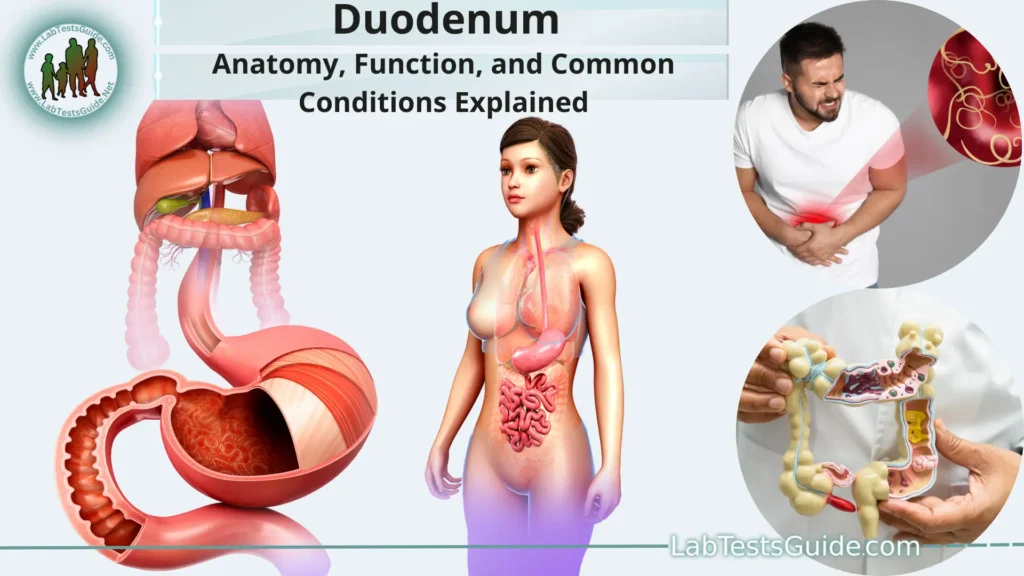
The duodenum is the first part of the small intestine, which is an essential component of the digestive system in humans and many other animals. It plays a crucial role in the digestion of food and the absorption of nutrients.
What is the Duodenum?
he duodenum is the first and shortest part of the small intestine, which is a crucial component of the digestive system in humans and many other animals. It is a C-shaped tube, approximately 25-30 centimeters (about 10-12 inches) long, and is located in the upper abdomen, just below the stomach.
Function of the Duodenum:
- Receiving and Mixing Chyme: The duodenum receives partially digested food, known as chyme, from the stomach. The chyme contains food particles, gastric juices, and stomach acid. The duodenum’s first function is to mix and regulate the flow of chyme into the small intestine, preventing overwhelming amounts from entering at once.
- Neutralization of Acidity: The stomach secretes hydrochloric acid to aid in the breakdown of food. However, this acidic chyme can be harmful to the delicate lining of the small intestine. The duodenum’s second crucial function is to neutralize the acidic chyme by releasing bicarbonate-rich mucus and receiving alkaline secretions from the pancreas. This helps maintain a slightly alkaline pH, which is more suitable for the action of digestive enzymes.
- Digestion: The duodenum plays a significant role in further breaking down the chyme into smaller, absorbable components. It receives digestive enzymes from the pancreas, which are released through the pancreatic duct. These enzymes include:
- Pancreatic Amylase: It breaks down carbohydrates (starches) into simple sugars like glucose and maltose.
- Pancreatic Lipase: It breaks down fats into fatty acids and glycerol.
Pancreatic Proteases: These enzymes (trypsin, chymotrypsin, and carboxypeptidase) break down proteins into amino acids. - Bile Emulsification: The liver produces bile, which is stored in the gallbladder and released into the duodenum through the common bile duct. Bile is essential for the digestion and absorption of fats. It emulsifies large fat globules into smaller droplets, increasing the surface area and making it easier for pancreatic lipase to break down fats into absorbable components.
- Absorption of Nutrients: While the majority of nutrient absorption occurs in the jejunum and ileum (the subsequent parts of the small intestine), the duodenum still absorbs some water-soluble products of digestion. These include simple sugars, amino acids, and certain minerals.
- Hormonal Regulation: The duodenum produces several hormones that play essential roles in regulating digestive processes. Examples include secretin, which stimulates the pancreas to release bicarbonate, and cholecystokinin (CCK), which triggers the gallbladder to release bile and the pancreas to release digestive enzymes.
Duodenal Disorders and Conditions:
Some common duodenal disorders and conditions include.
- Duodenal Ulcers: Duodenal ulcers are open sores that develop on the lining of the duodenum. They are often caused by the erosion of the protective mucus layer, allowing stomach acid to come into direct contact with the delicate lining. The most common cause of duodenal ulcers is infection with the bacterium Helicobacter pylori, but they can also result from long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs). Symptoms may include burning pain in the upper abdomen, especially between meals and at night.
