, allowing for the differentiation of certain enteric bacteria based on their ability to ferment this carbohydrate.
- Salicin Hydrolysis: Salicin is included in HE Agar to detect hydrogen sulfide (H2S) production. Some bacteria can hydrolyze salicin, leading to the formation of a black precipitate due to the production of ferric sulfide.
- Isolation of Pathogens: HE Agar is commonly used for the isolation of enteric pathogens, including Salmonella and Shigella species, from mixed culture samples.
- Clinical Diagnosis: The principles of HE Agar are applied in clinical microbiology for diagnosing enteric infections, allowing for the selection and differentiation of potential pathogens.
- Quality Control: Ensuring the consistency and reliability of HE Agar in differentiating enteric bacteria is essential in microbiological laboratories.
- Environmental Testing: HE Agar can also be used in environmental microbiology to assess water quality and detect fecal contamination by enteric bacteria.
- Education: It is used as an educational tool in microbiology courses to teach students about selective and differential media and bacterial identification techniques.
Properties of HE Agar:
- Selective: HE Agar is a selective medium that inhibits the growth of non-enteric bacteria, allowing the growth of enteric organisms.
- Differential: It is a differential medium used to differentiate enteric bacteria based on their carbohydrate fermentation and other metabolic activities.
- pH Indicator: HE Agar contains bromothymol blue as a pH indicator, which changes color as pH levels shift during fermentation.
- Lactose Fermentation: It detects lactose fermentation by enteric bacteria, leading to the formation of yellow or orange colonies.
- Non-Lactose Fermenters: Non-lactose fermenting bacteria produce green or blue colonies on HE Agar.
- Salicin Hydrolysis: HE Agar detects hydrogen sulfide (H2S) production through the formation of a black precipitate when salicin is hydrolyzed.
- Isolation: It is used for the isolation of enteric pathogens from mixed cultures, especially in clinical microbiology.
- Clinical Diagnosis: HE Agar aids in the diagnosis of enteric infections, guiding treatment decisions.
- Environmental Testing: It can be used to assess water quality and detect fecal contamination in environmental samples.
- Teaching Tool: HE Agar is used for educational purposes in microbiology courses to demonstrate differential media principles.
Clinical Applications of Hektoen Enteric Agar:
- Diagnosis of Gastrointestinal Infections: HE Agar is used to isolate and differentiate enteric pathogens responsible for gastrointestinal infections, such as Salmonella and Shigella species.
- Treatment Guidance: It assists in selecting appropriate treatments for patients by identifying the specific enteric bacteria causing the infection.
- Epidemiological Investigations: HE Agar is employed in epidemiological studies to trace the source and transmission routes of enteric infections and outbreaks.
- Public Health Surveillance: Monitoring and characterizing enteric pathogens using HE Agar is crucial for public health efforts in controlling the spread of infectious diseases.
- Quality Control: It undergoes quality control measures to ensure reliable and consistent results in clinical microbiology laboratories.
Ingredients, Materials and Composition of HE Agar:
Hektoen Enteric Agar (HE Agar) is a specialized microbiological medium used for the isolation and differentiation of enteric bacteria. Its composition includes various ingredients and materials. Here’s an overview of the typical ingredients, materials, and composition of HE Agar:
Ingredients:
- Protease Peptone: This ingredient serves as a source of amino acids and nutrients to support bacterial growth in the medium.
- Yeast Extract: Yeast extract provides additional nutrients and vitamins to promote the growth of bacteria.
- Lactose: Lactose is a carbohydrate used as a substrate for carbohydrate fermentation testing. Lactose-fermenting bacteria produce acid during fermentation, leading to a change in pH.
- Sucrose: Sucrose is another carbohydrate used to differentiate enteric bacteria based on their ability to ferment this sugar.
- Salicin: Salicin is included in HE Agar for the detection of hydrogen sulfide (H2S) production. Some bacteria can hydrolyze salicin, leading to the formation of a black precipitate due to the production of ferric sulfide.
