Cartilage is a flexible connective tissue found in various parts of the body, serving as a structural component and providing support to certain organs and structures. It is firmer than other types of connective tissue like muscle or skin but more flexible than bone. Cartilage consists of cells called chondrocytes embedded within a matrix composed of collagen fibers and proteoglycans, which give it its unique properties.
Definition and Characteristics of Cartilage.
Here are the key characteristics of cartilage.
- Composition: Cartilage is composed of cells called chondrocytes, which are embedded within a dense extracellular matrix. This matrix consists of collagen fibers and proteoglycans.
- Chondrocytes: Chondrocytes are specialized cells responsible for producing and maintaining the extracellular matrix of cartilage. They are found in spaces called lacunae within the matrix.
- Extracellular Matrix (ECM): The ECM of cartilage is a gel-like substance composed of collagen fibers and proteoglycans. Collagen provides tensile strength, while proteoglycans attract water, giving the matrix its resilience and ability to withstand compression.
- Avascularity: Cartilage lacks blood vessels, nerves, and lymphatic vessels. Nutrients and oxygen are obtained through diffusion from surrounding tissues.
- Types: There are three main types of cartilage: hyaline cartilage, elastic cartilage, and fibrocartilage. Each type has distinct characteristics and is found in specific regions of the body.
- Hyaline Cartilage: This type has a glassy, smooth appearance and is the most abundant form of cartilage. It forms the articular surfaces of bones in joints, supports the respiratory passages, and is involved in embryonic bone development.
- Elastic Cartilage: Elastic cartilage contains a higher proportion of elastic fibers in its matrix, making it flexible and elastic. It is found in structures like the external ear and the epiglottis.
- Fibrocartilage: Fibrocartilage has a dense arrangement of collagen fibers, making it very strong. It serves as a shock absorber and is found in areas subjected to heavy pressure, such as intervertebral discs and the pubic symphysis.
- Function: Cartilage provides a smooth surface for joint movement, absorbs shock in weight-bearing joints, helps maintain the shape of structures like the nose and ears, and plays a role in the growth of long bones during development.
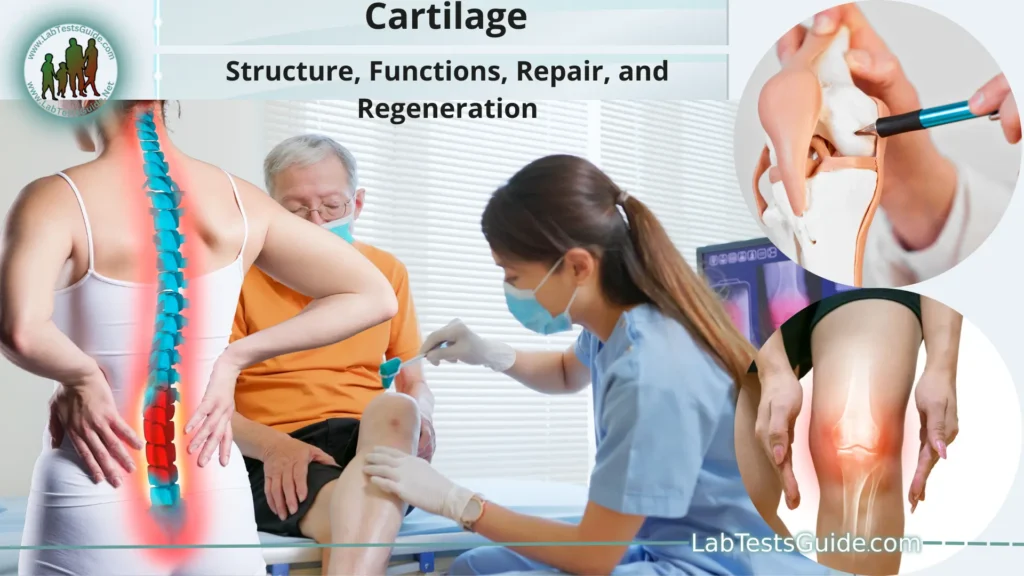
- Repair and Regeneration: Cartilage has limited regenerative capacity due to its avascular nature. Injuries to cartilage can lead to long-term issues. Researchers are exploring various techniques, including tissue engineering and stem cell therapies, to improve cartilage repair.