- Duodenitis: Duodenitis is the inflammation of the duodenal lining, which can be caused by various factors, including H. pylori infection, excessive alcohol consumption, smoking, or certain medications. Symptoms may include abdominal pain, bloating, and discomfort.
- Duodenal Polyps: Duodenal polyps are small, non-cancerous growths that can develop on the inner lining of the duodenum. While most duodenal polyps are harmless, some larger or more numerous polyps may increase the risk of cancer development in the duodenum.
- Duodenal Obstruction: A duodenal obstruction occurs when there is a blockage or narrowing of the duodenum, which can impede the normal flow of chyme from the stomach into the small intestine. It can be caused by factors such as tumors, scar tissue, or congenital abnormalities. Symptoms may include severe abdominal pain, vomiting, and bloating.
- Celiac Disease: Celiac disease is an autoimmune disorder in which the consumption of gluten (a protein found in wheat, barley, and rye) triggers an immune response that damages the lining of the small intestine, including the duodenum. This damage can lead to malabsorption of nutrients and various gastrointestinal symptoms.
- Bile Duct Disorders: Certain conditions, such as gallstones or inflammation of the bile ducts, can impact the normal flow of bile into the duodenum. This can affect the digestion of fats and lead to symptoms like jaundice and abdominal pain.
- Zollinger-Ellison Syndrome: This is a rare condition in which tumors, called gastrinomas, form in the pancreas or duodenum and produce excessive amounts of the hormone gastrin. Gastrin stimulates the stomach to produce more acid, leading to peptic ulcers.
- Diagnosis and Treatment: The diagnosis of duodenal disorders involves a combination of medical history, physical examination, and various diagnostic tests, such as endoscopy, imaging studies, blood tests, and biopsy.
Treatment depends on the specific condition but may include:
- Medications: Antibiotics for H. pylori infection, acid-reducing medications, and other drugs to manage symptoms or underlying causes.
- Lifestyle Changes: Dietary modifications, avoiding trigger factors (e.g., smoking, alcohol), and stress management.
- Surgery: In some cases, surgical intervention may be necessary to address obstructions, remove polyps, or manage certain conditions.
Diagnosis of Duodenal Conditions:
Here are some common methods used in the diagnosis of duodenal conditions.
- Medical History and Physical Examination: The first step is to take a detailed medical history, including information about the patient’s symptoms, duration, and any relevant medical conditions. A physical examination may also be conducted to assess abdominal tenderness or other signs of potential duodenal disorders.
- Endoscopy: Upper gastrointestinal endoscopy (also known as esophagogastroduodenoscopy or EGD) is a crucial diagnostic procedure used to visualize the interior of the esophagus, stomach, and duodenum. During this procedure, a flexible tube with a camera at its tip (endoscope) is passed through the mouth and guided down the esophagus to examine the duodenum’s lining. This allows the doctor to identify any abnormalities, such as ulcers, inflammation, or polyps.
- Biopsy: During an endoscopy, the doctor may also take small tissue samples (biopsies) from the duodenal lining. These samples are then sent to a laboratory for microscopic examination to check for infection, inflammation, or signs of celiac disease.
- Imaging Studies: Various imaging techniques, such as abdominal X-rays, ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI), may be used to visualize the duodenum and surrounding structures. These can help detect obstructions, tumors, or other abnormalities.
- Blood Tests: Blood tests can provide valuable information about the overall health of the patient and may be used to check for specific markers related to duodenal conditions. For example, blood tests can help detect H. pylori infection or assess for malabsorption-related conditions like celiac disease.
- Stool Tests: Stool tests may be performed to check for the presence of blood, infections, or other signs of gastrointestinal disorders.
- Functional Tests: In some cases, functional tests may be used to assess the function of the duodenum and the digestive system as a whole. This can include tests to evaluate enzyme levels, gastric emptying, or bile flow.
- Capsule Endoscopy: In certain situations, a patient may undergo capsule endoscopy. This involves swallowing a small, disposable capsule containing a camera that takes images as it travels through the digestive tract, allowing doctors to examine the small intestine, including the duodenum.
Treatment and Management:
Here are some common approaches used to treat and manage duodenal conditions.
Medications:
- Proton Pump Inhibitors (PPIs): PPIs are commonly prescribed to reduce stomach acid production and promote the healing of duodenal ulcers and duodenitis. Examples include omeprazole, lansoprazole, and pantoprazole.
- Antibiotics: If the duodenal condition is caused by an infection with H. pylori, a course of antibiotics is typically prescribed along with acid-suppressing medications to eradicate the bacteria.
