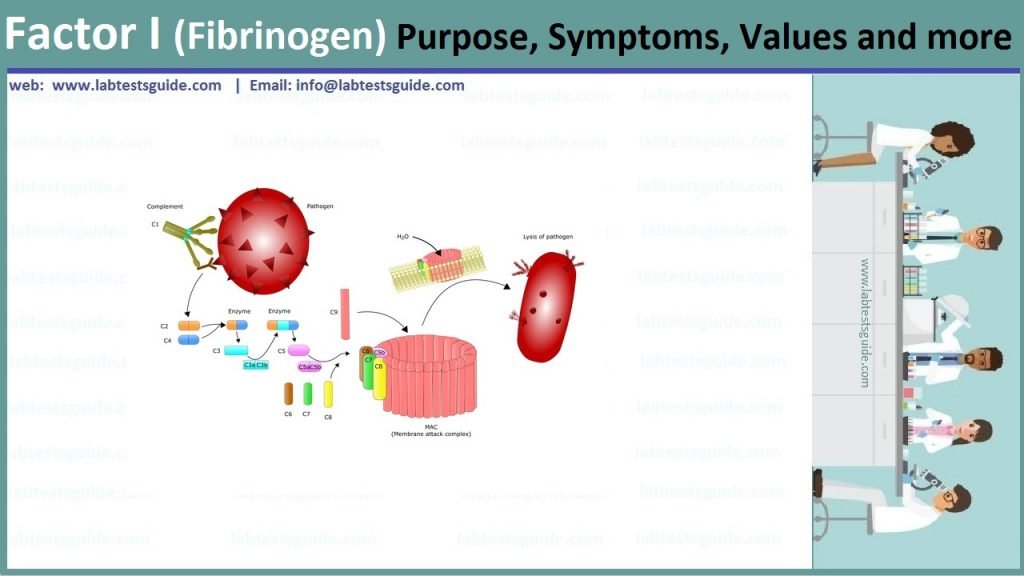
Factor I deficiency is a collective term for three rare inherited fibrinogen deficiencies. Fibrinogen helps platelets unite to form the initial “plug” after an injury. Fibrinogen deficiencies can be quantitative or qualitative, depending on whether the fibrinogen is deficient or defective. Quantitative disorders are afibrinogenemia, when fibrinogen is absent, and hypofibrinogenemia, when a protein with a normal structure is present but below the levels necessary for normal coagulation. Dysfibrinogenemia is a qualitative disorder in which the liver makes normal amounts of fibrinogen, but does not coagulate properly.
Complement factor I, also known as C3b/C4b inactivator, is a protein that in humans is encoded by the CFI gene. Complement factor I (factor I) is a protein of the complement system
Also Known as: Coagulation Fators, Factor Assays, Blood Clotting Factors, Clotting Factors, Factor I, Factor II, Factor III,Factor IV, Factor V, Factor VI, Factor VII, Factor VIII, Factor IX, Factor X, Factor XI, Factor XII,Factor XIII
Related Tests: Prothrombin Time (PT), Partial Thromboplastin Time (PTT), Fibrinogen, Activated Partial Thromboplastin Time (APTT)
Factor I (or fibrinogen) deficiency is a very rare inherited disorder with complications that vary with the severity of the disorder. It is not well known, even among health professionals. People affected by this disorder and those close to them have very little written information about it. There are three types of fibrinogen deficiency: afibrinogenemia, hypofibrinogenemia and dysibrinogenemia. This disorder affects men and women in equal numbers. In some cases it can also cause severe bleeding or thrombosis. This booklet seeks to provide information to people trying to deal with this health problem. Explain the causes of the disorder and the treatments currently available.
What is Fibrinogen:
Fibrinogen, also called Factor I, is a blood plasma protein produced by the liver that plays an important role in blood clotting. Blood coagulation is a process in which several components of the blood form a clot. When blood escapes from a rupture in a blood vessel, coagulation is triggered. Several proteins, called coagulation factors, go into action to produce thrombin. The thrombin then converts the fibrinogen into fibrin. Fibrin produced from fibrinogen is the main protein in a blood clot. It surrounds blood cells and plasma and helps form the clot. The resulting clot, which is stabilized by Factor XIII, remains intact for 10 to 14 days, the time required for healing to take place.
