“Chronic” is an adjective that describes a long-lasting condition or situation, often one that persists for an extended period of time or is recurrent. It is commonly used in the context of health and medical conditions, such as chronic pain, chronic illness, or chronic fatigue syndrome. In medicine, a chronic condition is typically one that lasts for three months or more.
Definition of Chronic.
Chronic” is an adjective used to describe a condition, situation, or disease that persists or continues for an extended and often indefinite period of time. It is characterized by its long-lasting, ongoing, and recurrent nature.
In a medical context, a chronic condition is generally one that lasts for three months or more. Chronic conditions can include diseases, illnesses, or health issues like diabetes, hypertension, arthritis, and asthma, among others. These conditions typically require ongoing management, treatment, or care to maintain a person’s quality of life.
Types of Chronic Conditions:
Here are some common categories of chronic conditions.
Chronic Diseases:
- Cardiovascular Conditions: This includes conditions such as coronary artery disease, congestive heart failure, and hypertension.
- Respiratory Conditions: Chronic obstructive pulmonary disease (COPD) and asthma fall under this category.
- Metabolic Conditions: Diabetes mellitus (Type 1 and Type 2) is a common chronic metabolic condition.
- Neurological Conditions: Conditions like Alzheimer’s disease and Parkinson’s disease are characterized by ongoing degeneration of the nervous system.
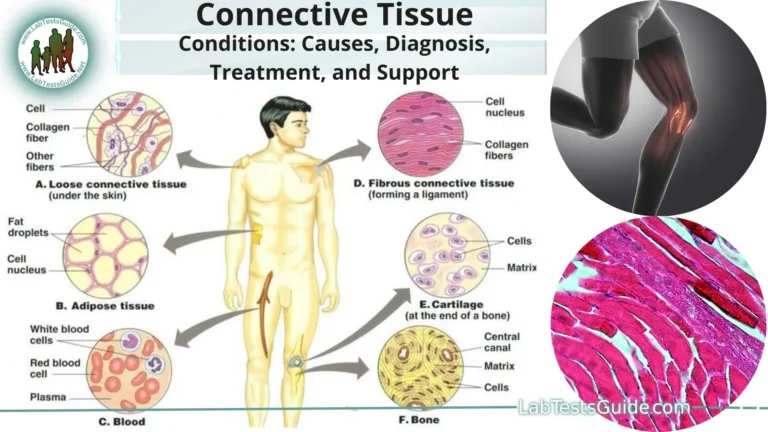
- Autoimmune Conditions: Rheumatoid arthritis, lupus, and multiple sclerosis are examples of autoimmune diseases.
- Gastrointestinal Conditions: Irritable bowel syndrome (IBS) and Crohn’s disease are examples of chronic digestive disorders.
Chronic Pain Conditions:
- Chronic Back Pain: Conditions like herniated discs or spinal stenosis can lead to ongoing back pain.
- Fibromyalgia: Characterized by widespread musculoskeletal pain and tenderness.
- Chronic Headaches: Migraines and tension-type headaches can become chronic in nature.
Chronic Infectious Diseases:
- HIV/AIDS: The human immunodeficiency virus (HIV) can lead to a chronic and progressive illness if left untreated.
- Hepatitis C: Chronic hepatitis C infection can lead to liver damage over time.
Mental Health Conditions:
- Depression: Ongoing and persistent feelings of sadness and hopelessness.
- Anxiety Disorders: Conditions like generalized anxiety disorder or panic disorder can be chronic.
- Schizophrenia: A severe and chronic mental disorder that affects thinking, feeling, and behavior.
Chronic Skin Conditions:
- Psoriasis: A skin condition characterized by red, itchy, and scaly patches.
- Eczema: Also known as atopic dermatitis, it leads to ongoing skin inflammation and itching.
Chronic Autoinflammatory Conditions:
- Rheumatoid Arthritis: An autoimmune disease affecting the joints.
- Lupus: An autoimmune condition that can affect various organs and systems in the body.
- Chronic Kidney Disease: The progressive loss of kidney function over time.
