The cardiovascular system, also known as the circulatory system, is one of the most vital systems in the human body. It consists of the heart, blood vessels, and blood, and its primary function is to transport oxygen, nutrients, hormones, and waste products throughout the body.

Definition of Cardiovascular System.
The cardiovascular system, also known as the circulatory system, is a complex network of organs and blood vessels that is responsible for circulating blood throughout the body. Its primary function is to transport oxygen, nutrients, hormones, and waste products to and from the body’s cells and organs. This system plays a crucial role in maintaining the body’s overall health and homeostasis by ensuring that all tissues receive the necessary oxygen and nutrients while removing metabolic waste products.
What is the importance of the Cardiovascular system?
Here are the key reasons why the cardiovascular system is crucial.
- Transport of Oxygen: The cardiovascular system carries oxygen from the lungs to body tissues and organs. Oxygen is essential for cellular respiration, where cells generate energy (ATP) for various metabolic processes. Without oxygen delivery, tissues would quickly become hypoxic (oxygen-deprived), leading to cell damage or death.
- Nutrient Delivery: It transports nutrients absorbed from the digestive system to cells throughout the body. These nutrients, including glucose, amino acids, and fatty acids, provide the building blocks and energy necessary for cellular functions, growth, and repair.
- Waste Removal: The cardiovascular system transports metabolic waste products, such as carbon dioxide and urea, away from cells to be eliminated from the body. Efficient waste removal is vital to prevent the buildup of toxic substances within tissues.
- Hormone Circulation: Hormones produced by endocrine glands are released into the bloodstream and transported to target organs and tissues. This ensures the proper regulation of various physiological processes, including metabolism, growth, and stress responses.
- Temperature Regulation: Blood circulation plays a role in regulating body temperature. When the body is too warm, blood vessels in the skin dilate to release heat, while in cold conditions, they constrict to conserve heat.
- Immune System Support: The blood carries white blood cells and antibodies, which are crucial components of the immune system. They help defend the body against infections and foreign invaders.
- Maintenance of pH and Electrolyte Balance: The cardiovascular system helps maintain the body’s pH balance (acid-base equilibrium) and regulates the concentration of electrolytes, such as sodium, potassium, and calcium, in the bloodstream. These factors are essential for proper cellular function.
- Blood Pressure Regulation: The cardiovascular system plays a role in regulating blood pressure, ensuring that it remains within a healthy range. High or low blood pressure can have adverse effects on overall health.
- Tissue Repair and Growth: Blood circulation is essential for delivering nutrients and oxygen to injured tissues for repair and regeneration. It also supports the growth and development of various body structures, especially during childhood and adolescence.
- Organ and System Functionality: The cardiovascular system supports the proper functioning of all organs and body systems. Insufficient blood flow or dysfunction in this system can lead to organ damage and a wide range of health issues.
Anatomy of the Cardiovascular System:
Heart:
- The heart is a muscular organ located in the chest, slightly to the left. It is about the size of a closed fist and is enclosed by a double-layered membrane called the pericardium.
- The heart consists of four chambers: two atria (right atrium and left atrium) and two ventricles (right ventricle and left ventricle).
- The atria receive blood, while the ventricles pump blood out of the heart.
- The heart’s walls contain cardiac muscle tissue responsible for contracting and pumping blood.
Blood Vessels:
- Arteries: Arteries are thick-walled, muscular blood vessels that carry oxygenated blood away from the heart to various parts of the body.
- Veins: Veins transport deoxygenated blood back to the heart. They typically have thinner walls and may contain one-way valves to prevent backflow.
- Capillaries: Capillaries are tiny, thin-walled vessels that connect arteries and veins. They facilitate the exchange of oxygen, nutrients, and waste products between the blood and body tissues.
Blood:
- Blood is a fluid connective tissue that flows through the cardiovascular system. It is composed of various components, including:
- Red Blood Cells (Erythrocytes): These cells contain hemoglobin, which binds to oxygen and carries it to tissues.
- White Blood Cells (Leukocytes): These cells play a vital role in the immune system, defending the body against infections.
- Platelets: Small cell fragments that help with blood clotting.
- Plasma: The liquid component of blood, composed mainly of water, electrolytes, proteins, hormones, and waste products.
Major Blood Vessels:
- Aorta: The largest artery in the body, originating from the left ventricle and carrying oxygenated blood to the rest of the body.
- Superior and Inferior Vena Cava: Large veins that return deoxygenated blood from the upper and lower parts of the body, respectively, to the right atrium of the heart.
- Pulmonary Arteries and Veins: These vessels are responsible for transporting blood between the heart and the lungs for oxygenation (pulmonary arteries carry deoxygenated blood, and pulmonary veins carry oxygenated blood).
Heart Valves:
- Four heart valves ensure one-way blood flow through the heart:
- Tricuspid Valve: Located between the right atrium and right ventricle.
