Connective and Mesenchymal Tissues and Their Stains 100 FAQs and 60 MCQs
Connective and Mesenchymal Tissues and Their Stains FAQs:
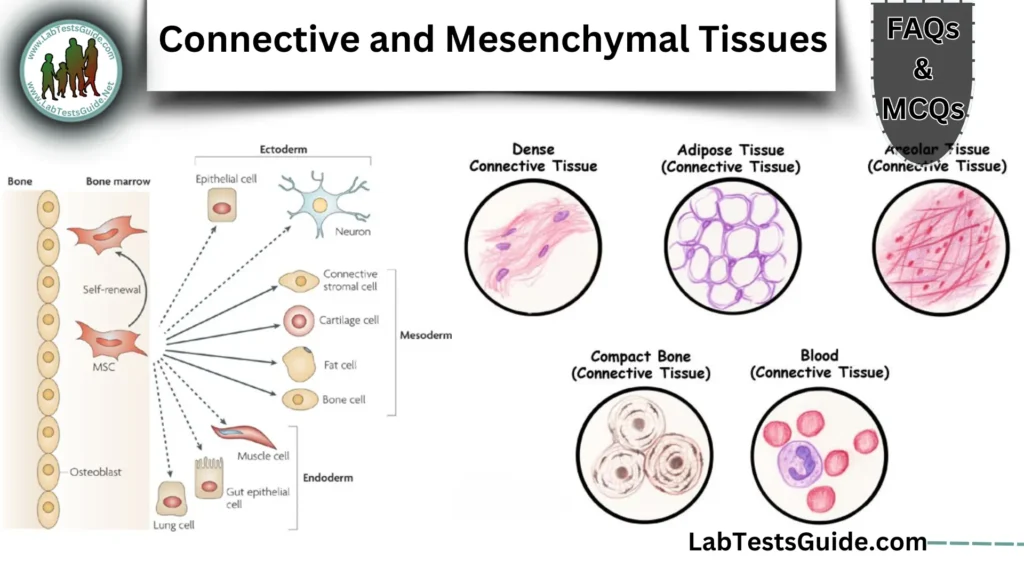
What are the four main types of connective tissue?
Four main connective tissues: Connective tissue proper (loose/dense), cartilage, bone, blood.
What embryonic layer gives rise to connective tissues?
Embryonic origin: Mesoderm (mesenchyme).
What are the three main components of connective tissue?
Components: Cells, fibers (collagen/elastic/reticular), ground substance.
How does the function of bone differ from that of blood?
Bone vs. blood: Bone provides structural support; blood transports nutrients/gases.
What is the role of fibroblasts in connective tissue?
Fibroblasts: Synthesize collagen and ground substance; repair tissues.
Why is adipose tissue classified under connective tissue?
Adipose classification: Mesenchymal origin, embedded in ECM with reticular fibers.
What distinguishes “connective tissue proper” from other connective tissue types?
Connective tissue proper: Excludes specialized types (bone/blood); includes loose/dense tissues.
What is the amorphous ground substance composed of?
Ground substance: Glycosaminoglycans (e.g., hyaluronic acid), proteoglycans, glycoproteins.
How does the cellular-to-matrix ratio vary in different connective tissues?
Cellular-to-matrix: Bone (low cells, high matrix); blood (high cells, low matrix).
What are the primary functions of connective tissue?
Functions: Support, binding, protection, transport, storage.
What are the four major types of collagen?
Collagen types: I (bone/skin), II (cartilage), III (reticular), IV (basement membranes).
Which collagen type forms thick fibers in bone and skin?
Type I collagen: Forms thick, strong bundles in bone and skin.
How does Type III collagen differ from Type I?
Type III vs. I: Type III forms fine reticular networks; Type I forms dense fibers.
Why are reticular fibers argyrophilic?
Argyrophilic reticular fibers: Carbohydrate-rich proteoglycans bind silver stains.
What staining methods differentiate collagen from reticular fibers?
Staining differentiation: Silver impregnation (reticular); trichrome (collagen).