Chronic Eye Conditions:
- Glaucoma: A group of eye conditions that can lead to vision loss.
- Age-Related Macular Degeneration: An eye disease that causes vision loss in older adults.
Chronic Respiratory Conditions:
- Chronic Obstructive Pulmonary Disease (COPD): A group of lung diseases that obstruct airflow.
Chronic Infectious Diseases:
- Tuberculosis (TB): TB can become chronic if not treated effectively.
- Lyme Disease: Some individuals may experience ongoing symptoms if Lyme disease is not treated promptly.
Causes and Risk Factors:
Here are some general causes and risk factors associated with chronic conditions.
- Genetics: Family history and genetic factors can predispose individuals to certain chronic conditions. Some conditions have a strong genetic component, such as certain types of cancer and hereditary disorders like cystic fibrosis.
Lifestyle Factors:
Unhealthy lifestyle choices can significantly contribute to the development of chronic conditions. These factors include.
- Diet: A diet high in processed foods, saturated fats, and sugary beverages can lead to conditions like obesity, diabetes, and cardiovascular diseases.
- Physical Inactivity: Lack of regular exercise can contribute to obesity and increase the risk of heart disease and other chronic conditions.
- Smoking: Tobacco use is a major risk factor for lung cancer, chronic obstructive pulmonary disease (COPD), and cardiovascular disease.
- Excessive Alcohol Consumption: Heavy drinking can lead to liver disease, certain cancers, and cardiovascular problems.
- Substance Abuse: Illicit drug use can lead to chronic health issues, including addiction, mental health disorders, and infectious diseases like HIV/AIDS.
- Environmental Factors: Exposure to environmental toxins, pollutants, and contaminants can increase the risk of certain chronic conditions. For example, prolonged exposure to asbestos can lead to mesothelioma, and exposure to air pollutants can exacerbate respiratory conditions.
- Infections: Some infections, if left untreated or not managed properly, can become chronic. For example, untreated or inadequately treated sexually transmitted infections (STIs) can lead to chronic health problems.
- Age: Aging is a risk factor for many chronic conditions. Conditions like osteoarthritis and age-related macular degeneration become more common as people grow older.
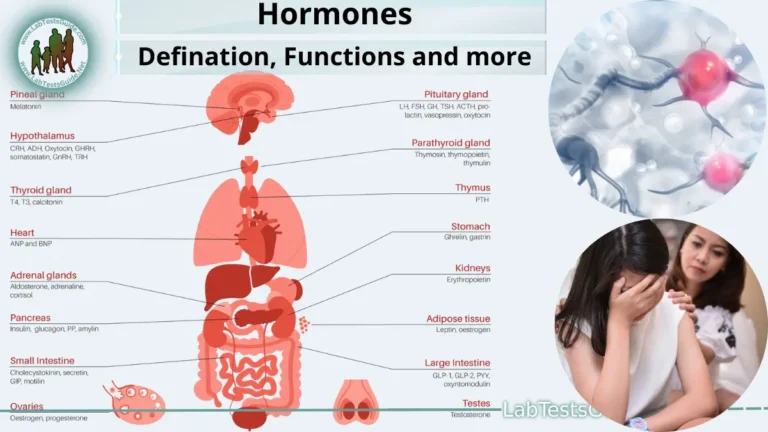
- Hormonal Changes: Hormonal changes in women, such as those that occur during menopause, can increase the risk of osteoporosis.
- Obesity: Obesity is a major risk factor for several chronic conditions, including type 2 diabetes, heart disease, and certain cancers.
- Chronic Stress: Prolonged exposure to stress can have negative effects on physical and mental health, potentially contributing to chronic conditions like hypertension, depression, and anxiety disorders.
- Immunosuppression: Conditions or treatments that weaken the immune system, such as HIV infection or immunosuppressive medications, can increase the risk of chronic infections and certain cancers.
- Hereditary and Congenital Factors: Some individuals are born with genetic conditions or structural abnormalities that predispose them to chronic conditions. For example, congenital heart defects can lead to lifelong cardiovascular issues.