- Bicuspid (Mitral) Valve: Located between the left atrium and left ventricle.
- Pulmonary Valve: Located between the right ventricle and the pulmonary artery.
- Aortic Valve: Located between the left ventricle and the aorta.
Coronary Arteries:
- Coronary arteries supply the heart muscle (myocardium) with oxygen and nutrients. The left and right coronary arteries branch from the aorta and encircle the heart.
Cardiac Conduction System:
- This system consists of specialized cells that generate electrical impulses to coordinate heart contractions. Key components include the sinoatrial (SA) node, atrioventricular (AV) node, and bundle of His.
Pericardium:
- The pericardium is a double-layered sac surrounding the heart. It provides protection and reduces friction as the heart beats.
Circulation:
There are several important aspects of circulation.
Systemic Circulation:
- Systemic circulation refers to the circulation of blood throughout the body, excluding the lungs. Oxygenated blood is pumped out of the left ventricle of the heart into the aorta, the largest artery, which branches into smaller arteries.
- Arteries carry oxygenated blood to various organs, tissues, and cells throughout the body.
- Capillaries are the smallest blood vessels that connect arteries to veins. They facilitate the exchange of oxygen, nutrients, and waste products between the blood and body tissues.
- Veins collect deoxygenated blood and waste products from body tissues and return it to the right atrium of the heart via the superior and inferior vena cava.
Pulmonary Circulation:
- Pulmonary circulation refers to the circulation of blood between the heart and the lungs.
- Deoxygenated blood from the body returns to the right atrium, is pumped into the right ventricle, and then flows through the pulmonary arteries to the lungs.
- In the lungs, blood picks up oxygen and releases carbon dioxide. Oxygenated blood returns to the heart via the pulmonary veins, entering the left atrium and then the left ventricle before being pumped into the systemic circulation.
Coronary Circulation:
- Coronary circulation refers to the circulation of blood within the heart muscle itself.
- The coronary arteries supply the myocardium (heart muscle) with oxygen and nutrients necessary for its contractions.
- Coronary veins collect deoxygenated blood from the heart muscle and return it to the right atrium.
Fetal Circulation:
- Fetal circulation is a specialized circulation that occurs in the developing fetus within the womb.
- Oxygen and nutrients are obtained from the mother’s bloodstream via the placenta.
- Fetal blood bypasses the lungs, as they are non-functional in the womb. This is achieved through structures like the foramen ovale and ductus arteriosus.
- After birth, as the infant takes its first breath and the lungs become functional, fetal circulation transitions to the adult circulation pattern.
Lymphatic Circulation (related system):
- The lymphatic system is a complementary system to the cardiovascular system.
- It circulates lymph, a clear fluid containing white blood cells, which plays a crucial role in immune function and fluid balance.
- The lymphatic system helps return excess tissue fluid (interstitial fluid) to the bloodstream and filters out pathogens and cellular debris
Cardiac Cycle:
Atrial Contraction (Atrial Systole):
- The cardiac cycle begins with atrial contraction, also known as atrial systole.
- Both atria contract simultaneously, pushing blood into the ventricles.
- The atrial contraction is initiated by an electrical impulse generated by the sinoatrial (SA) node, causing the atria to depolarize and contract.
Atrial Relaxation (Atrial Diastole):
- Following atrial contraction, the atria relax and begin to refill with blood.
- As the atria relax, pressure within them decreases, allowing blood from the venae cavae (superior and inferior) and pulmonary veins to flow into the atria.
Ventricular Contraction (Ventricular Systole):
- Ventricular systole begins shortly after atrial contraction.
- An electrical impulse generated by the atrioventricular (AV) node travels down the bundle of His and Purkinje fibers, causing the ventricles to contract.
- The right ventricle pumps deoxygenated blood into the pulmonary artery, while the left ventricle pumps oxygenated blood into the aorta.
- The closure of the atrioventricular valves (tricuspid and bicuspid/mitral valves) prevents blood from flowing back into the atria during ventricular contraction.
Ventricular Relaxation (Ventricular Diastole):
- After ventricular contraction, both ventricles relax during ventricular diastole.
- The relaxation phase allows the ventricles to refill with blood from the atria and prevents excessive pressure buildup.
- The semilunar valves (pulmonary and aortic valves) close at the beginning of ventricular diastole to prevent blood from flowing back into the ventricles from the pulmonary artery and aorta.
During the cardiac cycle, there are two important phases for blood flow:
- Systole: This phase corresponds to ventricular contraction. During systole, blood is ejected from the ventricles into the pulmonary artery and aorta.
- Diastole: This phase corresponds to ventricular relaxation. During diastole, the ventricles fill with blood from the atria.
Cardiovascular Physiology:
Here are some key aspects of cardiovascular physiology.