Types of Cartilage:
Hyaline Cartilage:
- Appearance: Hyaline cartilage has a smooth and glassy appearance under a microscope.
- Composition: It contains a matrix primarily composed of collagen fibers and proteoglycans, giving it a semi-transparent appearance.
- Function: Hyaline cartilage provides a smooth surface for joint movement, reduces friction between bones, supports the respiratory passages (trachea and bronchi), and aids in embryonic bone development and growth.
- Locations: It is found in the articular surfaces of synovial joints, the ribcage, the nasal septum, and the larynx.
Elastic Cartilage:
Appearance: Elastic cartilage contains more elastic fibers within its matrix, giving it a yellowish color and greater flexibility.
Composition: Its matrix includes collagen fibers, proteoglycans, and a significant amount of elastic fibers.
Function: Elastic cartilage is highly flexible and provides support with elasticity. It maintains the shape of certain structures while allowing flexibility and deformation.
Locations: It is found in the external ear (pinna), the epiglottis (flap covering the trachea during swallowing), and the auditory (Eustachian) tubes.
Fibrocartilage:
- Appearance: Fibrocartilage has a dense arrangement of collagen fibers, making it appear tougher and more durable.
- Composition: The matrix of fibrocartilage contains a high proportion of collagen fibers and proteoglycans.
- Function: Fibrocartilage is specialized for its tensile strength and ability to absorb shock. It acts as a cushion and provides stability in regions subjected to heavy pressure and stress.
- Locations: Fibrocartilage is found in the intervertebral discs of the spine, the pubic symphysis (joint between the pelvic bones), and certain tendons and ligaments.
Structure of Cartilage:
Chondrocytes:
- Chondrocytes are the specialized cells found within cartilage. They are responsible for producing and maintaining the extracellular matrix.
- Chondrocytes are situated in spaces called lacunae, which are small cavities within the matrix where individual chondrocytes reside.
Extracellular Matrix (ECM):
- The extracellular matrix is a crucial component of cartilage, providing its unique properties and functions.
- Collagen Fibers: Collagen is a protein that forms fibers within the matrix, providing tensile strength to the cartilage. Collagen fibers are responsible for the tissue’s ability to resist stretching and maintain its shape.
- Proteoglycans: These are large molecules consisting of a core protein surrounded by chains of glycosaminoglycans (GAGs). Proteoglycans attract and trap water molecules, which gives the cartilage its ability to resist compression and absorb shock. This interaction between proteoglycans and water also helps maintain tissue hydration.
Perichondrium:
- In some types of cartilage, particularly hyaline and elastic cartilage, a layer of connective tissue called the perichondrium surrounds the cartilage. It contains blood vessels and acts as a source of nutrients for the cartilage.
- The perichondrium also contains progenitor cells that can differentiate into chondrocytes, aiding in cartilage growth and repair.
Territorial and Interterritorial Matrix:
- In hyaline cartilage, the matrix is divided into two regions: the territorial matrix and the interterritorial matrix.
- The territorial matrix is immediately surrounding the lacunae and contains a higher concentration of chondrocytes and their immediate matrix products.
- The interterritorial matrix is the space between the territorial matrices and contains a lower concentration of cells and a greater concentration of collagen fibers and proteoglycans.
Blood Supply and Healing:
- Cartilage is avascular, meaning it lacks its own blood vessels. Nutrients and oxygen are obtained through diffusion from nearby blood vessels in the surrounding tissues.
- Due to its limited blood supply, cartilage has a relatively slow healing process compared to other tissues.
Functions of Cartilage:
Here are the main functions of cartilage.
Support and Structure:
- Cartilage provides structural support to various parts of the body. It helps maintain the shape and integrity of certain structures, ensuring they remain functional and properly positioned.
Smooth Joint Movement:
- In synovial joints, such as the knee or shoulder joints, articular cartilage covers the ends of bones, providing a smooth and low-friction surface for joint movement. This allows bones to glide against each other during motion, reducing friction and wear.
Shock Absorption:
- Certain types of cartilage, like fibrocartilage, have a dense arrangement of collagen fibers that enable them to absorb shocks and impacts. For example, the fibrocartilage in intervertebral discs cushions the vertebrae and absorbs the compressive forces experienced during activities like walking and running.