- Poor Access to Healthcare: Limited access to healthcare, including preventive care and early intervention, can result in undiagnosed or poorly managed chronic conditions.
Diagnosis and Management:
Here are some general principles and steps involved in the diagnosis and management of chronic conditions.
Diagnosis:
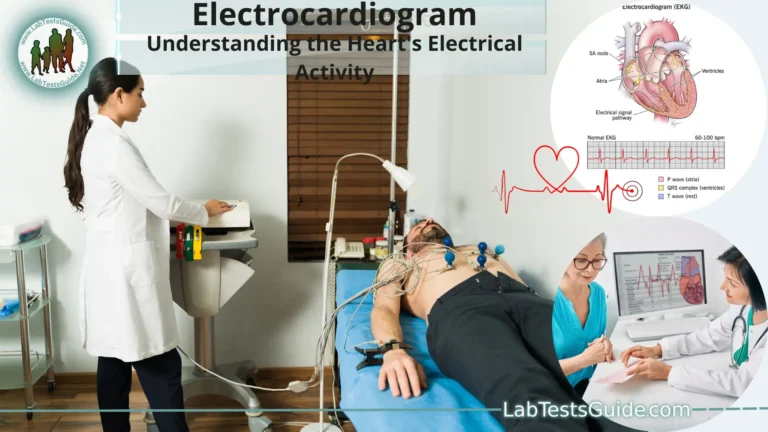
- Medical Evaluation: A healthcare provider typically begins the diagnosis process by conducting a thorough medical evaluation, which may include a review of the patient’s medical history, a physical examination, and discussions about symptoms and family history.
- Diagnostic Tests: Depending on the suspected condition, various diagnostic tests may be ordered, such as blood tests, imaging studies (like X-rays or MRI scans), biopsies, or other specialized tests.
- Symptom Assessment: Understanding the symptoms and their duration is critical in diagnosing chronic conditions. Symptoms are often monitored over time to establish the chronic nature of the condition.
- Medical Imaging: For conditions affecting the organs or body structures, medical imaging, such as CT scans, MRIs, or ultrasound, may be used to visualize and diagnose the condition.
- Biopsy: In some cases, a biopsy may be required to examine tissue samples for signs of chronic diseases like cancer.
Treatment and Management:
- Medications: Many chronic conditions are managed with medication. The type of medication prescribed depends on the condition. For example, insulin for diabetes, pain relievers for chronic pain, or immunosuppressants for autoimmune diseases.
- Lifestyle Modifications: Lifestyle changes are often essential for managing chronic conditions. This can include dietary modifications, regular exercise, stress reduction, smoking cessation, and weight management. These changes are especially important for conditions like heart disease, diabetes, and obesity.
- Therapies: Depending on the condition, therapies like physical therapy, occupational therapy, speech therapy, and cognitive-behavioral therapy may be beneficial in managing symptoms and improving quality of life.
- Surgery: In some cases, surgery may be necessary to treat or manage chronic conditions. For example, joint replacement surgery for chronic joint pain or cancer surgery to remove tumors.
- Supportive Care: Managing chronic conditions often involves supportive care, such as pain management, symptom control, and maintaining the best possible quality of life for the patient. This is especially important in conditions like advanced cancer or end-stage kidney disease.
- Regular Follow-Up: Patients with chronic conditions typically require regular follow-up with healthcare providers. These visits help monitor the condition’s progress, adjust treatment plans as necessary, and provide education and support.
- Disease-Specific Management Plans: Some chronic conditions have specific management plans and guidelines. For instance, diabetes management may involve monitoring blood sugar levels, adjusting insulin doses, and following a diabetic diet.
- Patient Education: Educating patients about their condition is crucial. This includes understanding the condition, its progression, and the importance of adhering to treatment plans. Patient engagement and self-management are often key components of managing chronic conditions.
- Support Networks: Many chronic conditions have support networks or patient advocacy groups that can provide information, resources, and emotional support to individuals and their families.