Blood Pressure:
- Blood pressure is the force exerted by the blood against the walls of the arteries as it flows through them.
- It is typically measured in millimeters of mercury (mmHg) and is expressed as two values: systolic (the pressure during ventricular contraction) and diastolic (the pressure during ventricular relaxation).
- Blood pressure is regulated by various factors, including cardiac output, peripheral resistance, and hormonal control (e.g., renin-angiotensin-aldosterone system).
Cardiac Output:
- Cardiac output is the volume of blood pumped by the heart per minute and is a crucial determinant of blood pressure.
- It is calculated as the product of heart rate (beats per minute) and stroke volume (the volume of blood pumped by each heartbeat).
- The sympathetic nervous system and various hormones, such as epinephrine and norepinephrine, can modulate heart rate and stroke volume to adjust cardiac output.
Stroke Volume:
- Stroke volume is the volume of blood ejected by the left ventricle during each contraction (systole).
- It is influenced by factors such as preload (the amount of blood returning to the heart), afterload (the resistance the heart must overcome to eject blood), and contractility (the strength of ventricular contractions).
Heart Rate:
- Heart rate refers to the number of times the heart beats per minute.
- It is regulated by the autonomic nervous system, with the sympathetic branch increasing heart rate (positive chronotropic effect) and the parasympathetic branch decreasing heart rate (negative chronotropic effect).
Blood Flow and Hemodynamics:
- Hemodynamics is the study of blood flow within the cardiovascular system.
- Blood flow is determined by factors like pressure, resistance, and vessel diameter. Poiseuille’s law describes the relationship between these factors and blood flow rate.
- Vasoconstriction (narrowing of blood vessels) and vasodilation (widening of blood vessels) are critical mechanisms for regulating blood flow and distribution.
Blood Composition and Functions:
- Blood is composed of various elements, including red blood cells (erythrocytes), white blood cells (leukocytes), platelets, and plasma.
- Red blood cells carry oxygen (as oxyhemoglobin) and carbon dioxide (as carbaminohemoglobin).
- White blood cells play a crucial role in the immune response.
- Platelets are involved in blood clotting.
- Plasma transports nutrients, hormones, electrolytes, and waste products.
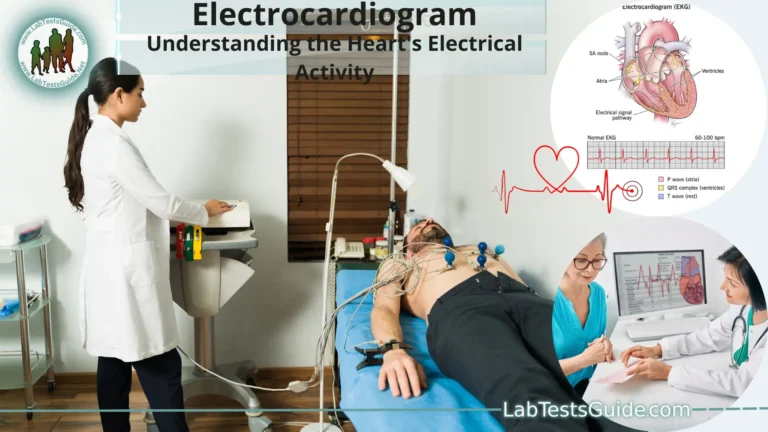
Electrocardiography (ECG or EKG):
- Electrocardiography is a diagnostic tool that records the electrical activity of the heart.
- The ECG waveform consists of P-waves (atrial depolarization), QRS complexes (ventricular depolarization), and T-waves (ventricular repolarization).
- ECGs are used to diagnose arrhythmias, conduction abnormalities, and other cardiac conditions.
Electrocardiography (ECG or EKG):
Electrical Activity of the Heart:
- The heart generates electrical impulses that coordinate the contraction (systole) and relaxation (diastole) of its chambers, allowing it to pump blood effectively. This electrical activity is crucial for maintaining a regular heartbeat.
Components of an ECG:
The resulting ECG waveform consists of several key components:
- P-Wave: Represents atrial depolarization (contraction). It reflects the electrical activity as the impulse moves through the atria.
- QRS Complex: Represents ventricular depolarization (contraction). It reflects the electrical activity as the impulse moves through the ventricles. The QRS complex is typically the largest part of the ECG.
- T-Wave: Represents ventricular repolarization (relaxation). It reflects the electrical recovery of the ventricles after contraction.
ECG Leads:
Common lead systems include:
- 12-Lead ECG: This is the standard ECG recording method, which uses 12 leads to provide a comprehensive view of the heart’s electrical activity. It includes six limb leads (I, II, III, aVR, aVL, aVF) and six precordial leads (V1 to V6).
- 3-Lead ECG: A simplified version often used for basic cardiac monitoring, usually with limb leads (I, II, III).