- Antacids and H2 Blockers: These medications can be used to provide short-term relief from acid-related symptoms in conditions like duodenal ulcers or gastritis.
Lifestyle Changes:
- Dietary Modifications: Avoiding spicy foods, acidic foods, caffeine, and alcohol can help alleviate symptoms in some individuals with duodenal issues.
- Quitting Smoking: For those who smoke, quitting can improve overall gastrointestinal health.
- Stress Management: Chronic stress can exacerbate symptoms, so stress reduction techniques, such as exercise, yoga, or meditation, may be beneficial.
Dietary Management:
- Gluten-Free Diet: For individuals diagnosed with celiac disease, a strict gluten-free diet is essential to manage the condition and prevent further damage to the small intestine, including the duodenum.
- Avoiding Trigger Foods: Identifying and avoiding foods that worsen symptoms can be helpful in managing certain duodenal conditions.
- Surgical Interventions: In some cases, such as severe duodenal ulcers that do not respond to medical treatment or duodenal obstructions caused by tumors or strictures, surgery may be necessary. Surgical options vary depending on the specific issue and may involve removing the affected tissue or repairing the obstruction.
- Management of Complications: Addressing complications related to duodenal disorders, such as managing bleeding from ulcers, treating infections, or correcting nutritional deficiencies caused by malabsorption.
- Follow-Up and Monitoring: Regular follow-up with a healthcare provider is essential to monitor the progress of treatment and make any necessary adjustments to the management plan.
Prevention of Duodenal Issues:
The following general guidelines can help reduce the risk of duodenal problems.
- Healthy Diet: Consume a well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
Limit the intake of spicy, fatty, and acidic foods, as well as alcohol and caffeine, which can irritate the stomach and duodenum. - Maintain a Healthy Weight: Achieve and maintain a healthy body weight through a combination of regular physical activity and a balanced diet.
Obesity can increase the risk of acid reflux and gastric issues, which may impact the duodenum. - Avoid Smoking and Alcohol: Quit smoking, as it can weaken the lower esophageal sphincter, leading to acid reflux and potential damage to the duodenum.
Limit alcohol consumption, as excessive alcohol can irritate the digestive tract. - Manage Stress: Practice stress-reducing techniques, such as mindfulness, meditation, yoga, or deep breathing exercises, as chronic stress can affect digestive health.
- Medication Use: Use nonsteroidal anti-inflammatory drugs (NSAIDs) sparingly and under the guidance of a healthcare professional. Prolonged or excessive use of NSAIDs can increase the risk of duodenal ulcers.
- Hydration: Stay well-hydrated by drinking an adequate amount of water throughout the day. Water helps maintain the appropriate balance of fluids in the digestive system.
- Screening and Early Detection: If you have a family history of gastrointestinal conditions, such as celiac disease or gastrointestinal cancers, consider regular screenings or genetic testing to identify potential risks.
- Follow Medical Advice: If you are diagnosed with a condition that affects the duodenum, such as celiac disease or H. pylori infection, follow the prescribed treatment plan and attend regular follow-up appointments.
- Food Allergies and Intolerances: If you have known food allergies or intolerances, avoid consuming trigger foods to prevent adverse reactions that can affect the digestive system.
- Promote a Healthy Gut Microbiome: Consume foods rich in probiotics (e.g., yogurt, fermented foods) to support a healthy gut microbiome, which plays a role in digestion and overall gut health.
Related Organs and Systems:
Here are some of the main related organs and systems.
- Stomach: The duodenum is directly connected to the stomach. It receives partially digested food (chyme) from the stomach, which is then further broken down and processed in the duodenum through the action of digestive enzymes and bile.
- Pancreas: The pancreas is a vital organ located behind the stomach. It plays a crucial role in digestion by producing and releasing digestive enzymes into the duodenum. These enzymes, such as amylase, lipase, and proteases, help break down carbohydrates, fats, and proteins, respectively.
- Liver and Gallbladder: The liver and gallbladder work together to produce and store bile, which is essential for the digestion of fats. The liver produces bile, and the gallbladder stores it until it is needed. When food enters the duodenum, the gallbladder releases bile through the common bile duct to aid in the digestion and absorption of fats.
- Small Intestine (Jejunum and Ileum): The duodenum is the first part of the small intestine, followed by the jejunum and ileum. Together, these three sections of the small intestine play a vital role in the absorption of nutrients from digested food. While the duodenum primarily focuses on initial digestion, the jejunum and ileum are responsible for absorbing nutrients, including vitamins, minerals, and other essential compounds.
- Esophagus: The esophagus connects the mouth to the stomach and is not directly related to the duodenum. However, it is part of the upper gastrointestinal tract and plays a critical role in transporting food to the stomach, where it will eventually enter the duodenum.