- Mental Health Support: Managing the emotional and psychological aspects of chronic conditions is important. Mental health support can include counseling, therapy, and medication when needed.
Prevention and Public Health:
Here are some key aspects of prevention and public health related to chronic conditions.
Primary Prevention:
Primary prevention strategies focus on preventing chronic conditions from developing in the first place. These strategies include.
- Health Education: Raising awareness about healthy lifestyle choices, risk factors, and the importance of regular check-ups can help individuals make informed decisions.
- Promoting Healthy Lifestyles: Encouraging healthy behaviors such as maintaining a balanced diet, regular physical activity, avoiding tobacco and excessive alcohol use, and practicing safe sex can reduce the risk of many chronic conditions.
- Vaccination: Immunizations can prevent certain infectious diseases that may lead to chronic conditions, such as hepatitis B or human papillomavirus (HPV) vaccines to prevent liver and cervical cancer.
- Screening and Early Detection: Regular screenings and health checks can identify risk factors and early signs of chronic diseases, allowing for timely intervention.
- Environmental Interventions: Public health policies and regulations can address environmental factors that contribute to chronic conditions, such as clean air and water regulations and workplace safety standards.
Secondary Prevention:
Secondary prevention focuses on early detection and management of chronic conditions to prevent complications.
- Regular Health Check-ups: Encouraging individuals to visit healthcare providers for routine check-ups, screenings, and monitoring of health parameters.
- Screening Programs: Public health initiatives that provide screenings for conditions like hypertension, diabetes, and certain cancers can help identify cases early.
- Education for Healthcare Providers: Ensuring that healthcare providers are aware of the latest guidelines for early detection and management of chronic conditions is essential.
Tertiary Prevention:
Tertiary prevention aims to prevent the progression of chronic conditions, reduce complications, and improve quality of life for those already diagnosed.
- Chronic Disease Management Programs: Providing structured programs for individuals with chronic conditions to help them manage their disease, including medication management and lifestyle changes.
- Rehabilitation Services: Offering rehabilitation and physical therapy for conditions like stroke or chronic musculoskeletal disorders.
- Supportive Care: Providing palliative care and support for individuals with advanced or terminal chronic conditions.
Public Health Policies:
Public health policies at the local, national, and international levels play a significant role in chronic disease prevention.
- Tobacco Control Measures: Implementing and enforcing policies that restrict smoking in public places, increase taxes on tobacco products, and promote smoking cessation programs.
- Nutrition and Food Policies: Promoting healthy food options, reducing the consumption of unhealthy foods, and implementing food labeling and nutrition education.
- Physical Activity Initiatives: Encouraging physical activity through initiatives like building and maintaining safe parks, bike lanes, and walking paths.
- Environmental Regulations: Enforcing environmental regulations that improve air and water quality, reducing exposure to environmental toxins.
- Access to Healthcare: Expanding access to healthcare services, including preventive care, for all individuals, regardless of income or insurance status.
Research and Surveillance:
- Public health agencies and research institutions conduct studies and collect data on chronic diseases, risk factors, and interventions to inform prevention strategies and policies. Surveillance systems monitor trends in chronic conditions, enabling timely responses.
Impact of Chronic Conditions:
Here are some of the common impacts of chronic conditions.
Physical Consequences:
- Reduced Quality of Life: Chronic conditions can lead to pain, discomfort, fatigue, and physical limitations that affect a person’s overall well-being and quality of life.
- Disability: Some chronic conditions can result in varying degrees of disability, affecting a person’s ability to perform daily activities, work, or participate in social and recreational activities.
- Complications: Chronic conditions can lead to complications that further impact health. For example, uncontrolled diabetes can result in complications like neuropathy, retinopathy, and cardiovascular disease.
- Increased Healthcare Utilization: People with chronic conditions often require frequent medical care, leading to increased healthcare costs.
Emotional and Psychological Effects:
- Emotional Distress: Living with a chronic condition can lead to feelings of stress, anxiety, depression, and frustration, especially when managing symptoms or facing uncertainty about the future.