Clinical Applications:
ECG is used in a variety of clinical settings to.
- Diagnose Arrhythmias: It can detect irregular heart rhythms (arrhythmias) such as atrial fibrillation, ventricular tachycardia, and bradycardia.
- Assess Ischemia and Infarction: ECG can identify signs of inadequate blood supply to the heart (ischemia) and heart muscle damage (infarction), as seen in myocardial infarctions (heart attacks).
- Evaluate Heart Enlargement: Changes in the ECG pattern can suggest conditions like left ventricular hypertrophy (LVH), which is an enlarged heart chamber.
- Monitor Cardiac Medications: It helps monitor the effects of medications that affect the heart’s electrical conduction.
- Preoperative and Pre-Procedure Screening: ECG is often performed before surgeries or certain medical procedures to assess cardiac risk.
- Holter Monitoring: This involves wearing a portable ECG device for an extended period to capture intermittent or unusual heart rhythms that may not be apparent during a standard ECG.
- Exercise Stress Testing: ECG is used during exercise stress tests to evaluate how the heart responds to physical activity, helping diagnose coronary artery disease.
Interpretation:
- Interpreting an ECG requires expertise, as the waveform patterns can provide valuable diagnostic information. Clinicians look for abnormalities in wave shapes, intervals, and segments to identify cardiac issues.
Blood Flow and Hemodynamics:
Here are the key concepts related to blood flow and hemodynamics.
Hemodynamics Basics:
- Hemodynamics is the study of the physical principles governing blood flow, pressure, and resistance within the circulatory system.
- Blood flow (Q) is the volume of blood passing through a vessel per unit of time and is typically measured in milliliters per minute (mL/min).
- Blood pressure (BP) is the force exerted by the blood against the walls of blood vessels and is measured in millimeters of mercury (mmHg).
Factors Affecting Blood Flow:
Blood flow is influenced by several factors:
- Pressure Gradient: Blood flows from areas of higher pressure to areas of lower pressure. The pressure gradient drives blood through the circulatory system.
- Vessel Radius: The diameter of blood vessels significantly affects resistance. Smaller vessels offer more resistance to blood flow, while larger vessels have less resistance.
- Vessel Length: Longer vessels offer more resistance than shorter ones, as blood encounters more friction along the vessel walls.
- Blood Viscosity: The thickness or stickiness of blood affects resistance. Higher viscosity results in greater resistance to flow.
- Vessel Compliance: Arteries can expand and contract to accommodate changes in blood volume. Compliance affects blood pressure regulation.
Poiseuille’s Law:
- Poiseuille’s law describes the relationship between blood flow, pressure, and resistance:
- Blood Flow (Q) = (Change in Pressure) / (Resistance)
- This law demonstrates that blood flow is directly proportional to the pressure difference (ΔP) between two points and inversely proportional to resistance (R).
Vasoconstriction and Vasodilation:
- Vasoconstriction is the narrowing of blood vessels, which increases resistance and reduces blood flow.
- Vasodilation is the widening of blood vessels, which decreases resistance and increases blood flow.
- The autonomic nervous system, hormones, and local factors regulate these processes to meet specific physiological needs.
Blood Pressure Regulation:
- Blood pressure is regulated to maintain adequate tissue perfusion while preventing damage to blood vessel walls.
- Baroreceptors in the aorta and carotid arteries detect changes in blood pressure and send signals to the cardiovascular control center in the brain to adjust heart rate and vessel diameter.
- Hormonal mechanisms, such as the renin-angiotensin-aldosterone system, also play a role in blood pressure regulation.
Local Blood Flow Regulation:
- Autoregulation allows tissues to regulate their own blood flow based on metabolic needs.
- Local factors such as oxygen, carbon dioxide, and pH levels can trigger vasodilation or vasoconstriction to match blood flow with tissue demand.
Blood Circulation Control:
Autonomic Nervous System (ANS):
- The autonomic nervous system plays a central role in regulating blood circulation. It consists of two branches:
- Sympathetic Nervous System: The sympathetic branch is responsible for the “fight or flight” response. When activated, it increases heart rate and contractility, causes vasoconstriction in some blood vessels (e.g., skin and digestive organs), and redistributes blood to vital organs like the heart and skeletal muscles.
- Parasympathetic Nervous System: The parasympathetic branch is responsible for the “rest and digest” response. It slows heart rate and reduces contractility, promoting vasodilation in some blood vessels and conserving energy.
Baroreceptor Reflex:
- Baroreceptors are specialized sensory receptors located in the walls of certain blood vessels, such as the carotid arteries and aorta. They detect changes in blood pressure.
- When blood pressure rises, baroreceptors send signals to the brain, which activates the parasympathetic nervous system, leading to decreased heart rate and vasodilation to lower blood pressure.
- When blood pressure falls, baroreceptors signal the sympathetic nervous system to increase heart rate and cause vasoconstriction to raise blood pressure.