Embryonic Bone Development:
- Hyaline cartilage plays a crucial role in the development of the skeleton in embryos. It serves as a template for the formation of many bones, including the long bones. This process is known as endochondral ossification, where cartilage gradually transforms into bone tissue.
Respiratory Support:
- Cartilage provides support to the respiratory system. In the trachea and bronchi, rings of hyaline cartilage prevent collapse of these air passages, maintaining an open pathway for air to flow during breathing.
Bone Growth and Longitudinal Growth:
- During the growth phase, cartilage at the ends of long bones (epiphyseal plates) allows for longitudinal bone growth. Chondrocytes in these plates divide and contribute to the elongation of bones before they eventually calcify and are replaced by bone tissue.
Maintaining Shape of Structures:
- Elastic cartilage, found in structures like the external ear and the epiglottis, helps maintain their shape while allowing for flexibility. This elasticity allows the ear to return to its original shape after being bent or folded.
Distribution of Forces:
- Cartilage helps distribute forces evenly across joint surfaces, preventing excessive stress on specific areas. This is particularly important in weight-bearing joints like the knee and hip.
Bone Protection:
- Fibrocartilage in structures like the intervertebral discs provides protection to adjacent bones by cushioning and absorbing impact forces. This is essential in preventing damage to the spinal column during activities that involve bending, twisting, and weight-bearing.
Locations of Cartilage in the Body:
Here are some key locations where cartilage is present.
Articular Cartilage:
- Location: Found on the ends of bones within synovial joints, where bones come into contact with each other.
- Function: Provides a smooth and low-friction surface for joint movement, reducing wear and allowing for smooth articulation.
Nasal Cartilage:
- Location: Composes the nasal septum and maintains the shape of the nose.
- Function: Provides structural support to the nose, helping to maintain its shape and preventing collapse of the nasal passages.
Tracheal and Bronchial Rings:
- Location: Rings of hyaline cartilage are present in the trachea and bronchi.
- Function: Prevents the collapse of the air passages during breathing, ensuring an open pathway for air movement.
Costal Cartilage:
Location: Connects the ribs to the sternum (breastbone).
Function: Provides flexibility and allows for slight movement of the ribcage during breathing, contributing to lung expansion.
Auricular Cartilage:
- Location: Forms the structure of the external ear (pinna).
- Function: Maintains the shape of the ear while allowing for flexibility and movement.
Epiglottis:
- Location: A flap of elastic cartilage at the base of the tongue, covering the entrance of the trachea during swallowing.
- Function: Protects the trachea by preventing food and liquids from entering the respiratory tract while swallowing.
Intervertebral Discs:
- Location: Situated between the vertebrae of the spinal column.
- Function: Fibrocartilage in intervertebral discs acts as a shock absorber, cushions the spine, and allows for slight movement between vertebrae.
Pubic Symphysis:
- Location: The joint between the two pubic bones in the pelvic region.
- Function: Fibrocartilage in the pubic symphysis provides stability and flexibility to the pelvis, particularly during childbirth.
Larynx (Voice Box) Cartilage:
- Location: Forms the framework of the larynx, supporting the vocal cords and aiding in sound production.
- Function: Maintains the structure of the larynx and assists in phonation (sound production).
Cartilage Growth and Development:
Embryonic Cartilage Formation:
- Cartilage serves as a precursor to bone during embryonic development. The process of bone formation from cartilage is known as endochondral ossification.
- Mesenchymal cells, which are undifferentiated stem cells, condense to form cartilage models of future bones. This process begins during the early stages of embryonic development.
Appositional Growth:
- Cartilage growth occurs through two main mechanisms: appositional growth and interstitial growth.
- Appositional growth involves the addition of new cartilage tissue on the surface of existing cartilage. Chondroblasts within the perichondrium (a layer of connective tissue surrounding some cartilage types) differentiate into chondrocytes and produce new matrix.
Interstitial Growth:
- Interstitial growth occurs from within the cartilage tissue. Chondrocytes within lacunae divide and produce new matrix, causing the cartilage to grow from within.
- This type of growth contributes to the lengthening of bones during childhood, particularly in the growth plates (epiphyseal plates) located at the ends of long bones.