- Social Isolation: Some individuals with chronic conditions may experience social isolation due to physical limitations or stigma associated with their condition.
- Coping Challenges: Learning to cope with a chronic condition can be emotionally challenging, requiring adaptation to changes in one’s life and daily routines.
Social and Economic Implications:
- Financial Burden: The costs associated with managing a chronic condition can be substantial, including medication, healthcare services, and accommodations. This financial burden can lead to economic strain.
- Impact on Employment: Some chronic conditions may result in job loss or reduced work hours, affecting an individual’s income and job security.
- Family and Caregiver Impact: Chronic conditions can also affect the lives of family members and caregivers who provide support and assistance to those with the condition.
Healthcare System Impact:
- Increased Healthcare Costs: Chronic conditions are a significant driver of healthcare costs, including hospitalizations, medications, and long-term care.
- Resource Allocation: The management of chronic conditions demands a substantial portion of healthcare resources, which can limit resources available for other healthcare needs.
Public Health Impact:
- Public Health Burden: Chronic conditions pose a substantial public health burden, contributing to a significant portion of healthcare costs and impacting the overall health of populations.
- Reduced Productivity: Chronic conditions can lead to reduced workforce productivity, affecting the economy at large.
- Health Disparities: Chronic conditions can disproportionately affect vulnerable populations, exacerbating health disparities based on factors like income, race, and access to healthcare.
FAQs:
What are chronic conditions?
Chronic conditions are long-lasting health issues that persist for an extended period, often lasting for three months or more. They may require ongoing management and care.
What’s the difference between chronic and acute conditions?
Acute conditions have a sudden onset and typically resolve quickly, while chronic conditions persist over an extended period. Acute conditions are often severe and short-lived, whereas chronic conditions are ongoing and may be less severe but have long-term effects.
What are common examples of chronic conditions?
Common chronic conditions include diabetes, heart disease, arthritis, asthma, chronic obstructive pulmonary disease (COPD), and autoimmune diseases like rheumatoid arthritis and lupus.
What are the risk factors for chronic conditions?
Risk factors vary depending on the condition but can include genetics, lifestyle choices (e.g., diet, smoking, physical inactivity), environmental factors (e.g., exposure to toxins), and age.
How are chronic conditions diagnosed?
Diagnosis typically involves a medical evaluation, medical history review, physical examination, and diagnostic tests such as blood tests, imaging, and sometimes biopsies.
How are chronic conditions managed?
Management often involves a combination of medication, lifestyle modifications, therapies (physical, occupational, or psychological), surgery if necessary, and ongoing medical care.
Can chronic conditions be prevented?
Many chronic conditions can be prevented or their onset delayed through healthy lifestyle choices, vaccination, and regular health check-ups.
What is the impact of chronic conditions on individuals and society?
Chronic conditions can have physical, emotional, social, and economic impacts, affecting quality of life and healthcare systems. They also contribute to healthcare costs and public health burdens.
What are the emerging trends in chronic condition research and management?
Trends include personalized medicine, telemedicine, early detection and predictive analytics, digital health, genomic research, disease biomarkers, regenerative medicine, lifestyle interventions, big data and AI, patient empowerment, and health equity.
How can individuals with chronic conditions improve their quality of life?
Individuals can improve their quality of life by adhering to treatment plans, adopting healthy lifestyle changes, seeking support and education, and actively managing their condition with healthcare providers.
Conclusion:
In conclusion, chronic conditions present a complex and multifaceted challenge to individuals, healthcare systems, and society at large. These long-lasting health issues demand ongoing attention, management, and support to mitigate their physical, emotional, and economic impacts. However, with advancements in medical research, personalized care, and a growing emphasis on prevention and patient empowerment, there is hope for improved outcomes and a better quality of life for those living with chronic conditions. As we continue to expand our knowledge and refine our approaches, the future holds promise for more effective prevention, diagnosis, and management of chronic conditions, ultimately reducing their burden and enhancing the well-being of those affected.
Possible References Used


One Comment