Hormonal Regulation:
Several hormones play roles in blood circulation control.
- Renin-Angiotensin-Aldosterone System (RAAS): When blood pressure decreases, specialized cells in the kidneys release renin, triggering a cascade that leads to the formation of angiotensin II. Angiotensin II constricts blood vessels and stimulates aldosterone release, which increases sodium and water retention, raising blood pressure.
- Antidiuretic Hormone (ADH): Also known as vasopressin, ADH is released by the pituitary gland in response to low blood volume or increased blood osmolarity. It causes vasoconstriction and increases water reabsorption in the kidneys to raise blood pressure.
- Epinephrine and Norepinephrine: These hormones, released by the adrenal medulla in response to stress or sympathetic stimulation, increase heart rate, contractility, and vasoconstriction to raise blood pressure.
Local Blood Flow Regulation:
Tissues can regulate their own blood flow locally based on metabolic demands. For example:
- Increased tissue oxygen demand leads to vasodilation, ensuring adequate oxygen delivery.
- Accumulation of metabolic waste products (e.g., carbon dioxide, lactic acid) triggers vasodilation to remove waste and improve oxygen delivery.
- Endothelial Cells: Endothelial cells lining blood vessels release nitric oxide, a potent vasodilator, and endothelin, a vasoconstrictor. They help maintain vascular tone and regulate blood flow.
- Central Control in the Brain: Brain regions, such as the medulla oblongata and hypothalamus, regulate blood pressure and circulation by receiving and processing sensory information and issuing commands to adjust autonomic responses.
Cardiovascular Disorders:
Here are some common cardiovascular disorders.
Hypertension (High Blood Pressure):
- Hypertension is a condition characterized by elevated blood pressure levels consistently higher than normal.
- It is a significant risk factor for heart disease, stroke, and other cardiovascular complications.
- Hypertension is often called the “silent killer” because it can be asymptomatic for years while causing damage to blood vessels and organs.
Coronary Artery Disease (CAD):
- CAD is a condition in which the coronary arteries, which supply the heart muscle with oxygen and nutrients, become narrowed or blocked by atherosclerosis (plaque buildup).
- This can lead to angina (chest pain) or heart attacks (myocardial infarctions) if blood flow to the heart muscle is severely restricted.
Heart Failure:
- Heart failure occurs when the heart cannot pump blood effectively to meet the body’s needs.
- It can result from conditions like CAD, high blood pressure, or cardiomyopathies.
- Symptoms include shortness of breath, fatigue, fluid retention (edema), and decreased exercise tolerance.
Arrhythmias:
- Arrhythmias are irregular heart rhythms caused by abnormalities in the heart’s electrical system.
- They can manifest as tachycardias (fast heart rhythms) or bradycardias (slow heart rhythms).
- Some arrhythmias are benign, while others can be life-threatening.
Valvular Heart Diseases:
- Valvular heart diseases involve abnormalities in the heart valves, which can lead to conditions like stenosis (narrowing) or regurgitation (leakage) of the valves.
- Common valvular disorders include aortic stenosis, mitral regurgitation, and mitral valve prolapse.
Peripheral Artery Disease (PAD):
- PAD is a condition in which atherosclerosis affects the arteries outside the heart, typically in the legs.
- It can cause reduced blood flow to the extremities, leading to pain, cramping, and, in severe cases, tissue damage or gangrene.
Atherosclerosis:
- Atherosclerosis is the buildup of fatty deposits (plaques) in the walls of arteries, which can narrow and stiffen the arteries.
- It is a common underlying cause of several cardiovascular disorders, including CAD and PAD.
Congenital Heart Defects:
- Congenital heart defects are structural abnormalities present at birth. They can range from mild defects with few symptoms to severe conditions requiring immediate medical attention.
Cardiomyopathies:
- Cardiomyopathies are diseases of the heart muscle that affect its structure and function.
- There are different types of cardiomyopathies, including dilated, hypertrophic, and restrictive cardiomyopathies.
Stroke:
- Stroke occurs when there is a disruption in blood flow to the brain, either due to a blood clot (ischemic stroke) or bleeding (hemorrhagic stroke).
- Some strokes are related to cardiovascular disorders, particularly atrial fibrillation and atherosclerosis.
Thrombosis and Embolism:
- Thrombosis refers to the formation of blood clots within blood vessels, while embolism occurs when a clot breaks free and travels to other parts of the body, potentially blocking blood flow.
Infective Endocarditis: - Infective endocarditis is an infection of the inner lining of the heart and heart valves, often caused by bacteria entering the bloodstream.
Diagnostic Tools and Tests:
Here are some commonly used diagnostic tools and tests in medicine.
Blood Tests:
- Blood tests, also known as blood panels or blood work, analyze blood samples to assess various aspects of health.