- Bile Salts Mixture: Bile salts are selective agents that inhibit the growth of many non-enteric bacteria while allowing enteric bacteria to grow. They contribute to the selective nature of the medium.
- Sodium Chloride: Sodium chloride is added to provide the necessary salt concentration for bacterial growth.
- Sodium Thiosulfate: Sodium thiosulfate is used as a source of sulfur, which is required for the production of hydrogen sulfide (H2S) by certain bacteria.
- Ferric Ammonium Citrate: Ferric ammonium citrate is included in HE Agar for the detection of hydrogen sulfide (H2S) production. It reacts with H2S to form a black precipitate.
- Acid Fuchsin: Acid fuchsin is a pH indicator used in the medium.
- Bromothymol Blue: Bromothymol blue is another pH indicator that changes color from green to blue as the pH of the medium becomes more alkaline due to acid production from carbohydrate fermentation.
- Agar: Agar is the solidifying agent that gives the medium its gel-like consistency, allowing for the growth and isolation of bacterial colonies.
Materials:
- Agar: Agar is the solidifying agent that gives HE Agar its gel-like consistency, allowing for the growth and isolation of bacterial colonies.
- Distilled Water: Distilled water is used to dissolve and prepare the agar medium.
- pH Control: The pH of HE Agar is typically adjusted to around 7.2 to 7.6 to maintain suitable conditions for bacterial growth and pH indicator function.
Composition of Hektoen Enteric Agar:
Here is a table summarizing the composition of Hektoen Enteric Agar (HE Agar) with the quantity of each ingredient and its purpose:
| Ingredient | Quantity per Liter of Agar | Purpose |
|---|---|---|
| Protease Peptone | 16 grams | Provides amino acids and nutrients for bacterial growth |
| Yeast Extract | 3 grams | Supplies additional nutrients and vitamins |
| Lactose | 12 grams | Carbohydrate for fermentation and pH indicator |
| Sucrose | 12 grams | Carbohydrate for differentiation |
| Salicin | 2 grams | Detects hydrogen sulfide (H2S) production |
| Bile Salts Mixture | 10 grams | Selective agent inhibiting non-enteric bacteria |
| Sodium Chloride | 5 grams | Provides salt concentration for bacterial growth |
| Sodium Thiosulfate | 0.08 grams | Provides a source of sulfur for H2S production |
| Ferric Ammonium Citrate | 0.012 grams | Detects hydrogen sulfide (H2S) production |
| Acid Fuchsin | 0.002 grams | pH indicator |
| Bromothymol Blue | 0.06 grams | pH indicator |
| Agar | 13.5 grams | Solidifying agent for the medium |
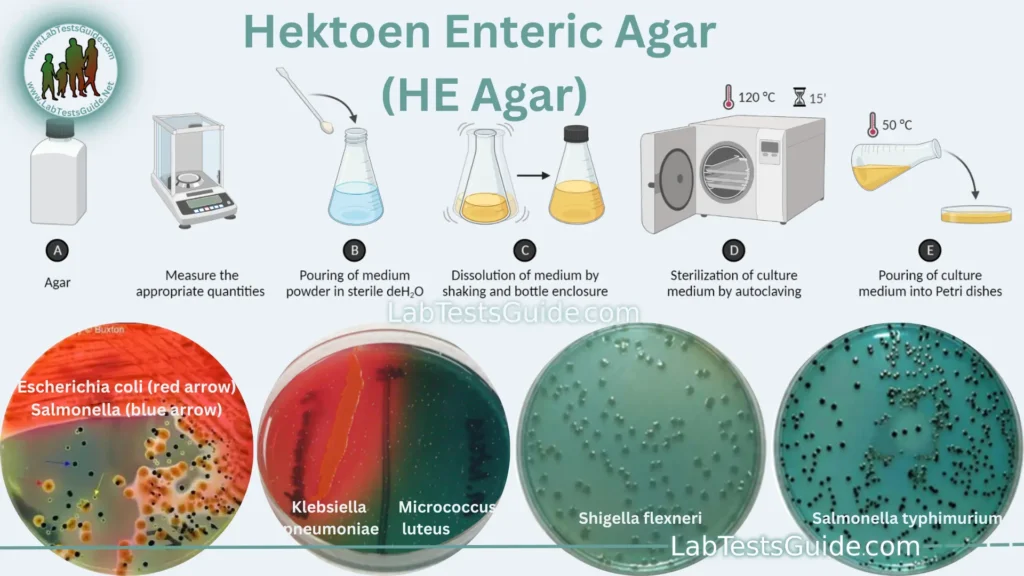
Preparation of HE Agar:
- Gather Materials: Ensure you have all the necessary materials and ingredients ready, including a balance, autoclave, glassware, and HE Agar components.
