A boil is a skin infection that is usually caused by the bacteria Staphylococcus aureus (staph). A carbuncle is a group of boils located in one area of the body. If left alone, a boil will break and drain on its own over time. In certain cases, a doctor may need to cut into your skin to drain the pus.
Definition of a Boil.
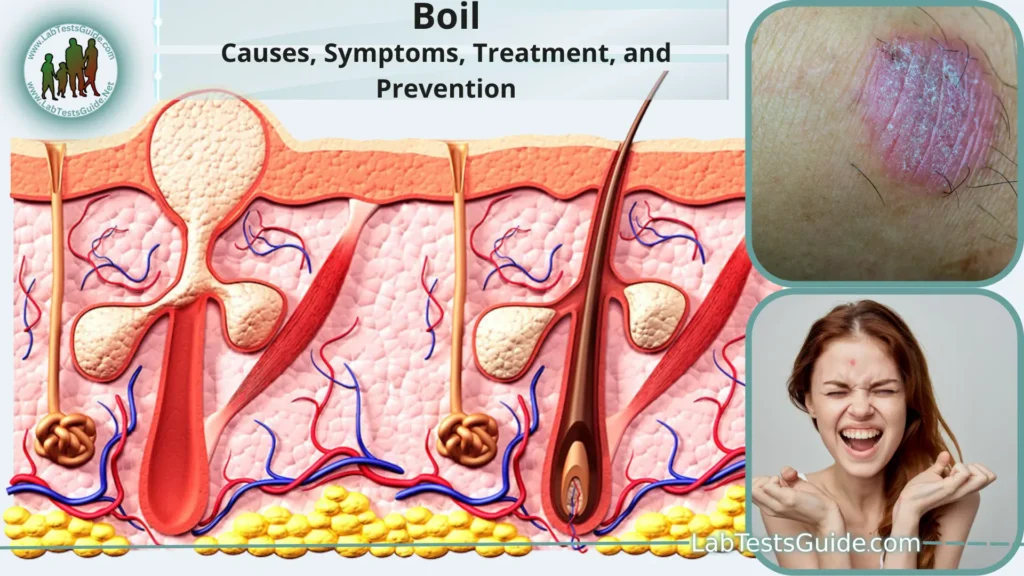
A boil, also known as a furuncle, is a painful and inflamed bump or lump that forms beneath the skin’s surface. It is typically caused by a bacterial infection, most commonly involving the Staphylococcus aureus bacterium. Boils usually start as a red, tender area, which gradually becomes more swollen and painful as it fills with pus.
Causes of Boils:
Here are some common causes and risk factors associated with the development of boils.
- Bacterial Infection: The most common cause of boils is a bacterial infection, often due to Staphylococcus aureus. These bacteria can enter the body through small cuts, breaks in the skin, or hair follicles.
- Weakened Immune System: Individuals with compromised immune systems, such as those with diabetes, HIV/AIDS, or other conditions that weaken the body’s ability to fight infections, are at higher risk of developing boils.
- Poor Hygiene: Inadequate personal hygiene can increase the risk of bacterial infections and, subsequently, the development of boils. Regularly washing the skin and keeping it clean can help prevent boils.
- Close Contact: Boils can be contagious. Close contact with someone who has a boil or who carries the bacteria on their skin (staphylococcal carriage) can increase the risk of infection.
- