Dermatitis, also known as eczema, is a common skin condition characterized by inflammation of the skin. It can cause various symptoms, such as redness, itching, swelling, and sometimes even blistering or oozing of the skin. Dermatitis can be chronic (long-lasting) or acute (short-term), and it can affect people of all ages.

Definition of Dermatitis.
Dermatitis, often referred to as eczema, is a common skin condition characterized by inflammation of the skin. It typically presents with symptoms such as redness, itching, swelling, and sometimes the formation of blisters, scales, or crusts on the affected areas of the skin. Dermatitis can occur in various forms and can affect people of all ages, ranging from infants to adults.
The inflammation associated with dermatitis is a response to irritants, allergens, or other triggers that the skin comes into contact with. These triggers can vary widely and may include substances like soaps, detergents, certain fabrics, metals, cosmetics, fragrances, and even environmental factors such as changes in temperature or humidity.
Causes and Triggers:
Here are some common causes and triggers associated with different types of dermatitis.
Atopic Dermatitis:
- Genetic Predisposition: A family history of atopic conditions like asthma, hay fever, or eczema can increase the risk.
- Immune System Dysfunction: Abnormal immune responses to irritants or allergens can contribute.
- Environmental Factors: Cold, dry weather or exposure to certain allergens can exacerbate symptoms.
Contact Dermatitis:
- Allergens: Exposure to substances like nickel, fragrances, cosmetics, latex, and plants (like poison ivy) can trigger allergic contact dermatitis.
- Irritants: Substances such as soaps, detergents, solvents, acids, and alkalis can cause irritant contact dermatitis.
Seborrheic Dermatitis:
- Malassezia Yeast: Overgrowth of the Malassezia yeast on the skin can contribute to seborrheic dermatitis.
- Hormonal Factors: Fluctuations in hormones may play a role, as it often affects infants (cradle cap) and adults (dandruff) during hormonal changes.
Nummular Dermatitis:
- Dry Skin: Dry skin can make the skin more susceptible to irritation and trigger nummular dermatitis.
- Environmental Factors: Exposure to cold, dry weather can worsen symptoms.
Stasis Dermatitis:
- Poor Circulation: Conditions that affect blood flow, like varicose veins or venous insufficiency, can lead to stasis dermatitis.
- Fluid Retention: Swelling due to fluid accumulation in the legs can contribute to its development.
Other Factors:
- Emotional Stress: Stress can exacerbate various types of dermatitis by weakening the immune response and triggering inflammation.
- Sweating: Excessive sweating, especially in skin folds, can worsen certain types of dermatitis.
- Certain Foods: In some individuals, certain foods may trigger or worsen symptoms, particularly in cases of atopic dermatiti
Common Symptoms:
Here are some of the typical symptoms.
- Redness (Erythema): Affected skin areas can become red and inflamed due to the underlying inflammation.
- Itching (Pruritus): Itching is a hallmark symptom of dermatitis. It can range from mild to severe and can be very distressing for individuals.
- Dryness: The skin in affected areas may become dry, rough, and scaly, leading to a feeling of tightness.
- Swelling (Edema): Inflammation can cause the skin to swell, leading to a puffy appearance.
- Blistering or Vesicles: Some forms of dermatitis, like allergic contact dermatitis, can lead to the development of small blisters or vesicles filled with fluid.
- Crusting and Oozing: In cases where blisters rupture, the skin can crust over or ooze clear or yellowish fluid.
- Thickened Skin (Lichenification): Chronic scratching or rubbing can lead to thickening of the skin, making it appear leathery.
- Patches or Patches of Discoloration: Depending on the type of dermatitis, you might notice patches of lighter or darker skin compared to the surrounding areas.
- Scaly Skin: Raised, flaky patches of skin can develop, especially in conditions like seborrheic dermatitis.
- Pain or Discomfort: In some cases, dermatitis can cause discomfort or even mild pain, particularly when the skin is cracked or broken.