Epiphyseal Plate Growth:
- In long bones, the epiphyseal plate (growth plate) consists of hyaline cartilage located between the epiphysis (end) and diaphysis (shaft) of the bone.
- During childhood and adolescence, the epiphyseal plate is responsible for longitudinal bone growth. Chondrocytes in the growth plate divide, leading to the production of new cartilage matrix. As new cartilage forms, older cartilage is replaced by bone through endochondral ossification.
Hormonal Influence:
- Growth hormone, secreted by the pituitary gland, plays a significant role in stimulating the growth of cartilage and bone during childhood.
- Puberty marks the closure of the growth plates due to hormonal changes, leading to the cessation of longitudinal bone growth.
Remodeling and Maturation:
- As bones mature, cartilage undergoes gradual transformation into bone tissue through the process of endochondral ossification.
- Chondrocytes in the center of the cartilage model hypertrophy (enlarge) and die, creating cavities. Blood vessels invade these cavities, bringing osteoblasts that deposit bone matrix. Eventually, the cartilage is replaced by bone, with only a thin layer of cartilage remaining on the articular surfaces.
Cartilage Repair and Regeneration:
Here are some approaches being investigated.
Conservative Management:
- Mild cartilage injuries may respond well to conservative treatments like rest, physical therapy, pain management, and lifestyle modifications.
- Conservative approaches are often used for managing early-stage cartilage damage and mild osteoarthritis.
Arthroscopic Procedures:
- Arthroscopy involves minimally invasive procedures in which a thin camera (arthroscope) is inserted into the joint. This technique can be used to remove damaged tissue, smooth rough surfaces, or stimulate limited healing responses.
Microfracture Surgery:
- In this technique, small holes are drilled into the subchondral bone beneath the damaged cartilage. This stimulates bleeding and the formation of a blood clot, which contains cells that can differentiate into cartilage-forming cells.
- The formed tissue is usually fibrocartilage, which is not as resilient as normal hyaline cartilage.
Autologous Chondrocyte Implantation (ACI):
- ACI involves removing a small sample of healthy cartilage from the patient, growing chondrocytes in a lab, and then implanting them into the damaged area.
- This technique aims to replace damaged cartilage with healthy cartilage cells, potentially leading to better tissue quality.
Osteochondral Autograft or Allograft Transplantation:
- In this procedure, a portion of both cartilage and underlying bone is transplanted from a non-weight-bearing area of the joint (autograft) or a donor (allograft) to the damaged area.
- The goal is to replace the damaged tissue with healthy tissue from another part of the body or a donor.
Tissue Engineering and Scaffold-Based Approaches:
- Researchers are investigating the use of biocompatible scaffolds that mimic the extracellular matrix of cartilage. These scaffolds can be seeded with chondrocytes or stem cells, encouraging tissue growth.
- Combined with growth factors and other biological cues, these approaches aim to generate new cartilage tissue.
Stem Cell Therapy:
- Stem cells, such as mesenchymal stem cells (MSCs), are being explored for their potential to differentiate into chondrocyte-like cells and aid in cartilage repair.
- Techniques include injecting stem cells into the damaged area or combining them with scaffold-based approaches.
Platelet-Rich Plasma (PRP):
- PRP involves using a concentrated solution of the patient’s own platelets, which are rich in growth factors, to stimulate tissue healing.
- While not a direct cartilage regeneration method, PRP injections can be used in conjunction with other treatments.
Gene Therapy and Biologics:
- These emerging approaches involve delivering genes or biological agents to the damaged area to stimulate cartilage repair and regeneration.
Cartilage-related Medical Conditions:
Here are some common cartilage-related medical conditions:
- Osteoarthritis: Osteoarthritis is a degenerative joint disease that primarily affects the articular cartilage in joints. Over time, the cartilage deteriorates, leading to pain, inflammation, stiffness, and reduced joint mobility.
As the condition progresses, bones may develop bony growths called osteophytes. Osteoarthritis commonly affects weight-bearing joints like the knees, hips, and spine. - Cartilage Injuries and Tears: Injuries to cartilage can occur due to trauma, sports-related activities, or wear and tear over time.