- Safety Precautions: Follow laboratory safety protocols, including wearing appropriate protective gear such as lab coats and gloves.
- Weigh Ingredients: Weigh out the specified quantities of each ingredient according to the recipe or manufacturer’s instructions.
- Dissolve in Distilled Water: In a large flask or container, dissolve the weighed ingredients in distilled water while stirring gently to avoid clumping.
- Adjust pH: Adjust the pH of the solution to the specified range, typically around 7.2 to 7.6, using pH indicators and pH-adjusting agents as needed. Check the pH using a calibrated pH meter or pH indicator strips.
- Heat and Stir: Heat the mixture while stirring continuously to ensure even distribution and dissolution of the ingredients. Heat until the solution becomes clear.
- Autoclave: Sterilize the medium by autoclaving it at the appropriate temperature (typically 121°C) and pressure for the specified time (usually 15-20 minutes). This step ensures the elimination of any contaminants.
- Cooling: Allow the autoclaved HE Agar to cool but not solidify. Maintain it at a temperature around 45-50°C.
- Pouring Plates: Aseptically pour the molten HE Agar into sterile Petri dishes, filling them to the desired depth for solidification. Use aseptic techniques to prevent contamination.
- Solidification: Allow the poured agar plates to cool and solidify at room temperature. Ensure they are stacked securely to prevent condensation on the agar surface.
- Labeling: Label the agar plates with essential information, such as date of preparation, agar type, and any other relevant details.
- Storage: Store the prepared HE Agar plates in a refrigerator at 2-8°C until they are ready for use. Make sure they are properly sealed to prevent dehydration or contamination.
Required Specimins for Culturing on HE Agar:
Here is a short list of required specimens that can be cultured on Hektoen Enteric Agar (HE Agar) for microbiological testing:
- Fecal Samples: HE Agar is commonly used to culture fecal specimens for the isolation and identification of enteric pathogens responsible for gastrointestinal infections.
- Clinical Stool Samples: Stool samples collected from patients with suspected gastrointestinal infections are routinely cultured on HE Agar for diagnostic purposes.
- Environmental Samples: HE Agar can be used to culture environmental samples from water sources or food products to detect fecal contamination and the presence of enteric bacteria.
- Clinical Isolates: Pure cultures of suspected enteric pathogens obtained from clinical specimens, such as swabs or liquid samples, can be streaked onto HE Agar for isolation and identification.
Usage Procedure of HE Agar:
Here is a list of steps with short descriptions for the usage procedure of Hektoen Enteric Agar (HE Agar) in a microbiological laboratory:
- Prepare the HE Agar Plates:
- Retrieve the HE Agar plates from storage at 2-8°C.
- Ensure the plates are labeled with the necessary information.
- Prepare the Specimen:
- Obtain the specimen to be cultured on HE Agar, which can be a fecal sample, clinical isolate, environmental sample, or clinical stool sample.
- If necessary, use appropriate swabs or inoculating loops to collect the specimen.
- Inoculate the Agar:
- Using aseptic techniques, streak or inoculate the specimen onto the surface of the HE Agar plate. Streak for isolation and even distribution.
- Ensure the agar surface is not excessively wet to prevent spreading of bacteria.
- Incubation:
- Place the inoculated HE Agar plate in an incubator set at the appropriate temperature, typically around 35-37°C.