Types of Fibrinogen deficiency:
- Afibrinogenemia: (absence of fibrinogen):
In this type of factor I deficiency, there is a complete absence of fibrinogen. The fibrinogen level is <0.2 g/l of plasma. about 5 people out of 10 million are affected by it. of the three types, this one causes the most serious bleeding. - Hypofibrogenemia: (lower than normal level):
In this anomaly, fibrinogen is present, but at a lower level than normal, between 0.2 g/l and 0.8 g/l. This anomaly is less frequent than afibrinogenemia. Bleeding problems may be mild, moderate or severe. - Dysfibrinogenemia: (malfunctioning):
In dysfibrinogenemia, the fibrinogen level is normal, which means between 2 and 4 g/l, but the fibrinogen does not function properly. About 1 person in 1 million is affected by this condition. More than 100 different types of dysfibrinogenemia have been reported. Those affected rarely suffer from hemorrhaging problems. They may even present the opposite condition: thrombosis (blood coagulates in the blood stream). - Other types of bleeding have been described:
- bruises
- bleeding from the gums
- epistaxis (nosebleeds)
- gastrointestinal hemorrhage
- genito-urinary hemorrhage
- intra-cranial hemorrhage
- rupture of the spleen and hemorrhage in the spleen
Fibrinogen group:
Sample Required:
- The plasma is needed, take 5 ml of venous blood and add sodium citrate as the anticoagulant.
- Perform the assay immediately or as soon as possible.
- For factors II, V, VII, and X, place the citrated plasma on ice immediately, and the sample is stable for 2 hours.
- Freeze if it is delayed >2 hours.
Test Preparation Needed
No need any Preparation for this sample.
Normal Values:
- Adult = 200 to 400 mg/dL
- Newborn = 125 to 300 mg/dL
Fibrinogen Level Increased Is Seen In:
- Acute inflammatory reactions.
- Trauma.
- Coronary heart disease.
- Cigarette smoking.
Fibrinogen Decreased Level Is Seen In:
- Liver diseases like hepatitis and cirrhosis.
- DIC ( disseminated intravascular coagulopathy ).
- Fibrinolysis.
List of factors:
The table lists 13 of 20 different coagulation factors involved in the coagulation cascade that are vital to normal blood clotting.
| Coagulation Factor | Other Common Name |
|---|---|
| Factor I | Fibrinogen |
| Facto II | Prothrombin |
| Factor III | Tissue factor or thromboplastin |
| Factor IV | Calcium |
| Factor V | Proaccelerin (Labile factor) |
| Factor VI | Unassigned – old name of Factor Va |
| Factor VII | Proconvertin (Stable factor) |
| Factor VIII | Antihaemophilic factor A, Antihaemophilic globulin |
| Factor IX | Antihaemophilic factor B, Plasma thromboplastin component, Christmas factor |
| Factor X | Stuart-Prower factor |
| Factor XI | Plasma thromboplastin antecedent, Haemophilia C, Rosenthal syndrome |
| Factor XII | Hageman factor |
| Factor XIII | Fibrin stabilising factor, Laki-Lorand factor |
Normal Values:
| Factors | Normal Values |
|---|---|
| Factor I (Fibrinogen) | Adult = 200 to 400 mg/dLNewborn = 125 to 300 mg/dL |
| Factor II (Prothrombin) | 10 to 15 mg/dL |
| Factor III (Thromboplastin) | |
| Factor IV (Ionized calcium) | 4.60 to 5.08 mg/dL |
| Factor V (Labile Factor) | 5 to 10 mg/dL |
| Factor VI | Not existing |
| Factor VII (Stable factor) | 5 to 20 mg/dL |
| Factor VIII (Antihemophilic factor) | 30 mg/dL |
| Factor IX (Christmas factor) | 30 mg/dL |
| Factor X (Stuart factor) | 8 to 10 mg/dL |
| Factor XI (Plasma thromboplastin) | 25 mg/dL |
| Factor XII (Hageman factor) | |
| Factor XIII (Fibrin-stabilizing factor) | |
| Von Willebrand factor |
Diseases Leading To Coagulation Factor Deficiency:
| Disease | Factor deficiency |
|---|---|
| Disseminated intravascular coagulopathy | I, V, VIII |
| Liver diseases | I, II, V, VII, IX, X, XI |
| Autoimmune diseases | VIII |
| Congenital deficiency | I, II, V, VII, VIII, IX, X, XI, XII |
| Vit K deficiency | II, VII, IX, X, XI |
| Heparin therapy | II |
| Warfarin therapy | II, VII, IX, X, XI |
| Fibrinolysis | I, V, VIII |
Possible References Used