Effusion refers to the abnormal accumulation of fluid in a body cavity or space. This excess fluid can accumulate in various parts of the body, leading to potential health issues.

Definition of Effusion:
Effusion, in a medical context, refers to the abnormal accumulation of fluid in a body cavity or space. This excess fluid buildup can occur in various areas of the body, such as the pleural cavity around the lungs, the pericardial sac around the heart, the abdominal cavity, or within joints (synovial spaces). Effusion can result from a wide range of underlying conditions, including infections, inflammation, cancer, heart failure, liver disease, and autoimmune disorders, among others.
The accumulation of fluid can lead to swelling, pain, discomfort, and impaired organ function, depending on the affected area and the amount of fluid present. Diagnosing effusion typically involves a physical examination, medical history review, and imaging tests to visualize the fluid collection and identify the underlying cause.
Pleural Effusion:
Causes of Pleural Effusion:
Pleural effusion can be caused by various underlying conditions, including.
- Infections: Pneumonia, tuberculosis, and other lung infections can lead to pleural effusion.
- Congestive Heart Failure (CHF): Heart failure can cause fluid to back up into the lungs and pleural cavity.
- Cancer: Lung cancer, as well as cancers that spread (metastasize) to the lungs or pleura, can result in pleural effusion.
- Pulmonary Embolism: A blood clot in the lung can cause inflammation and fluid accumulation.
- Kidney Disease: Certain kidney disorders can lead to fluid retention and pleural effusion.
- Autoimmune Disorders: Conditions like rheumatoid arthritis or systemic lupus erythematosus may be associated with pleural effusion.
- Trauma: Chest injuries or surgical procedures can cause pleural effusion.
- Cirrhosis: Advanced liver disease can lead to pleural effusion due to increased pressure in the blood vessels surrounding the liver.
Symptoms of Pleural Effusion:
The symptoms of pleural effusion may vary depending on the amount of fluid and the underlying cause. Common symptoms include.
- Shortness of breath (dyspnea)
- Chest pain, especially during deep breathing or coughing
- Cough, often dry and non-productive
- Reduced chest wall movement on the affected side
- General fatigue and weakness
Diagnosis and Treatment:
- To diagnose pleural effusion, a healthcare professional may perform a physical examination, review medical history, and order imaging tests such as chest X-rays, ultrasound, CT scans, or MRI. Additional tests, such as thoracentesis (a procedure to remove fluid for analysis) or pleural biopsy, may be performed to determine the cause of the effusion.
- Treatment of pleural effusion depends on the underlying cause. It may involve addressing the primary condition, draining the accumulated fluid through thoracentesis or other drainage procedures, and using medications to alleviate symptoms or combat infections. In some cases, further interventions like pleurodesis (a procedure to prevent recurrent effusions) or surgery may be necessary.
Pericardial Effusion:
Causes of Pericardial Effusion:
Pericardial effusion can have various underlying causes, including
- Inflammation: Infections (viral, bacterial, fungal), autoimmune diseases (e.g., systemic lupus erythematosus), or radiation therapy to the chest can cause inflammation of the pericardium and lead to effusion.
- Heart Conditions: Certain heart conditions, such as myocarditis (inflammation of the heart muscle) or pericarditis (inflammation of the pericardium), can result in fluid accumulation.
- Cancer: Cancer that affects the pericardium or metastasizes to the pericardium can cause effusion.
- Kidney Failure: Chronic kidney disease can lead to fluid retention and pericardial effusion.
- Trauma: Injuries to the chest or heart surgery can cause fluid accumulation.
- Hypothyroidism: An underactive thyroid gland can be associated with pericardial effusion.
Symptoms of Pericardial Effusion:
The severity of symptoms in pericardial effusion depends on the amount of fluid accumulated and how quickly it accumulates. Some common symptoms include.
- Chest pain: Often sharp and pleuritic (worsens with breathing).
- Shortness of breath: Especially when lying flat (orthopnea) or at rest (paroxysmal nocturnal dyspnea).
- Fatigue and weakness.
- Palpitations: Sensation of irregular or rapid heartbeats.
- Cough.
- Swelling in the abdomen or legs (if caused by heart failure).