- Gastrointestinal (GI) Tract: The duodenum is part of the gastrointestinal tract, a series of organs responsible for digestion and nutrient absorption. The GI tract includes the mouth, esophagus, stomach, small intestine (duodenum, jejunum, and ileum), large intestine (colon), and rectum.
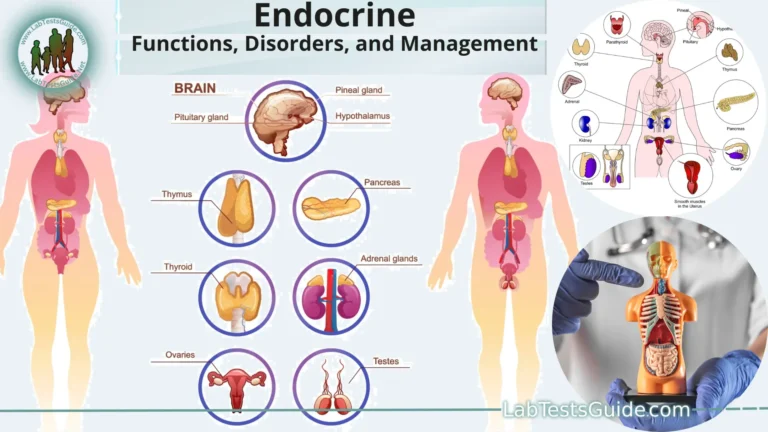
- Endocrine System: The duodenum produces various hormones that play significant roles in regulating digestive processes. For example, secretin stimulates the pancreas to release bicarbonate to neutralize stomach acid, while cholecystokinin (CCK) triggers the release of bile from the gallbladder and digestive enzymes from the pancreas.
- Cardiovascular System: The cardiovascular system plays an indirect role in supporting the duodenum’s functions by delivering oxygen and nutrients to the organs involved in digestion, including the liver, pancreas, and small intestine.
FAQs:
What is the duodenum, and what is its function?
The duodenum is the first part of the small intestine, located just below the stomach. Its primary function is to receive partially digested food from the stomach (chyme) and further digest it using enzymes from the pancreas and bile from the liver. It also neutralizes the acidity of chyme and absorbs some nutrients.
What are duodenal ulcers, and what causes them?
Duodenal ulcers are open sores that form on the duodenal lining. They are often caused by Helicobacter pylori infection or overuse of nonsteroidal anti-inflammatory drugs (NSAIDs).
Can duodenal ulcers be treated without surgery?
Yes, most duodenal ulcers can be treated with medications, including acid-reducing agents and antibiotics to eliminate H. pylori infection. Surgery is typically reserved for severe cases or complications.
Is celiac disease related to the duodenum?
Yes, celiac disease is an autoimmune disorder that affects the small intestine, including the duodenum. In celiac disease, the ingestion of gluten triggers an immune response, damaging the lining of the small intestine and impairing nutrient absorption.
What are the symptoms of duodenal issues?
Symptoms of duodenal issues may include abdominal pain or discomfort, bloating, indigestion, heartburn, nausea, vomiting, and changes in bowel movements.
How are duodenal disorders diagnosed?
Diagnosis often involves a combination of medical history, physical examination, endoscopy (EGD), imaging tests, blood tests, and biopsies of the duodenal tissue.
What lifestyle changes can help prevent duodenal issues?
Adopting a healthy diet, avoiding smoking and excessive alcohol consumption, managing stress, maintaining a healthy weight, and avoiding trigger foods can help prevent duodenal issues.
Can duodenal polyps become cancerous?
While most duodenal polyps are benign, some larger or more numerous polyps can have the potential to become cancerous. Regular monitoring and management by a healthcare professional are essential.
Can stress worsen duodenal conditions?
Yes, chronic stress can exacerbate duodenal issues and may contribute to symptoms like abdominal pain and digestive disturbances. Stress-reducing techniques can be beneficial.
How are duodenal obstructions treated?
The treatment of duodenal obstructions depends on the underlying cause. In some cases, surgery may be necessary to remove the obstruction or repair strictures.
Conclusion:
In conclusion, the duodenum is a critical component of the digestive system, serving as the first part of the small intestine responsible for receiving, digesting, and neutralizing partially digested food from the stomach. It plays a key role in breaking down nutrients through the action of pancreatic enzymes and bile, facilitating their absorption in the subsequent parts of the small intestine. While the duodenum can be affected by various disorders and conditions, early diagnosis, appropriate treatment, and healthy lifestyle choices can help maintain its optimal function and overall digestive health, ensuring the body’s efficient absorption of essential nutrients and contributing to overall well-being.
Home | Blog | About Us | Contact Us | Disclaimer
Possible References Used