What is the role of Type IV collagen in basement membranes?
Type IV collagen: Creates mesh-like basement membranes for filtration/support.
How do collagen fibers appear under polarized light?
Collagen under polarization: Birefringent (Type I bright; Type III faint).
What causes the periodic banding pattern in collagen fibrils?
Banding pattern: Staggered collagen molecules create 64 nm repeating bands.
How does aging affect collagen structure?
Aging collagen: Increased cross-linking reduces flexibility, causing stiffness.
What is thesignificance of pN collagen III in fibril formation?
pN collagen III: Controls Type I fibril size during development.
What are the two main components of elastic fibers?
Elastic fibers: Elastin (core) + microfibrils (e.g., fibrillin).
How do oxytalan and elaunin fibers differ from mature elastic fibers?
Oxytalan/elaunin: Oxytalan (microfibrils only); elaunin (partial elastin).
What staining techniques are used for elastic fibers?
Elastic stains: Verhöeff’s, orcein, aldehyde fuchsin, Weigert’s resorcin-fuchsin.
Why does Verhöeff’s hematoxylin require differentiation with ferric chloride?
Verhöeff differentiation: Ferric chloride removes excess stain, isolating elastic fibers.
How does aldehyde fuchsin stain elastic fibers?
Aldehyde fuchsin: Stains oxidized elastin’s sulfonic acid groups (purple).
What biochemical changes occur in elastic fibers with aging?
Aging elastin: Fragmentation, calcification, loss of elasticity (e.g., wrinkled skin).
What is the role of desmosine in elastin cross-linking?
Desmosine: Cross-links elastin polypeptides, enabling stretch-recoil.
Why are elastic fibers congophilic?
Congophilic: Binds Congo red due to beta-sheet structures (green birefringence).
How do fenestrae in arterial elastic laminae function?
Fenestrae: Pores in arterial elastic laminae for nutrient diffusion.
What is the clinical significance of elastin degradation in emphysema?
Emphysema: Elastin degradation in alveoli reduces lung elasticity.
What proteins are reticular fibers primarily composed of?
Reticular fibers: Type III collagen + proteoglycans (e.g., decorin).
Why are silver impregnation methods preferred for reticular fiber visualization?
Silver methods: Highlight carbohydrate-rich reticular fibers with high contrast.
How does Gordon & Sweets’ method work?
Oxidation: Potassium permanganate oxidizes fibers.
Sensitization: Ferric ammonium sulfate acts as a mordant.
Silver impregnation: Silver nitrate binds to glycoproteins.
Reduction: Formalin reduces silver to metallic deposits.
Toning/clearing: Gold chloride and sodium thiosulfate enhance contrast.
Result: Reticular fibers appear black; collagen remains unstained.What is the role of potassium permanganate in reticular fiber staining?
Role of potassium permanganate: Acts as an oxidizing agent to expose carbohydrate-rich regions of reticular fibers, enhancing silver ion binding during staining.
How do reticular fibers support organs like the liver and spleen?
Support in liver/spleen: Forms a flexible 3D network that supports parenchymal cells while allowing nutrient diffusion and immune cell movement.
What causes reticular fibers to stain black in silver methods?
Black staining in silver methods: Silver ions bind to proteoglycans on reticular fibers, reduced to metallic silver (black precipitate).
Why are reticular fibers PAS-positive?
PAS-positive: Due to carbohydrate-rich glycosaminoglycans in their proteoglycan coating.
How does fixation affect reticular fiber staining?
ixation effects: Mercury-based fixatives may mask carbohydrates; formalin preserves structure for optimal staining.
What is the relationship between reticular fibers and Type III collagen?
Relationship with Type III collagen: Reticular fibers are primarily composed of Type III collagen.
Can trichrome stains reliably differentiate reticular fibers?
Trichrome reliability: No—trichrome stains (e.g., Masson’s) poorly differentiate reticular fibers; silver impregnation is superior.
What are the three layers of basement membranes?
Lamina lucida (epithelial cell adhesion).
Lamina densa (Type IV collagen/laminin meshwork).