Diagnosis and Treatment:
- Diagnosing pericardial effusion involves a thorough physical examination, medical history review, and various diagnostic tests, including echocardiography (ultrasound of the heart) and electrocardiography (ECG/EKG) to assess heart function and pericardial changes.
- Treatment of pericardial effusion depends on the underlying cause and the severity of symptoms. Mild cases with no significant symptoms may not require specific treatment and may be monitored closely. However, if the effusion is large or causing symptoms, treatment options may include:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be used to reduce inflammation and fluid accumulation.
- Pericardiocentesis: This procedure involves the removal of excess fluid from the pericardial sac using a needle or catheter to relieve pressure on the heart.
- Pericardial Window: In cases where recurrent effusion is a concern, a surgical procedure called pericardial window may be performed. It involves creating a small opening in the pericardium to allow excess fluid to drain into the nearby structures.
- Pericardiectomy: In severe cases or when there’s a chronic effusion, surgical removal of part or all of the pericardium (pericardiectomy) may be necessary.
Ascites:
Causes of Ascites:
Ascites can be caused by various underlying conditions, including.
- Liver Cirrhosis: The most common cause of ascites is cirrhosis of the liver, a condition characterized by extensive scarring and damage to liver tissue due to chronic liver disease, often caused by alcohol abuse, hepatitis B or C infection, or nonalcoholic fatty liver disease (NAFLD).
- Hepatitis: Viral hepatitis, particularly chronic hepatitis B or C, can lead to liver damage and ascites.
- Heart Failure: Congestive heart failure can cause decreased blood flow through the liver and result in fluid retention in the abdomen.
- Cancer: Ascites can occur as a result of certain cancers, particularly those affecting the liver, ovaries, or peritoneal lining.
- Kidney Disease: Impaired kidney function can lead to sodium and water retention, contributing to ascites.
- Pancreatitis: Inflammation of the pancreas can lead to fluid accumulation in the abdomen.
- Infections: Certain infections, such as tuberculosis or peritonitis, can cause ascites.
- Budd-Chiari Syndrome: A condition characterized by blood clot formation in the liver’s veins, leading to liver congestion and ascites.
Symptoms of Ascites:
The symptoms of ascites can vary depending on the amount of fluid accumulated and the underlying cause. Some common signs and symptoms include.
- Abdominal swelling and distension
- Feeling of fullness or discomfort in the abdomen
- Rapid weight gain
- Shortness of breath (dyspnea)
- Swelling in the legs and ankles (peripheral edema)
- Nausea or reduced appetite
- Fatigue and weakness
Diagnosis and Treatment:
- To diagnose ascites, a healthcare professional will perform a physical examination and may use imaging tests such as ultrasound or CT scans to visualize the fluid in the abdominal cavity. Blood tests may be conducted to assess liver and kidney function and determine the underlying cause.
Treatment of ascites aims to address the underlying condition, reduce fluid accumulation, and relieve symptoms. Depending on the cause and severity, treatment options may include.
- Diuretics: Medications that promote urine output and help reduce fluid retention.
- Paracentesis: A procedure in which a needle is used to drain excess fluid from the abdomen to relieve discomfort and difficulty breathing.
- Salt Restriction: Limiting sodium intake can help reduce fluid retention.
- Albumin Infusion: In severe cases of ascites, albumin, a protein that helps maintain fluid balance, may be infused to prevent a drop in blood pressure during paracentesis.
- Treating Underlying Conditions: Managing the primary cause, such as liver disease or heart failure, is essential to prevent further fluid accumulation.
Synovial Effusion:
Causes of Synovial Effusion:
Synovial effusion can be caused by various factors, including.
- Inflammatory Conditions: Joint effusion can occur as a result of inflammatory conditions such as rheumatoid arthritis, gout, or juvenile idiopathic arthritis.
- Trauma or Injury: Sprains, strains, fractures, or other injuries to the joint can lead to inflammation and fluid accumulation.
- Infection: Bacterial or viral infections can cause synovial membrane inflammation and fluid buildup in the joint.
- Osteoarthritis: The wear and tear of joints associated with osteoarthritis can result in inflammation and effusion.
- Hemarthrosis: Bleeding into the joint space due to trauma or a bleeding disorder can cause synovial effusion.
Symptoms of Synovial Effusion:
The symptoms of synovial effusion can vary depending on the joint affected and the underlying cause. Common signs and symptoms include.