- Incubate the plate for a specific duration (usually 18-24 hours) to allow bacterial growth.
- Examine for Colonies:
- After incubation, examine the HE Agar plate for the presence of bacterial colonies.
- Observe colony morphology, color, and characteristics.
- Interpretation:
- Interpret the results based on colony characteristics:
- Yellow or orange colonies: Lactose-fermenting bacteria.
- Green or blue colonies: Non-lactose fermenters.
- Black precipitate around colonies: Hydrogen sulfide (H2S) production from salicin hydrolysis.
- Interpret the results based on colony characteristics:
- Subculture (if necessary):
- If identification or further testing is needed, subculture individual colonies onto appropriate differential or selective media for additional characterization.
- Identification:
- Perform additional tests, such as biochemical assays or serological tests, to identify the isolated bacteria to species or strain level.
- Data Recording:
- Record the results of colony morphology, color, and any additional test outcomes in a laboratory notebook or computer system.
- Reporting:
- Prepare a report with the identification of the isolated bacteria and any relevant information for clinical or research purposes.
- Dispose of Waste:
- Dispose of used HE Agar plates and any contaminated materials following laboratory waste disposal protocols.
Result Interpretation of HE Agar:
Interpreting the results of Hektoen Enteric Agar (HE Agar) involves assessing the characteristics of bacterial colonies grown on the agar. HE Agar is used to differentiate enteric bacteria based on their ability to ferment carbohydrates and produce specific colony colors. Here’s a guide to interpreting the results on HE Agar:
- Lactose-Fermenting Bacteria:
- Colony Color: Lactose-fermenting bacteria typically produce colonies with a yellow or orange color.
- Interpretation: Yellow or orange colonies on HE Agar indicate the presence of lactose-fermenting enteric bacteria.
- Non-Lactose Fermenters:
- Colony Color: Non-lactose fermenting bacteria appear as green or blue colonies.
- Interpretation: Green or blue colonies on HE Agar suggest the presence of non-lactose fermenters among the isolated bacteria.
- Salicin Hydrolysis (H2S Production):
- Black Precipitate: Some bacteria have the ability to hydrolyze salicin, resulting in the production of hydrogen sulfide (H2S). This is indicated by the formation of a black precipitate around the colonies.
- Interpretation: The presence of a black precipitate around colonies indicates that the isolated bacteria can produce H2S by hydrolyzing salicin.
- Overall Interpretation:
- HE Agar allows for the differentiation of enteric bacteria into three main categories:
- Lactose-fermenting bacteria (yellow or orange colonies).
- Non-lactose fermenters (green or blue colonies).
- H2S-producing bacteria (black precipitate around colonies).
- HE Agar allows for the differentiation of enteric bacteria into three main categories:
- Further Testing and Identification:
- While HE Agar provides valuable preliminary information, further testing, such as biochemical assays or serological tests, may be required to identify the isolated bacteria to species or strain level.
- Clinical Significance:
- Interpretation of HE Agar results is essential in clinical microbiology for diagnosing enteric infections and guiding appropriate treatment decisions.
- Reporting:
- Record and report the results of HE Agar interpretation, including colony colors and any additional test outcomes, in laboratory reports or clinical records.