Common blood tests include:
- Complete Blood Count (CBC): Measures the number of red and white blood cells and platelets.
- Basic Metabolic Panel (BMP) or Comprehensive Metabolic Panel (CMP): Evaluates electrolyte and kidney function, glucose levels, and more.
- Lipid Profile: Measures cholesterol and triglyceride levels.
- Blood Chemistry Tests: Assess specific substances in the blood, such as liver enzymes, thyroid hormones, and blood gases.
Imaging Studies:
- Medical imaging techniques visualize the internal structures of the body to diagnose conditions and assess organ function.
Common imaging studies include:
- X-rays: Use ionizing radiation to create images of bones and some soft tissues.
- Computed Tomography (CT or CAT scan): Combines X-ray technology with computer processing to create detailed cross-sectional images of the body.
- Magnetic Resonance Imaging (MRI): Uses magnetic fields and radio waves to generate high-resolution images of soft tissues and organs.
- Ultrasound: Uses high-frequency sound waves to visualize internal structures, often used for fetal monitoring and assessing blood flow.
- Positron Emission Tomography (PET scan): Shows metabolic activity within the body, aiding in the diagnosis and staging of cancers.
- Electrocardiography (ECG or EKG): ECG records the electrical activity of the heart to diagnose arrhythmias, ischemia, and other cardiac conditions.
- Electroencephalogram (EEG): EEG measures electrical activity in the brain and is used to diagnose neurological disorders such as epilepsy and sleep disorders.
- Biopsy: A biopsy involves the removal of a small sample of tissue or cells for microscopic examination.
It is used to diagnose cancer, infections, and certain other conditions. - Endoscopy: Endoscopy uses a flexible tube with a camera and light to visualize and examine the interior of organs such as the digestive tract (gastroscopy, colonoscopy), respiratory tract (bronchoscopy), or urinary tract (cystoscopy).
- Mammography: Mammography is an X-ray of the breast used for breast cancer screening and diagnosis.
- Colonoscopy: A colonoscopy is used to examine the colon and rectum for conditions like colorectal cancer, polyps, and inflammatory bowel disease.
- Pulmonary Function Tests (PFTs): PFTs measure lung function, including lung capacity and the ability to inhale and exhale effectively. They are used to diagnose respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD).
- Bone Densitometry (DEXA): DEXA scans measure bone density and are used to diagnose osteoporosis and assess fracture risk.
- Genetic Testing: Genetic tests analyze DNA to identify inherited genetic mutations or predispositions to certain diseases.
Examples include carrier screening, diagnostic genetic testing, and pharmacogenomic testing. - Nuclear Medicine: Nuclear medicine scans use small amounts of radioactive materials to diagnose and treat diseases. Common tests include bone scans, thyroid scans, and cardiac stress tests.
- Urinalysis: Urinalysis examines the physical, chemical, and microscopic properties of urine to diagnose urinary tract conditions and systemic diseases.
Treatment and Management:
Here are some general approaches and strategies used in the treatment and management of various health conditions.
Medications:
- Medications are commonly used to treat a wide range of medical conditions, including infections, chronic diseases, pain, and more.
- Types of medications include antibiotics, antivirals, analgesics (pain relievers), anti-inflammatories, immunosuppressants, and many others.
- Medications can be administered orally, topically, intravenously, or through other routes, depending on the condition and the drug.
Surgery:
- Surgery is often necessary to treat conditions that cannot be managed with medications alone. It may involve the removal of tumors, repair of damaged organs, or correction of anatomical abnormalities.
- Types of surgical procedures include open surgery, minimally invasive surgery (e.g., laparoscopy), and robotic-assisted surgery.
Physical Therapy and Rehabilitation:
- Physical therapy aims to improve physical function and mobility through exercises, stretches, and other techniques.
- Rehabilitation programs help individuals recover from injuries, surgeries, or chronic conditions and regain independence.
Diet and Nutrition:
- Proper nutrition plays a crucial role in managing various medical conditions, such as diabetes, heart disease, and obesity.
- Dietary changes may involve limiting certain foods, increasing others, and managing portion sizes.
Lifestyle Modifications:
- Lifestyle changes, such as quitting smoking, reducing alcohol consumption, and increasing physical activity, can significantly impact the management of many chronic diseases.
Psychological and Behavioral Therapies:
- Psychological therapies, including cognitive-behavioral therapy (CBT), can be effective in managing mental health conditions such as depression and anxiety.
- Behavioral therapies are used to modify unhealthy behaviors and establish healthier ones.
Chronic Disease Management:
- Chronic diseases such as diabetes, hypertension, and asthma require ongoing management, often involving regular monitoring, medication adherence, and lifestyle adjustments.
- Disease management programs may offer education, support, and resources to help patients better manage their conditions.