- Swelling and enlargement of the joint.
- Joint pain and tenderness.
- Stiffness and reduced range of motion.
- Warmth and redness around the joint (inflammatory effusion).
- Fever and general malaise (in the case of an infectious effusion).
Diagnosis and Treatment:
- Diagnosing synovial effusion involves a physical examination, evaluation of medical history, and imaging tests such as X-rays, ultrasound, or MRI to visualize the joint and the presence of fluid.
Treatment of synovial effusion depends on the underlying cause and the severity of symptoms. Some common treatment approaches include.
- Rest and Immobilization: Limiting the use of the affected joint can help reduce inflammation and promote healing.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce pain and inflammation.
- Aspiration: In some cases, a needle may be used to drain excess fluid from the joint (arthrocentesis) to relieve pressure and alleviate symptoms.
- Physical Therapy: Strengthening and range-of-motion exercises may be recommended to improve joint function and prevent stiffness.
- Treating Underlying Conditions: Addressing the primary cause, such as managing arthritis or infections, is essential to prevent recurrent effusion.
- Joint Injections: In certain cases, the joint may be injected with medications, such as corticosteroids or hyaluronic acid, to reduce inflammation and improve joint lubrication.
Peritoneal Effusion:
Causes of Peritoneal Effusion:
Peritoneal effusion can be caused by various underlying conditions, including.
- Liver Cirrhosis: Cirrhosis of the liver is the most common cause of peritoneal effusion. It occurs when the liver is severely scarred and its function is impaired, leading to increased pressure in the blood vessels and fluid leakage into the peritoneal cavity.
- Cancer: Certain cancers, such as liver cancer, ovarian cancer, and gastrointestinal cancers, can spread to the peritoneum and cause fluid accumulation.
- Heart Failure: Congestive heart failure can lead to fluid buildup in the abdomen due to increased pressure in the veins.
- Infections: Peritonitis, which is inflammation of the peritoneum usually caused by bacterial infections, can lead to peritoneal effusion.
- Kidney Disease: Impaired kidney function can cause fluid retention and peritoneal effusion.
- Pancreatitis: Inflammation of the pancreas can lead to fluid accumulation in the abdominal cavity.
- Hypothyroidism: An underactive thyroid gland can be associated with peritoneal effusion.
Symptoms of Peritoneal Effusion:
The symptoms of peritoneal effusion can vary depending on the amount of fluid accumulated and the underlying cause. Some common signs and symptoms include.
- Abdominal swelling and distension.
- Feeling of fullness or discomfort in the abdomen.
- Rapid weight gain.
- Shortness of breath (dyspnea) due to pressure on the diaphragm.
- Nausea or reduced appetite.
- Swelling in the legs and ankles (peripheral edema).
- Fatigue and weakness.
Diagnosis and Treatment:
- To diagnose peritoneal effusion, a healthcare professional will perform a physical examination and may use imaging tests such as ultrasound or CT scans to visualize the fluid in the abdominal cavity. Blood tests may be conducted to assess liver and kidney function and determine the underlying cause.
- Treatment of peritoneal effusion depends on the underlying cause and the severity of symptoms. Treatment options may include.
- Diuretics: Medications that promote urine output and help reduce fluid retention.
- Paracentesis: A procedure in which a needle is used to drain excess fluid from the abdomen to relieve discomfort and difficulty breathing.
- Salt Restriction: Limiting sodium intake can help reduce fluid retention.
- Treating Underlying Conditions: Managing the primary cause, such as liver disease or heart failure, is essential to prevent further fluid accumulation.
- Peritoneovenous Shunt: In some cases of recurrent or refractory ascites, a shunt may be surgically placed to divert excess fluid from the peritoneal cavity to the bloodstream.
Differential Diagnosis:
The process of differential diagnosis typically includes the following steps.
- Gathering Patient Information: The healthcare provider collects a detailed medical history, including information about the patient’s symptoms, duration, and any relevant medical conditions or family history.
- Conducting Physical Examination: The healthcare provider performs a thorough physical examination to assess the patient’s overall health, observe specific signs, and identify any abnormal findings.
- Generating a List of Possible Diagnoses: Based on the patient’s symptoms and examination findings, the healthcare provider creates a list of potential conditions that could explain the observed features.