Coloney Characteristics of Enterobacteriaceae Family:
Source 1:
| Enterobacteriaceae Member | HE Agar Colony Characteristics |
|---|---|
| Escherichia coli | Yellow to salmon-colored, smooth, convex colonies |
| Salmonella | Yellow to salmon-colored, smooth, convex colonies |
| Shigella | Transparent to pale yellow, smooth, convex colonies |
| Klebsiella | Mucoid, yellow to amber-colored, flat to convex colonies |
| Enterobacter | Yellow to amber-colored, smooth, convex colonies |
| Serratia | Pink to red, smooth, convex colonies |
| Proteus | Swarming, colorless to light amber-colored, flat colonies |
Source 2:
| Organisms | HE Agar Colony Characteristics |
| Salmonella Typhimurium | Blue-green with or without black centers |
| Salmonella Abony | Blue-green with or without black centers |
| Salmonella Enteritidis | Blue-green with or without black centers |
| Salmonella Typhi | Blue-green with or without black centers |
| Escherichia coli | Orange (may have bile precipitate) |
| Shigella flexneri | Greenish blue |
| Shigella sonnei | Growth good to excellent; colonies light green |
| Proteus | Variable, blue-green to blue or salmon, most strains with black center or completely black |
| Enterobacter/Klebsiella | Large, yellow to salmon color |
Growth Other Bacterias on HE Agar:
| Bacteria | HE Agar Colony Characteristics |
|---|---|
| Pseudomonas aeruginosa | Blue-green colonies |
| Acinetobacter baumannii | Pale yellow to amber-colored colonies |
| Enterococcus faecalis | Round, white to cream-colored colonies |
| Staphylococcus aureus | Round, golden yellow colonies |
| Streptococcus pneumoniae | Round, alpha-hemolytic colonies |
Limitations of of HE Agar:
- Selective for Enteric Bacteria: HE Agar is selective for enteric bacteria and inhibits the growth of many non-enteric bacteria. However, it may not entirely exclude all non-enteric contaminants, leading to potential false positives or misleading results.
- Limited Differentiation: While HE Agar can differentiate between lactose-fermenting and non-lactose fermenting enteric bacteria, it does not provide species-level identification. Further testing is often required to accurately identify isolated organisms.
- Variability in Colony Appearance: The colony appearance on HE Agar can vary within and between different species and strains of enteric bacteria. This variability can make interpretation challenging, especially when dealing with atypical isolates.
- Limited Utility for Fastidious Organisms: Some fastidious or slow-growing enteric bacteria may not thrive on HE Agar, leading to false-negative results.
- Interference from Overgrowth: Overgrowth of colonies can obscure the detection of specific colony characteristics, making it difficult to interpret results accurately.
- Interference from Mixed Cultures: HE Agar may not be suitable for samples with mixed cultures, as it can be challenging to differentiate and interpret multiple colony types.
- Inability to Detect All Pathogens: While HE Agar is effective for the isolation and identification of common enteric pathogens, some atypical or less common strains may not exhibit typical colony characteristics on this medium.
- Lack of Sensitivity: HE Agar may not be as sensitive as other specialized media for the detection of certain enteric pathogens, potentially leading to missed infections.
- Limited Utility for Environmental Samples: When used for environmental testing, HE Agar may not provide the specificity needed to differentiate between environmental contaminants and enteric pathogens.
- Subjectivity in Interpretation: Interpretation of colony characteristics on HE Agar can be subjective and may vary among different microbiologists, leading to potential discrepancies in results.
- Quality Control Variability: The quality and performance of commercially prepared HE Agar plates can vary between manufacturers, affecting the consistency and reliability of results.
- Cost and Time: HE Agar may be relatively expensive compared to other culture media, and the time required for incubation and result interpretation can be longer than some rapid diagnostic methods.
Safety Considerations of HE Agar:
- Personal Protective Equipment (PPE): Always wear appropriate PPE, including lab coats, gloves, safety goggles, and, if necessary, a face shield to protect against potential splashes or spills.
- Aseptic Techniques: Use aseptic techniques to minimize the risk of contamination when streaking or inoculating specimens onto HE Agar plates.
- Chemical Handling: Handle the agar components and pH-adjusting chemicals with care. Follow safety data sheet (SDS) guidelines for safe handling, storage, and disposal.
- Autoclave Safety: When autoclaving HE Agar, ensure that containers are tightly sealed, and autoclave conditions are followed precisely to prevent bursting or leaking of agar.
- Hot Surface Awareness: Be cautious of the hot agar when pouring plates or performing inoculations. Allow agar to cool sufficiently before handling.
- Bacterial Cultures: Handle bacterial cultures carefully, especially if they are known pathogens. Follow biosafety guidelines and containment protocols appropriate for the level of risk.