Palliative Care and Hospice:
- Palliative care focuses on improving the quality of life for individuals with serious illnesses by addressing pain, symptoms, and emotional well-being.
- Hospice care provides end-of-life care and support for individuals with terminal illnesses.
Complementary and Alternative Medicine (CAM):
- Some patients explore complementary therapies such as acupuncture, herbal supplements, and massage therapy to complement conventional medical treatments.
- It’s important to consult with healthcare professionals before using CAM therapies, as some may interact with medications or have limited evidence of effectiveness.
Monitoring and Follow-Up:
- Regular medical check-ups, tests, and screenings are essential to monitor disease progression and treatment effectiveness.
- Healthcare providers may adjust treatment plans based on the patient’s response to therapy.
Patient Education and Self-Management:
- Patient education empowers individuals to understand their conditions, adhere to treatment plans, and make informed decisions about their health.
- Self-management strategies help patients take an active role in their care by monitoring symptoms and following recommended lifestyle modifications.
- Preventive Care: Preventive care, including vaccinations, health screenings, and lifestyle changes, aims to prevent the onset of diseases and reduce the risk of complications.
Prevention and Healthy Lifestyle:
Here are key aspects of prevention and maintaining a healthy lifestyle:
- Regular Health Check-ups: Schedule regular check-ups with your healthcare provider for screenings, vaccinations, and assessments of your overall health.
Early detection of health issues can lead to more effective treatment and better outcomes. - Vaccinations: Stay up to date with vaccinations to protect yourself and others from preventable diseases.
Common vaccines include those for influenza, tetanus, measles, mumps, rubella, and COVID-19. - Healthy Diet: Eat a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
Limit processed foods, sugary beverages, and excessive salt intake.
Pay attention to portion sizes to maintain a healthy weight. - Regular Physical Activity: Engage in regular physical activity to maintain cardiovascular health, muscle strength, and overall fitness.
Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week, along with muscle-strengthening activities. - Maintain a Healthy Weight: Achieve and maintain a healthy body weight through a combination of a balanced diet and regular exercise.
Consult with a healthcare provider or dietitian for personalized weight management guidance.
- Avoid Smoking and Tobacco Products: Quit smoking and avoid exposure to secondhand smoke and other tobacco products.
Smoking is a major risk factor for various cancers, heart disease, and respiratory conditions. - Limit Alcohol Consumption: If you drink alcohol, do so in moderation. Guidelines vary by country, but moderation generally means up to one drink per day for women and up to two drinks per day for men.
Excessive alcohol consumption is associated with various health risks, including liver disease and certain cancers. - Manage Stress: Practice stress management techniques such as meditation, deep breathing exercises, mindfulness, or hobbies that help you relax.
Chronic stress can contribute to various health problems, including cardiovascular disease and mental health disorders. - Get Adequate Sleep: Aim for 7-9 hours of quality sleep per night to support overall health and well-being.
Poor sleep is linked to obesity, heart disease, diabetes, and mental health issues. - Practice Safe Sex: Use protection (condoms or dental dams) to prevent sexually transmitted infections (STIs) and unintended pregnancies. Get regular STI screenings if sexually active.
- Sun Protection: Protect your skin from the sun’s harmful UV rays by wearing sunscreen, protective clothing, and sunglasses.Regular skin checks can help detect skin cancer early.
- Mental Health Care: Prioritize your mental health by seeking professional help if needed. Engage in activities that promote mental well-being, such as socializing, practicing mindfulness, and seeking support from friends and family.
- Avoid Risky Behaviors: Refrain from risky behaviors, such as driving under the influence, using illicit drugs, and engaging in dangerous activities that can lead to injuries or accidents.
- Stay Informed: Stay informed about health-related news and recommendations from reliable sources, such as healthcare providers and public health organizations.
- Build Supportive Relationships: Maintain positive relationships with friends and family, as social connections are essential for emotional well-being and resilience.
Health Education:
- Educate yourself about your specific health risks and make informed decisions about your health.
- Participate in health education programs and seek guidance from healthcare professionals.
Pediatric Cardiovascular System:
Fetal Development of the Heart:
- The development of the heart begins in the early stages of fetal development.
- Initially, the heart is a simple tube, but it undergoes complex changes to form four chambers: two atria and two ventricles.
- The fetal heart also has structures like the foramen ovale and ductus arteriosus that allow blood to bypass the lungs because they are not fully functional in the womb.
Neonatal Adaptation:
- At birth, the neonatal cardiovascular system undergoes significant changes as the baby transitions from fetal to postnatal life.
- The closure of the foramen ovale and ductus arteriosus, as well as changes in blood flow and pressure, are crucial for the adaptation process.
Congenital Heart Defects:
- Congenital heart defects are structural abnormalities present at birth in the heart or major blood vessels.
- These defects can range from mild to severe and can affect blood flow, oxygenation, and cardiac function.