Lamina reticularis (anchoring collagen VII to connective tissue).How is the glomerular basement membrane (GBM) structurally unique?
GBM uniqueness: Thicker lamina densa with specialized filtration slits; critical for kidney function.
Why does the periodic acid-methenamine silver method stain basement membranes?
Periodic acid-methenamine silver: Oxidizes carbohydrates to aldehydes, which reduce silver ions, highlighting basement membranes.
What glycoproteins are abundant in the lamina densa?
Lamina densa glycoproteins: Laminin and fibronectin (mediate cell adhesion and signaling).
How does diabetes affect basement membrane thickness?
Diabetes effect: Hyperglycemia thickens basement membranes (e.g., glomeruli), impairing filtration (diabetic nephropathy).
Why are basement membranes PAS-positive?
PAS-positive: High carbohydrate content from glycoproteins (e.g., laminin) and proteoglycans.
What is the role of laminin in basement membranes?
Laminin’s role: Binds epithelial cells to the basement membrane via integrins and collagen IV.
How does the lamina reticularis connect to underlying connective tissue?
Lamina reticularis connection: Contains anchoring fibrils (Type VII collagen) linking to underlying collagen I/III.
What staining artifacts can occur in basement membrane visualization?
Staining artifacts: Overstaining (false thickness), uneven silver deposition, or incomplete oxidation (patchy PAS).
How do autoimmune diseases target basement membrane components?
Goodpasture’s syndrome: Anti-Type IV collagen antibodies attack GBM.
Alport syndrome: Genetic defects in collagen IV disrupt basement membrane integrity.What proteins enable muscle contraction?
Actin (thin filaments) and myosin (thick filaments) are the primary proteins.
Troponin and tropomyosin regulate the interaction by controlling calcium-dependent contraction.How do the striations in skeletal muscle arise?
Result from the organized arrangement of A-bands (dark, myosin-rich) and I-bands (light, actin-rich).
Z-lines (anchor actin) and M-lines (anchor myosin) create repeating sarcomere units.What distinguishes cardiac muscle from skeletal muscle?
Cardiac: Involuntary, branched cells with intercalated discs, single nucleus, and rhythmic contractions.
Skeletal: Voluntary, unbranched multinucleated cells, no intercalated discs, and fast, forceful contractions.What are intercalated discs, and how do they appear histologically?
Function: Facilitate electrical and mechanical coupling between cardiac cells.
Histological appearance: Dark, step-like lines visible with H&E staining, containing gap junctions (communication) and desmosomes (structural adhesion).How does smooth muscle differ structurally from striated muscle?
Smooth: Non-striated, spindle-shaped cells with a single nucleus; contractions are slow, involuntary, and sustained.
Striated (skeletal/cardiac): Striations from sarcomeres; rapid, voluntary (skeletal) or rhythmic (cardiac) contractions.What staining methods highlight muscle striations?
H&E: Basic visualization of striations.
Phosphotungstic Acid Hematoxylin (PTAH): Enhances A-bands and Z-lines.
Masson’s trichrome: Differentiates muscle (red) from collagen (blue).Why is phosphotungstic acid hematoxylin (PTAH) used for muscle?
Binds to myosin and troponin, highlighting cross-striations and mitochondrial bands. Ideal for diagnosing myopathies and infarcts.
How does fixation affect muscle fiber staining?
Over-fixation (e.g., prolonged formalin): Hardens tissue, reducing stain penetration and clarity.
Optimal fixation: Preserves sarcomere structure for clear striation visualization.What is the role of the sarcoplasmic reticulum in muscle cells?
Stores and releases calcium ions to initiate contraction via actin-myosin interaction.
Forms a network around myofibrils, regulating excitation-contraction coupling.How do Z-lines and H-bands relate to sarcomere structure?
Z-lines: Anchor actin filaments; define sarcomere boundaries.
H-band: Central region of the A-band containing myosin only (visible during relaxation).
Sarcomere structure: Z-line → I-band → A-band (with H-band) → M-line → next Z-line.What is the principle behind trichrome staining?
Utilizes multiple dyes of varying molecular sizes and affinities to differentially stain tissue components. Smaller dyes (e.g., Biebrich scarlet) penetrate muscle/cytoplasm, while larger dyes (e.g., aniline blue) bind collagen. Acidic pH enhances selectivity for basic tissue elements.
How do dye molecular sizes influence trichrome results?
Smaller dyes stain cellular components (muscle, cytoplasm), while larger dyes are restricted to extracellular fibers (collagen). Size exclusion ensures structural differentiation.
Why are phosphotungstic acid (PTA) and phosphomolybdic acid (PMA) used in trichrome methods?
Role of PTA/PMA in trichrome:
Act as mordants to block non-collagen structures, enhancing contrast. They selectively bind to muscle/cytoplasm, allowing collagen to retain larger dyes.What fixatives optimize trichrome staining?
Optimal fixatives:
Zenker’s, Bouin’s, or formal mercury. Avoid prolonged formalin fixation (masks dye-binding sites via cross-linking).How does pH affect dye penetration in connective tissue stains?
pH effect on dye penetration:
Acidic pH (1.5–3.0) promotes binding of acid dyes to cationic groups in collagen. Adjusting pH controls dye-tissue affinity.What is the role of picric acid in van Gieson’s stain?
Picric acid in van Gieson’s stain:
Provides yellow counterstain for non-collagen structures (muscle, RBCs) while acid fuchsin stains collagen red. Acts as a differentiating agent.Why does prolonged formaldehyde fixation impair trichrome results?
Prolonged formaldehyde impairment:
Over-cross-linking masks reactive groups, reducing dye penetration. Pre-treatment with picric acid or mercury-based fixatives restores staining.How does the MSB method differentiate fibrin of varying ages?
MSB method fibrin differentiation:
1. Martius yellow: Young fibrin (yellow).
2. Brilliant crystal scarlet: Mature fibrin (red).
3. Methyl blue: Old fibrin/organized collagen (blue).
Phosphotungstic acid removes excess dye, isolating fibrin stages.What counterstains are compatible with elastic fiber stains?
Compatible elastic fiber counterstains:
Van Gieson (collagen red), eosin (cytoplasm pink), or nuclear fast red (nuclei). Avoid overlapping colors with elastic fiber stains (e.g., black).How does microwave heating enhance methenamine silver staining?
Microwave enhancement in methenamine silver:
Accelerates silver reduction via controlled heating, ensuring uniform staining. Reduces time and prevents overstaining.What are the steps in the Masson trichrome protocol?
Masson trichrome protocol steps:
1. Deparaffinize and hydrate.
2. Stain nuclei (hematoxylin).
3. Differentiate (acid alcohol).
4. Stain cytoplasm/muscle (Biebrich scarlet).
5. Treat with PTA/PMA.
6. Stain collagen (aniline blue).
7. Dehydrate, clear, mount.How does Weigert’s resorcin-fuchsin stain elastic fibers?
Weigert’s resorcin-fuchsin for elastin:
Resorcin-fuchsin binds elastin under acidic conditions. Differentiation with alcohol removes excess dye, leaving elastic fibers blue-black.What results does the Movat pentachrome stain produce?
Movat pentachrome results:
> Collagen: Yellow.
> Elastin: Black.
> Mucins/GAGs: Blue.
> Muscle: Red.
> Fibrin: Bright red.How does the Verhöeff method differentiate elastic fibers?
Verhöeff method differentiation:
Iron hematoxylin stains elastin black. Ferric chloride removes excess dye from collagen/nuclei, isolating elastic fibers.What is the purpose of iodine in the Gordon & Sweets’ silver method?
Iodine in Gordon & Sweets’ silver:
Acts as a mordant, oxidizing reticular fiber carbohydrates to enhance silver binding. Pre-stain oxidation step.How does alcian blue function in the Movat stain?
Alcian blue in Movat stain:
Stains acidic mucopolysaccharides (e.g., GAGs) blue at pH 2.5. Highlights ground substance in cartilage/mucous membranes.Why is gold toning used in silver impregnation techniques?