- Disposal: Properly dispose of used HE Agar plates and contaminated materials according to laboratory waste disposal protocols. Autoclave waste before disposal, if required.
- Emergency Procedures: Familiarize yourself with laboratory emergency procedures, including the location of safety showers, eyewash stations, and fire extinguishers.
- Labeling and Documentation: Clearly label all HE Agar plates with the necessary information, including date of preparation, content, and any potential hazards.
- Training: Ensure that laboratory personnel are adequately trained in handling HE Agar and are aware of safety protocols and procedures.
- Report Incidents: Report any accidents, spills, or exposure incidents promptly to laboratory supervisors and follow appropriate reporting procedures.
- Read Manufacturer Instructions: Follow the manufacturer’s instructions for the preparation and use of HE Agar to ensure safe and accurate procedures.
- Ventilation: Work in a well-ventilated area or use a biological safety cabinet when handling potentially infectious samples.
Comparison of HE Agar with Other Microbiological Media:
| spect | HE Agar | MacConkey Agar | Xylose Lysine Deoxycholate (XLD) Agar | Blood Agar |
|---|---|---|---|---|
| Type | Selective and differential medium | Selective and differential medium | Selective and differential medium | General-purpose medium |
| Selectivity | Selective for enteric bacteria | Selective for Gram-negative rods | Selective for Salmonella and Shigella | Not selective |
| Differential | Yes | Yes | Yes | Yes |
| Purpose | Isolation and differentiation of enteric bacteria | Isolation and differentiation of enteric bacteria | Isolation and differentiation of Salmonella and Shigella | Cultivation of a wide range of bacteria |
| Components | Lactose, sucrose, salicin, bile salts, pH indicators | Lactose, bile salts, crystal violet, pH indicators | Lysine, xylose, deoxycholate, phenol red, pH indicators | Blood (sheep or other animals), agar |
| Lactose Fermentation | Yes | Yes | No | Not relevant for Blood Agar |
| Color Indicators | Bromothymol blue and acid fuchsin | Neutral red and crystal violet | Phenol red | No color indicators |
| Detection of H2S | Yes (black precipitate) | No | Yes (black center) | No |
| Use in Clinical Microbiology | Commonly used for isolating and identifying enteric pathogens | Commonly used for enteric pathogen isolation | Used for isolating Salmonella and Shigella | Used for culturing a variety of bacteria |
| Common Applications | Diagnosis of enteric infections, water quality testing, food safety | Isolation of enteric pathogens, detection of lactose fermentation | Isolation of Salmonella and Shigella species | General-purpose media used in many clinical applications |
| Limitations | Limited species-level identification, may not exclude all non-enteric contaminants | Limited species-level identification, may not exclude all contaminants | Limited utility for non-Salmonella/Shigella enteric pathogens | Non-selective, not ideal for selective growth |
| Special Considerations | Requires selective and differential interpretation | Requires selective and differential interpretation | Requires selective interpretation | Used for non-selective cultivation |
| Quality Control | Ensures consistent and reliable results | Ensures consistent and reliable results | Ensures consistent and reliable results | Quality control measures are essential |
Future Trends in Enterobacteriaceae Family:
- Antibiotic Resistance and AMR Surveillance: Continued research into antibiotic resistance mechanisms among Enterobacteriaceae, along with the development of new surveillance methods to monitor the spread of antimicrobial resistance (AMR).
- Genomic Epidemiology: Advances in whole-genome sequencing (WGS) and bioinformatics are expected to enhance the genomic epidemiology of Enterobacteriaceae, allowing for more precise tracking of outbreaks and transmission dynamics.
- Phage Therapy and Alternative Treatments: Investigating the use of bacteriophages and alternative therapies to combat multidrug-resistant Enterobacteriaceae infections, especially in cases where traditional antibiotics are less effective.
- Microbiome Research: Exploring the role of Enterobacteriaceae within the human gut microbiome and its impact on health and disease, including studies on the gut-brain axis and metabolic disorders.
- Vaccine Development: Development and testing of vaccines against Enterobacteriaceae pathogens, such as Salmonella and Shigella, to prevent infections and reduce the burden of these diseases.