- Prioritizing Differential Diagnoses: The provider evaluates the likelihood of each potential diagnosis and considers factors such as the patient’s age, gender, risk factors, and medical history to prioritize the most probable conditions.
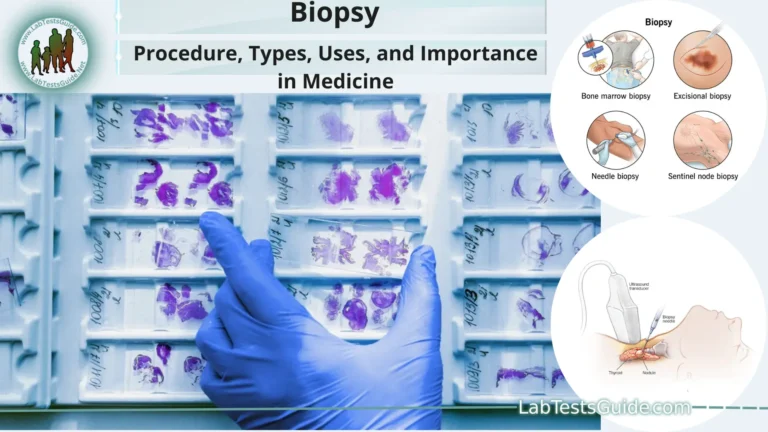
- Ordering Diagnostic Tests: To confirm or rule out the possible diagnoses, the healthcare provider may order laboratory tests, imaging studies (e.g., X-rays, ultrasound, CT scans), biopsies, or other specialized tests.
- Analyzing Test Results: The results of the diagnostic tests are interpreted in the context of the patient’s clinical presentation to help narrow down the potential diagnoses further.
- Reaching a Final Diagnosis: Based on the patient’s history, physical examination, and test results, the healthcare provider arrives at a final diagnosis—the most likely explanation for the patient’s symptoms and condition.
- Initiating Treatment: Once a definitive diagnosis is made, the appropriate treatment plan is initiated to address the underlying cause of the patient’s symptoms.
Complications and Prognosis:
Complications:
Complications are additional medical issues or adverse outcomes that can arise as a result of a primary medical condition or its treatment. They may occur due to the progression of the underlying disease, the impact of treatments, or other factors related to the patient’s overall health. Complications can vary in severity and may arise at any stage of the disease.
Some common examples of complications include.
- Infections: Patients with weakened immune systems or those undergoing immunosuppressive treatments may be more susceptible to infections.
- Organ Dysfunction: Chronic medical conditions or certain treatments can lead to impaired organ function or failure.
- Bleeding: Invasive medical procedures or certain medications can increase the risk of bleeding.
- Neurological Impairment: Conditions affecting the nervous system may lead to neurological complications, such as seizures or cognitive decline.
- Respiratory Distress: In conditions affecting the lungs or heart, respiratory complications may arise, leading to breathing difficulties.
- Wound Healing Issues: Certain medical conditions or therapies may delay or impair wound healing after surgeries or injuries.
- Side Effects of Medications: Some treatments may cause adverse reactions or side effects.
- Prognosis: Prognosis refers to the expected course and outcome of a medical condition based on various factors, including the patient’s specific diagnosis, disease progression, available treatments, and response to therapy. A favorable prognosis suggests a likelihood of recovery or improvement, while an unfavorable prognosis indicates a higher risk of complications or a poorer outcome.
Factors Affecting Prognosis:
- Stage and Severity of the Disease: The extent and severity of the disease at the time of diagnosis significantly influence the prognosis.
- Age and General Health: Overall health, age, and the presence of other medical conditions can impact a person’s ability to cope with the disease and respond to treatment.
- Treatment Options: The effectiveness of available treatments and the patient’s response to therapy play a crucial role in determining the prognosis.
- Compliance with Treatment: Adherence to prescribed treatments and lifestyle modifications can influence the overall outcome.
- Early Detection and Intervention: Early diagnosis and timely initiation of appropriate treatment can improve the chances of a positive outcome.
Prevention Strategies:
Here are some general prevention strategies.
- Healthy Diet: Maintain a balanced and nutritious diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the intake of processed foods, sugary beverages, and excessive salt and saturated fats.