Gold toning in silver techniques:
Replaces unbound silver with gold, reducing background and stabilizing stains. Enhances contrast (black → gray-black).What distinguishes the Lendrum MSB method from standard trichromes?
Lendrum MSB vs. trichromes:
Specialized for fibrin age differentiation (yellow→red→blue), unlike standard trichromes that focus on collagen/muscle.How does the periodic acid-Schiff (PAS) reaction work for basement membranes?
PAS reaction for basement membranes:
Oxidizes glycoprotein carbohydrates to aldehydes, which react with Schiff reagent to form magenta complexes.What steps prevent overstaining in the methenamine silver method?
Preventing overstaining in methenamine silver:
Controlled microwave heating.
Timed silver exposure.
Gold toning and sodium thiosulfate rinsing to remove excess silver.Why might collagen stain inconsistently in trichrome methods?
Collagen inconsistency in trichrome: Fixation issues (over/under-fixation), incorrect pH, expired dyes, or uneven sectioning.
How can mercury pigment interfere with staining, and how is it removed?
Mercury pigment interference: Forms black deposits; remove with iodine-thiosulfate treatment.
What causes excessive background staining in silver impregnation?
Excessive silver background: Overexposure, poor rinsing, or old reagents. Fix with timed steps and fresh solutions.
How does decalcification affect bone staining?
Decalcification effect: Acid damages collagen; use EDTA and extend staining.
Why do elastic fibers sometimes fail to stain with orcein?
Orcein failure: Old dye or lack of oxidation. Pre-treat with Lugol’s iodine.
How can over-differentiation in Verhöeff’s method be avoided?
Avoid over-differentiation: Monitor microscopically; use weaker ferric chloride (1%).
What causes fading in aldehyde fuchsin-stained slides?
Aldehyde fuchsin fading: Light exposure/acidic media. Store in dark with neutral mountant.
How does tissue thickness impact reticular fiber visualization?
Tissue thickness: Thick sections (>5 µm) obscure fibers. Use 2–3 µm slices.
Why are frozen sections less common in connective tissue staining?
Frozen sections: Ice crystals disrupt ECM; paraffin preserves structure.
How do fixatives containing chromium salts affect elastic fiber stains?
Chromium fixatives: Reduce elastin staining. Use formalin or prolong staining.
How does fibrin differ from fibrinoid histochemically?
Fibrin vs. fibrinoid: Fibrin (red/MSB); fibrinoid (bright red/magenta, immune complexes).
What staining features distinguish amyloid from collagen?
Amyloid vs. collagen: Amyloid (Congo red+/green birefringence); collagen (trichrome+/PAS+).
How are connective tissue stains used in diagnosing lupus nephritis?
Lupus nephritis: Thickened glomerular basement membranes (PAS/silver stains show “wire loops”).
Why is the Movat stain valuable in cardiovascular pathology?
Movat in CV: Highlights elastin (black), collagen (yellow), mucins (blue) for arterial damage.
What histological changes occur in Marfan syndrome?
Marfan syndrome: Fragmented aortic elastic fibers (Verhöeff’s stain); FBN1 mutation.
How does scurvy affect collagen synthesis?
Scurvy: Vitamin C deficiency → unstable collagen (poor staining, bleeding gums).
What staining patterns indicate necrotizing vasculitis?
Necrotizing vasculitis: Fibrinoid necrosis (trichrome red), disrupted elastin.
How are elastic fiber defects linked to aortic aneurysms?
Aortic aneurysms: Elastin loss → weakened walls (gaps in elastin stains).
Why is reticulin staining important in liver biopsies?
Reticulin in liver: Silver stain shows fibrosis (cirrhosis) or HCC architecture.
How do connective tissue stains aid in tumor classification?
Tumor classification:
> Sarcomas: Trichrome+ collagen stroma.
> Carcinomas: Epithelial clusters without collagen.
> Amyloidomas: Congo red+.
Connective and Mesenchymal Tissues and Their Stains 60 MCQs:
Possible References Used