- Secondary Infections: Scratching can create openings in the skin that make it susceptible to bacterial or fungal infections.
- Localized or Widespread: Symptoms can appear in specific areas or spread across larger portions of the body, depending on the type and severity of the dermatitis.
Diagnosis:
- Medical History: Your doctor will start by asking you about your symptoms, their duration, and any triggers or patterns you’ve noticed.
They may inquire about your personal and family history of allergies, asthma, or other skin conditions. - Physical Examination: A dermatologist will closely examine the affected areas of your skin. They will assess the appearance, distribution, and severity of the rash or symptoms.
They may ask about your scratching habits, as chronic scratching can lead to specific patterns of skin changes. - Patch Testing (if applicable): If your dermatitis is suspected to be due to contact with allergens, patch testing may be recommended. Small amounts of potential allergens are applied to your skin to determine if any cause a reaction.
- Skin Biopsy (if needed): In some cases, a small sample of skin tissue (biopsy) may be taken for examination under a microscope. This can help confirm the diagnosis and rule out other conditions.
- Blood Tests (if necessary): Blood tests may be conducted to rule out specific underlying conditions, especially if your symptoms are severe or not responding to treatment.
- Photographs: Photographs of the affected areas may be taken during your initial visit to document the appearance of the rash and its progression over time.
- Elimination Diets (if applicable): For individuals with suspected food-related triggers, an elimination diet under medical supervision may help identify potential dietary causes.
- Differential Diagnosis: Dermatitis can have similar symptoms to other skin conditions. The dermatologist will consider other possibilities and rule out conditions like psoriasis, fungal infections, and more.
Prevention:
Here are some prevention strategies you can consider.
- Identify and Avoid Triggers: If you know the substances or factors that trigger your dermatitis, take steps to avoid them. This might involve reading ingredient labels on products or making changes to your environment.
For contact dermatitis, patch testing can help identify specific allergens that cause a reaction. - Skin Care: Use mild, fragrance-free soaps and cleansers to avoid irritating the skin.
Avoid excessive bathing or use of hot water, as this can strip the skin of natural oils and worsen dryness.
After bathing, pat your skin dry gently and apply moisturizer to lock in moisture. - Moisturize Regularly: Regularly applying a hypoallergenic, fragrance-free moisturizer can help keep your skin hydrated and prevent dryness.
Choose moisturizers with ingredients like ceramides, hyaluronic acid, or petrolatum. - Choose Skin-Friendly Products: Opt for hypoallergenic and fragrance-free products, including cosmetics, lotions, detergents, and fabric softeners.
Test new products on a small patch of skin before applying them more widely. - Protective Measures: Wear protective clothing or gloves if you’re exposed to irritants or allergens at work or during activities.
Use sunscreen to protect your skin from harmful UV rays, especially if you have photosensitive dermatitis. - Stress Management: Stress can trigger or worsen dermatitis symptoms. Practice stress-reduction techniques such as deep breathing, meditation, yoga, or regular exercise.
- Diet and Hydration: Stay hydrated by drinking enough water to maintain skin moisture.
Some individuals find that certain foods can trigger flare-ups. Keeping a food diary might help identify potential triggers. - Environmental Control: Maintain a comfortable indoor environment with appropriate humidity levels, especially during dry or cold seasons.
Avoid exposure to extreme temperatures and sudden changes in weather. - Regular Checkups: Visit a dermatologist regularly to monitor your skin’s health, adjust your treatment plan as needed, and discuss any concerns.
- Proper Clothing: Choose breathable, soft fabrics like cotton to minimize skin irritation. Avoid tight clothing that can rub against the skin.
- Avoid Scratching: Scratching can worsen symptoms and even lead to skin infections. Keep your nails short and consider using gloves or covering affected areas if necessary.
Types of Dermatitis:
Here are some of the most common types of dermatitis.