- Regular Physical Activity: Engage in regular exercise to promote cardiovascular health, maintain a healthy weight, and improve overall fitness. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days per week.
- Avoid Tobacco and Limit Alcohol: Avoid smoking and exposure to secondhand smoke. If you drink alcohol, do so in moderation (up to one drink per day for women and up to two drinks per day for men).
- Vaccinations: Stay up-to-date with recommended vaccinations to protect against infectious diseases, such as influenza, pneumonia, hepatitis, and others.
- Regular Health Checkups: Schedule regular visits with a healthcare provider for preventive screenings, vaccinations, and early detection of health conditions.
- Sun Protection: Protect your skin from excessive sun exposure by wearing protective clothing, using sunscreen, and seeking shade during peak sun hours.
- Stress Management: Practice stress-reducing techniques, such as meditation, yoga, deep breathing exercises, or hobbies, to promote mental and emotional well-being.
- Safe Sex Practices: Practice safe sex to reduce the risk of sexually transmitted infections (STIs) and unintended pregnancies.
- Seat Belt and Helmet Use: Always wear a seat belt while driving or as a passenger, and use helmets when engaging in activities that pose a risk of head injuries, such as cycling or skating.
- Hygiene: Follow proper hygiene practices, including frequent handwashing, to prevent the spread of infections.
- Medication Adherence: Take prescribed medications as directed by healthcare providers, and do not skip doses or discontinue them without consulting a doctor.
- Chronic Disease Management: If you have a chronic medical condition, follow your healthcare provider’s recommendations for managing the condition, including medications, lifestyle changes, and regular checkups.
- Mental Health Awareness: Prioritize mental health and seek professional help if experiencing symptoms of anxiety, depression, or other mental health conditions.
FAQs:
What is the recommended amount of physical activity for adults?
The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days per week.
How often should I go for a regular health checkup?
It is generally recommended to have a regular health checkup at least once a year. However, the frequency may vary based on age, medical history, and risk factors. Consult with your healthcare provider for personalized advice.
What are the early signs of skin cancer?
Early signs of skin cancer may include changes in the size, shape, or color of a mole or spot, the appearance of a new growth, or a sore that does not heal. If you notice any suspicious changes on your skin, it is essential to get it checked by a dermatologist.
How can I reduce my risk of heart disease?
To reduce the risk of heart disease, focus on maintaining a healthy lifestyle. This includes adopting a balanced diet, engaging in regular physical activity, avoiding smoking, managing stress, and controlling risk factors such as high blood pressure, high cholesterol, and diabetes.
What vaccinations do adults need?
The vaccinations needed for adults may vary based on factors such as age, medical history, occupation, travel plans, and other risk factors. Common vaccinations for adults include those for influenza, tetanus, diphtheria, pertussis (Tdap), shingles, and pneumococcal disease. Consult with your healthcare provider for a personalized vaccination schedule.
How can I manage stress in my daily life?
Stress management techniques may include exercise, mindfulness practices (e.g., meditation, deep breathing), hobbies, spending time with loved ones, seeking support from friends or a counselor, and setting realistic goals and priorities.
How can I improve my sleep quality?
To improve sleep quality, maintain a consistent sleep schedule, create a relaxing bedtime routine, limit caffeine and screen time before bed, create a comfortable sleep environment, and engage in regular physical activity.
What are some healthy snack options?
Healthy snack options include fruits, vegetables with hummus or yogurt dip, nuts, seeds, whole-grain crackers with cheese, and Greek yogurt with berries.
How can I protect my skin from the sun?
To protect your skin from the sun, wear protective clothing (e.g., wide-brimmed hats, long-sleeved shirts), use sunscreen with an SPF of at least 30, seek shade during peak sun hours, and avoid tanning beds.
Conclusion:
In conclusion, maintaining a healthy lifestyle through regular physical activity, a balanced diet, and preventive healthcare measures can significantly contribute to overall well-being and reduce the risk of various medical conditions. Early detection, timely medical interventions, and adherence to prescribed treatments are crucial for managing existing health conditions and preventing potential complications. By adopting preventive strategies and making informed choices about our health, we empower ourselves to lead fulfilling lives and promote longevity and vitality. Remember to consult healthcare professionals for personalized guidance and support on your journey to optimal health.
Possible References Used