Common cartilage injuries include meniscal tears in the knee (tears in the fibrocartilage discs), chondral defects (localized damage to the articular cartilage), and labral tears in the hip and shoulder. - Chondromalacia Patellae: Chondromalacia patellae, also known as runner’s knee, is characterized by softening and degeneration of the cartilage on the underside of the patella (kneecap). This condition can cause pain and discomfort, particularly when bending the knee.
- Costochondritis: Costochondritis involves inflammation of the cartilage that connects the ribs to the breastbone (sternum). It can cause chest pain that mimics heart-related conditions but is typically localized and worsened by movement or touch.
- Avascular Necrosis: Avascular necrosis, also known as osteonecrosis, is a condition where bone tissue dies due to a lack of blood supply. This can affect the overlying cartilage as well.
It often occurs in the hip joint and can lead to cartilage damage and joint dysfunction. - Juvenile Idiopathic Arthritis: This type of arthritis affects children and adolescents. It can cause joint inflammation, pain, and cartilage damage.
Prompt medical management is essential to prevent long-term joint damage and deformities. - Knee Chondral Defects: Chondral defects are localized areas of damage to the articular cartilage in the knee joint. These defects can lead to pain, swelling, and reduced joint function.
- Osteochondritis Dissecans: This condition involves the detachment of a piece of cartilage and underlying bone within a joint. It often affects the knee and elbow joints and can cause pain and joint instability.
- Rheumatoid Arthritis: Rheumatoid arthritis is an autoimmune condition that can lead to joint inflammation, damage to cartilage and bone, and joint deformities.
It commonly affects multiple joints, including those in the hands and feet. - Ear Cartilage Conditions: Conditions like cauliflower ear (auricular hematoma) can occur due to trauma to the ear, resulting in damage to the cartilage’s blood supply and subsequent deformity.
Comparative Anatomy:
Here are some examples.
- Shark Cartilage: Sharks have a unique cartilaginous skeleton known as a chondrocranium, which forms their skull. This lightweight structure helps maintain buoyancy in water, as opposed to the denser bones found in most other vertebrates.
- Bird Beaks: Birds possess beaks made of keratin, a protein similar to that found in cartilage. These beaks vary greatly in shape and size, reflecting the birds’ specialized feeding habits, whether for pecking, probing, or capturing prey.
- Elephant Tusks: Elephant tusks are elongated structures made of dentin, a tissue similar to cartilage and bone. They serve various functions, including foraging, self-defense, and communication.
- Cephalopod Beaks: Cephalopods like squids and octopuses have beak-like structures made of chitin, a material related to both cartilage and exoskeletons. These beaks are used for predation and handling prey.
- Human Ears and Nose: The human ear’s external structure (auricle) contains elastic cartilage, providing flexibility while maintaining shape. The nose also contains cartilage that helps maintain its form and supports the nasal passages.
- Intervertebral Discs: While humans have fibrocartilage in their intervertebral discs, some animals like whales have a unique cartilaginous structure that cushions their spine and supports their massive bodies in aquatic environments.
- Fish Gills: Fish have gill arches made of cartilage that support their gills, aiding in respiration by extracting oxygen from water. The gill arches vary among species, reflecting their adaptations to different aquatic environments.
- Amphibian and Reptile Scales: Some amphibians and reptiles have dermal scales made of keratinized tissues similar to cartilage. These scales provide protection and regulate moisture.
Future Directions in Cartilage Research:
Here are some areas that researchers are exploring.
- Tissue Engineering and Biomaterials: Advances in tissue engineering aim to create biomimetic scaffolds that closely resemble the native cartilage extracellular matrix. These scaffolds can provide a supportive environment for cells to grow and differentiate into functional cartilage tissue.
- Stem Cell Therapies: Stem cells, including mesenchymal stem cells, induced pluripotent stem cells, and embryonic stem cells, hold great potential for cartilage regeneration. Researchers are working on optimizing techniques to guide stem cells into becoming chondrocyte-like cells for effective tissue repair.
- Gene Therapy and Biologics: Gene therapy approaches involve delivering genes that promote cartilage growth and healing directly to damaged areas. Biologics, such as growth factors and cytokines, are being studied for their ability to stimulate cartilage repair processes.