- One Health Approach: Emphasis on the One Health approach to understanding Enterobacteriaceae transmission between humans, animals, and the environment, with a focus on zoonotic infections.
- Innovations in Diagnostics: Advancements in diagnostic techniques, including rapid and point-of-care tests, for the early detection and identification of Enterobacteriaceae infections.
- Environmental Reservoirs: Investigation of environmental reservoirs of Enterobacteriaceae and their role in the dissemination of antibiotic resistance genes and pathogens.
- Global Health and Surveillance: Strengthening global surveillance networks to monitor the prevalence and distribution of Enterobacteriaceae infections and AMR patterns, with an emphasis on resource-limited settings.
- Public Health Interventions: Implementation of targeted public health interventions, including infection control measures and antibiotic stewardship programs, to mitigate the impact of Enterobacteriaceae-associated infections.
- Host-Pathogen Interactions: In-depth studies of host-pathogen interactions between Enterobacteriaceae and the host immune system, leading to potential therapeutic strategies.
- Biosecurity and Biodefense: Ongoing research and preparedness efforts related to the potential misuse of Enterobacteriaceae in bioterrorism or biowarfare, as well as laboratory biosecurity measures.
FAQs:
1. What is HE Agar?
- HE Agar, short for Hektoen Enteric Agar, is a selective and differential culture medium used in microbiology to isolate and differentiate enteric bacteria, particularly those responsible for gastrointestinal infections.
2. What are the main components of HE Agar?
- HE Agar contains various components, including peptone, lactose, sucrose, salicin, bile salts, sodium chloride, sodium thiosulfate, ferric ammonium citrate, acid fuchsin, bromothymol blue, and agar as the solidifying agent.
3. What is the purpose of HE Agar in microbiology?
- HE Agar serves the purpose of selectively isolating enteric bacteria and differentiating them based on their ability to ferment carbohydrates, produce hydrogen sulfide (H2S), and create specific colony colors.
4. How does HE Agar differentiate bacteria?
- HE Agar differentiates bacteria through several mechanisms, including lactose fermentation (yellow or orange colonies), non-lactose fermentation (green or blue colonies), and H2S production (black precipitate around colonies).
5. What are some common applications of HE Agar?
- HE Agar is commonly used for diagnosing gastrointestinal infections, isolating enteric pathogens, water quality testing, and environmental sample analysis.
6. Can HE Agar identify bacteria to the species level?
- HE Agar provides preliminary identification by differentiating between lactose-fermenting and non-lactose fermenting enteric bacteria. However, additional tests are usually required for species-level identification.
7. How should HE Agar plates be stored and handled?
- HE Agar plates should be stored at 2-8°C to maintain their integrity. When handling, use aseptic techniques to prevent contamination, and follow safety protocols.
8. What are some limitations of HE Agar?
- Limitations of HE Agar include the potential for false positives/negatives, variability in colony appearance, and the need for additional tests for species-level identification.
9. Can HE Agar be used for environmental samples?
- Yes, HE Agar can be used for environmental samples to detect fecal contamination and the presence of enteric bacteria in water or food products.
10. How long does it take to incubate HE Agar plates?
- Typically, HE Agar plates are incubated at around 35-37°C for 18-24 hours, but incubation times may vary depending on the specific application and laboratory protocols.
Conclusion:
In conclusion, Hektoen Enteric Agar (HE Agar) is a valuable tool in microbiology for the isolation and differentiation of enteric bacteria, particularly those associated with gastrointestinal infections. Its selective and differential properties make it a useful medium for identifying lactose-fermenting and non-lactose fermenting bacteria, as well as those capable of hydrogen sulfide (H2S) production.
HE Agar’s ability to provide preliminary information about bacterial pathogens in clinical, environmental, and food safety contexts is essential for diagnosis, research, and public health efforts. However, it’s important to recognize the limitations of HE Agar, such as its inability to identify bacteria to the species level and the potential for false results.
Possible References Used