Atopic Dermatitis (Eczema):
- A chronic inflammatory skin condition often associated with a family history of allergies, asthma, or hay fever.
- Commonly affects infants and young children but can persist into adulthood.
- Symptoms include intense itching, redness, dry skin, and the development of scaly or crusted patches.
Contact Dermatitis:
- Allergic Contact Dermatitis: Caused by an allergic reaction to a specific substance that comes into contact with the skin. Symptoms include redness, itching, and sometimes blisters.
- Irritant Contact Dermatitis: Results from direct irritation of the skin by substances such as soaps, detergents, chemicals, or solvents. Symptoms include redness, itching, and skin dryness.
Seborrheic Dermatitis:
- A common condition that primarily affects areas with high concentrations of oil glands, such as the scalp, face, and upper chest.
- Symptoms include greasy or scaly patches, itching, and redness. In infants, it’s known as “cradle cap.”
Nummular Dermatitis:
- Characterized by coin-shaped or oval patches of irritated, itchy skin that can ooze fluid and become crusted.
- Often associated with dry skin and may be triggered by factors like cold weather or irritants.
Stasis Dermatitis:
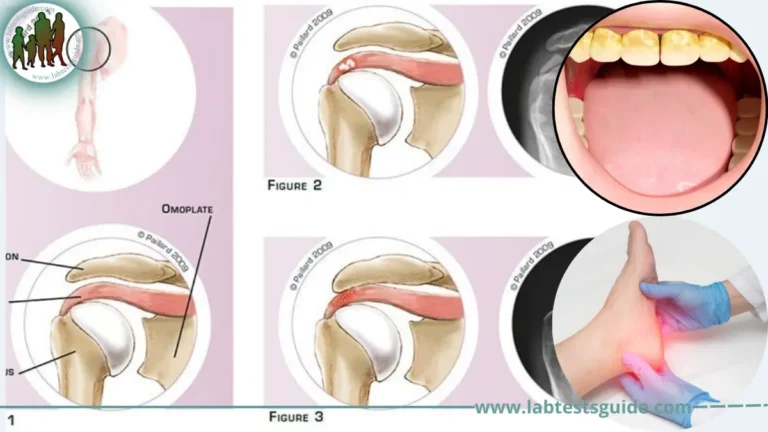
- Develops in the lower legs due to poor blood circulation, often associated with venous insufficiency or varicose veins.
- Symptoms include swelling, redness, itching, and skin changes that can progress to open sores if left untreated.
Dyshidrotic Dermatitis (Pompholyx):
- A form of eczema characterized by small, intensely itchy blisters that typically appear on the palms of the hands, sides of the fingers, and soles of the feet.
Allergic Contact Dermatitis (Other Than Plants):
- Caused by exposure to allergens like metals (e.g., nickel), fragrances, cosmetics, latex, and various chemicals.
Perioral Dermatitis:
- Primarily affects the area around the mouth (perioral region) and can resemble acne or rosacea.
- Presents with small red bumps, pustules, or papules that may be itchy or burning.
Lichen Simplex Chronicus:
- A condition where repeated scratching or rubbing of the skin leads to thickening and scaling. Often associated with underlying itchiness.
Autoimmune Dermatitis (such as Dermatitis Herpetiformis):
- Dermatitis associated with autoimmune disorders. Dermatitis herpetiformis is linked to celiac disease and presents with itchy, blistering skin lesions.
Treatment Options:
Here are some common treatment options.
- Topical Steroids: Corticosteroid creams or ointments are often prescribed to reduce inflammation, itching, and redness.
They come in varying strengths and are applied directly to the affected skin. - Topical Calcineurin Inhibitors: Non-steroidal creams, such as tacrolimus or pimecrolimus, can help manage inflammation and itching, especially in sensitive areas like the face and groin.
- Emollients (Moisturizers): Regular use of fragrance-free, hypoallergenic moisturizers helps maintain skin hydration and reduce dryness. They can also act as a protective barrier.