- 3D Printing and Bioprinting: 3D printing and bioprinting technologies enable the fabrication of customized cartilage constructs with precise architecture. This technology holds promise for creating patient-specific implants and tissue-engineered cartilage grafts.
- Advanced Imaging Techniques: High-resolution imaging techniques, such as MRI, CT, and ultrasound, are being refined to better assess cartilage quality, detect early changes, and monitor the progression of cartilage-related conditions.
- Smart Materials and Drug Delivery: Smart materials that respond to specific cues (such as pH or temperature) can be integrated into cartilage scaffolds for controlled drug delivery, helping to promote healing and reduce inflammation.
- Biomechanics and Functional Assessment: Researchers are investigating how biomechanical forces influence cartilage development, maintenance, and repair. Understanding the mechanical properties of cartilage is essential for designing effective interventions.
- Precision Medicine: The concept of precision medicine involves tailoring treatment approaches to an individual’s specific genetic, molecular, and clinical characteristics. Personalized therapies can lead to more targeted and effective outcomes in cartilage repair.
- Combination Therapies: Researchers are exploring combination therapies that integrate various approaches, such as stem cell treatments with biologics or scaffolds, to enhance cartilage regeneration.
- Biomarkers and Early Detection: Identifying specific biomarkers associated with cartilage health and disease progression could lead to early detection and intervention, potentially preventing or slowing the development of cartilage-related conditions.
- Animal Models and Translational Research: Studies using animal models provide insights into the efficacy and safety of novel cartilage repair approaches before clinical trials. Translational research bridges the gap between laboratory findings and clinical applications.
FAQs:
What is cartilage?
Cartilage is a specialized connective tissue that provides structural support, maintains shape, and enables smooth movement in the body. It consists of cells called chondrocytes embedded within an extracellular matrix composed of collagen fibers and proteoglycans.
What are the types of cartilage?
There are three main types of cartilage: hyaline cartilage, elastic cartilage, and fibrocartilage. Each type has distinct characteristics and is found in specific locations within the body.
What is the function of cartilage?
Cartilage serves various functions, including providing smooth joint surfaces, absorbing shock, maintaining the shape of structures like the nose and ears, supporting embryonic bone development, and allowing for longitudinal bone growth.
Can cartilage heal on its own?
Cartilage has limited regenerative capacity due to its avascular nature. Small injuries might heal through scar tissue formation, but larger or deeper injuries often require medical intervention to promote proper healing.
What is osteoarthritis?
Osteoarthritis is a degenerative joint disease that involves the gradual breakdown of cartilage in joints. It leads to pain, stiffness, and reduced joint mobility, particularly in weight-bearing joints.
How is cartilage repaired?
Cartilage repair strategies include conservative management, arthroscopic procedures, microfracture surgery, autologous chondrocyte implantation (ACI), osteochondral transplantation, tissue engineering, stem cell therapy, and gene therapy.
What is the growth plate in bones?
The growth plate, also known as the epiphyseal plate, is a cartilaginous region located at the ends of long bones. It allows for longitudinal bone growth during childhood and adolescence.
How is cartilage different from bone?
Cartilage is avascular, has a flexible and resilient matrix, and lacks mineralization. In contrast, bone is vascular, contains mineralized matrix (hydroxyapatite), and provides structural support and protection.
What is the role of cartilage in joint movement?
Articular cartilage covers the ends of bones in synovial joints, providing a smooth surface for frictionless joint movement. It helps distribute forces evenly and prevents bone-on-bone contact.
Can cartilage be replaced with synthetic materials?
While synthetic materials have been used as cartilage replacements, the challenge lies in replicating the complex properties and functions of natural cartilage. Tissue-engineered cartilage and biocompatible scaffolds are promising approaches.
Conclusion:
In conclusion, cartilage is a remarkable and multifaceted connective tissue that plays crucial roles in providing structural support, enabling smooth joint movement, absorbing shock, and contributing to skeletal development. Its diverse types, from hyaline to elastic and fibrocartilage, are strategically located throughout the body to fulfill specific functions. While its limited regenerative capacity poses challenges for repair, ongoing research into tissue engineering, stem cell therapies, and advanced technologies offers promising avenues for improving cartilage healing, regeneration, and overall quality of life for those affected by cartilage-related conditions.
Possible References Used