- Examples include ventricular septal defects (VSD), atrial septal defects (ASD), and tetralogy of Fallot.
Growth and Development:
- The pediatric cardiovascular system must adapt and grow as a child develops.
- The heart and blood vessels increase in size and complexity to support the child’s increasing metabolic demands and body size.
Pediatric Cardiovascular Conditions:
- Children can develop various cardiovascular conditions, such as arrhythmias, heart murmurs, cardiomyopathies, and Kawasaki disease.
- Timely diagnosis and appropriate management are crucial to ensure optimal outcomes for pediatric patients with heart conditions.
Pediatric Cardiovascular Evaluation:
- Pediatric cardiologists specialize in diagnosing and treating heart conditions in children.
- Evaluation may involve non-invasive tests like echocardiography, electrocardiography (ECG or EKG), and Holter monitoring.
Pediatric Cardiac Surgery:
- Some children with complex congenital heart defects may require surgical interventions to repair or correct heart abnormalities.
- Pediatric cardiac surgeons are skilled in performing these delicate procedures.
Pediatric Cardiac Rehabilitation:
- For children recovering from cardiac surgery or managing heart conditions, cardiac rehabilitation programs tailored to their age and needs can promote recovery and overall well-being.
Lifestyle and Prevention:
- Promoting a healthy lifestyle from an early age is essential for pediatric cardiovascular health.
- Encouraging physical activity, a balanced diet, and avoidance of tobacco smoke can reduce the risk of heart disease in adulthood.
FAQs:
What is climate change, and what are its causes?
Climate change refers to long-term alterations in the Earth’s average weather patterns. It is primarily caused by the accumulation of greenhouse gases in the atmosphere, primarily from human activities such as burning fossil fuels, deforestation, and industrial processes.
How does vaccination work?
Vaccination stimulates the immune system by introducing a weakened or inactivated form of a pathogen or a piece of it (antigen). This exposure helps the immune system recognize and remember the pathogen, allowing it to respond effectively if the person is exposed to the actual disease in the future.
What are renewable energy sources?
Renewable energy sources are energy resources that are naturally replenished, such as sunlight (solar energy), wind (wind energy), water (hydroelectric energy), and geothermal heat. They are considered sustainable because they do not deplete over time.
How do antibiotics work, and why is antibiotic resistance a concern?
Antibiotics are drugs that kill or inhibit the growth of bacteria. They work by targeting specific bacterial structures or processes. Antibiotic resistance occurs when bacteria mutate and become resistant to antibiotics, making infections more difficult to treat and posing a global health threat.
What is artificial intelligence (AI)?
Artificial intelligence refers to the development of computer systems that can perform tasks that typically require human intelligence, such as learning, problem-solving, and decision-making. AI encompasses machine learning, natural language processing, and robotics, among other technologies.
How does the cardiovascular system work?
The cardiovascular system consists of the heart, blood vessels, and blood. It pumps oxygen-rich blood to the body’s tissues and returns oxygen-depleted blood to the heart and lungs. The heart’s rhythmic contractions create blood flow, and the blood vessels regulate the distribution of blood throughout the body.
What is the difference between climate change and global warming?
Climate change is a broader term that refers to long-term shifts in the Earth’s climate patterns, which can involve both warming and cooling. Global warming specifically refers to the long-term increase in the Earth’s average surface temperature, often associated with the enhanced greenhouse effect.
How does the human brain work?
The human brain is a complex organ responsible for processing sensory information, thoughts, emotions, and motor functions. It consists of billions of neurons connected by synapses, allowing electrical and chemical signals to transmit information. Brain regions have specific functions related to cognition, memory, emotions, and more.
What is the difference between weather and climate?
Weather refers to the short-term atmospheric conditions in a specific location, including temperature, humidity, precipitation, and wind. Climate, on the other hand, refers to the long-term patterns and averages of weather conditions in a region over extended periods, typically 30 years or more.
How does a vaccine for a virus like COVID-19 get developed and approved?
The development of a vaccine involves preclinical testing, clinical trials (Phases I, II, and III), and regulatory review. Clinical trials assess vaccine safety and efficacy in human subjects. Regulatory agencies, such as the FDA, review trial data before granting approval for emergency use or full licensure.
Conclusion:
In conclusion, the cardiovascular system is a vital component of the human body, consisting of the heart, blood vessels, and blood, working together to ensure the delivery of oxygen, nutrients, and essential substances to various tissues and organs while removing waste products. Understanding the anatomy, circulation, and cardiac cycle, as well as the physiology, diagnostic tools, and common disorders associated with this system, is crucial for maintaining good health and effectively managing cardiovascular conditions. Additionally, staying informed about emerging trends in healthcare and adopting a healthy lifestyle can contribute to the prevention of cardiovascular diseases and promote overall well-being.
Possible References Used