- Antihistamines: Over-the-counter or prescription antihistamines can help relieve itching and reduce the urge to scratch. They are particularly useful for nighttime itching.
- Wet Dressings: Soaking affected areas and then applying wet dressings or wraps with emollients can provide relief and help heal the skin.
- Avoiding Triggers: Identifying and avoiding allergens or irritants that trigger flare-ups is crucial for managing dermatitis.
- Phototherapy (Light Therapy): Controlled exposure to ultraviolet (UV) light can help reduce inflammation and itching. UVB and UVA light treatments are used under medical supervision.
- Systemic Medications: In severe cases, oral corticosteroids or immunosuppressive medications may be prescribed. These are typically used for short periods due to potential side effects.
- Biologics (for Atopic Dermatitis): Recently, biologic medications targeting specific immune pathways have been approved for moderate to severe atopic dermatitis.
- Lifestyle Modifications: Proper skin care practices, such as using mild cleansers, avoiding hot water, and gently patting the skin dry, can help prevent flare-ups.
Choosing hypoallergenic products, wearing loose-fitting clothing, and avoiding tight garments can also be helpful. - Stress Management: Practicing stress reduction techniques like deep breathing, meditation, and yoga can help reduce the impact of stress on dermatitis.
- Dietary Changes (if applicable): In cases of suspected food triggers, a healthcare provider might recommend dietary modifications.
Lifestyle Management:
Here are some lifestyle management tips for dealing with dermatitis.
- Maintain Good Skin Hygiene: Use gentle, fragrance-free cleansers and avoid harsh soaps that can strip your skin of natural oils.
Take short, lukewarm showers or baths and avoid using hot water, which can worsen dryness. - Moisturize Regularly: Apply a hypoallergenic, fragrance-free moisturizer to your skin after bathing and throughout the day to keep your skin hydrated.
- Choose Skin-Friendly Products: Use hypoallergenic, non-comedogenic, and fragrance-free cosmetics, soaps, detergents, and personal care products.
- Clothing Choices: Opt for loose-fitting, breathable clothing made from natural fibers like cotton to reduce irritation.
Avoid wearing clothing that rubs against or traps moisture on the skin. - Avoid Irritants and Allergens: Identify and avoid substances that trigger your dermatitis, whether they’re chemicals, fabrics, metals, or certain foods.
- Stay Hydrated: Drink plenty of water to maintain overall skin and body hydration.
- Stress Management: Practice stress-reduction techniques such as meditation, deep breathing, yoga, or mindfulness to help minimize stress-induced flare-ups.
- Avoid Scratching: Keep your nails short and consider using gloves or covering affected areas if scratching is a significant issue.
Gently pat or tap itchy areas instead of scratching. - Manage Environmental Factors: Maintain a comfortable indoor environment with appropriate humidity levels, especially during dry or cold seasons.
Protect your skin from extreme temperatures, wind, and sun exposure. - Nutrition and Hydration: A balanced diet rich in nutrients can contribute to overall skin health. However, there’s no specific “eczema diet.” Focus on a well-rounded diet that includes fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Regular Exercise: Regular physical activity can help improve blood circulation and overall well-being. Just be mindful of sweating and choose moisture-wicking clothing.
- Medication Adherence: If you’ve been prescribed topical medications or other treatments, follow your healthcare provider’s instructions closely.
- Monitor Your Skin: Pay attention to any changes in your skin condition, and track your symptoms over time. This can help you identify triggers and assess the effectiveness of treatments.
- Consult Professionals: Keep regular appointments with your dermatologist to discuss your progress, receive guidance, and adjust your treatment plan as needed.
When to See a Doctor:
Here are some situations when you should consider seeking medical attention.
- New or Unexplained Symptoms: If you develop new skin symptoms, such as redness, itching, rashes, or blisters, and you’re unsure about their cause.
- Persistent Symptoms: If your symptoms continue for more than a few weeks despite using over-the-counter treatments or home remedies.
- Severe Symptoms: If your symptoms are severe, causing extreme discomfort, pain, or interfering with your daily activities.
- Secondary Infections: If you notice signs of infection such as increased redness, warmth, swelling, pus, or pain at the affected site.
- Worsening Condition: If your dermatitis is getting worse or spreading to other areas of your body.
- Difficulty Managing Symptoms: If you’re struggling to manage your symptoms with over-the-counter treatments or lifestyle changes.
- Face or Genital Involvement: If dermatitis affects sensitive areas like your face or genital region, it’s advisable to consult a dermatologist for proper treatment.
- Children or Infants: If your child or infant develops skin symptoms, especially if they’re very young or if the condition seems to be causing significant discomfort.
- Existing Medical Conditions: If you have other underlying medical conditions, such as diabetes or autoimmune disorders, that may complicate your dermatitis or require specialized care.
- Uncertainty About Diagnosis: If you’re uncertain about the cause of your symptoms or have questions about the diagnosis you’ve received.
- Treatment Not Working: If the treatments you’ve been using are not providing relief or if your symptoms are not improving.
- Changes in Appearance: If your skin changes in appearance, texture, or color in a way that concerns you.
FAQs:
What is dermatitis?
Dermatitis, also known as eczema, is a common skin condition characterized by inflammation, redness, itching, and sometimes blisters or dry patches on the skin.
What causes dermatitis?
Dermatitis can be caused by various factors such as genetics, allergens, irritants, environmental conditions, stress, and underlying health conditions.
Are there different types of dermatitis?
Yes, there are several types of dermatitis, including atopic dermatitis, contact dermatitis (allergic and irritant), seborrheic dermatitis, nummular dermatitis, and more.
What are the common symptoms of dermatitis?
Common symptoms include redness, itching, dryness, swelling, blisters, scaling, and in some cases, oozing or crusting of the skin.
Can dermatitis be cured?
While there may not be a permanent cure, dermatitis can be managed effectively with proper treatment, lifestyle changes, and avoidance of triggers.
How is dermatitis diagnosed?
Diagnosis involves a medical history review, physical examination, and, in some cases, patch testing or skin biopsies to confirm the type of dermatitis.
What are the treatment options for dermatitis?
Treatment may include topical steroids, moisturizers, antihistamines, avoiding triggers, and, in severe cases, oral medications or phototherapy.
Can I prevent dermatitis flare-ups?
Yes, you can prevent flare-ups by identifying and avoiding triggers, maintaining good skin care practices, managing stress, and making lifestyle adjustments.
When should I see a doctor for dermatitis?
You should see a doctor if you have persistent or worsening symptoms, severe discomfort, signs of infection, or if your treatments aren’t working effectively.
Can dermatitis affect any age group?
Yes, dermatitis can affect people of all ages, from infants to the elderly.
Is dermatitis contagious?
No, dermatitis is not contagious. It cannot be spread from person to person through contact.
Can diet affect dermatitis?
In some cases, certain foods might trigger or worsen dermatitis symptoms, but there’s no universal “eczema diet.” Consult a healthcare professional if you suspect food triggers.
Is stress linked to dermatitis?
Yes, stress can exacerbate dermatitis symptoms. Stress management techniques can help reduce the impact of stress on the condition.
Conclusion:
In conclusion, dermatitis, also known as eczema, is a common and often chronic skin condition characterized by inflammation, redness, itching, and various skin changes. It can affect people of all ages and can significantly impact quality of life. Understanding the different types of dermatitis, their causes, symptoms, and treatment options is essential for effective management.
From atopic dermatitis to contact dermatitis, seborrheic dermatitis, and more, each type has its unique triggers and treatment approaches. Early diagnosis, proper medical guidance, and a combination of lifestyle adjustments and treatments can help alleviate symptoms, prevent flare-ups, and improve overall skin health.
Possible References Used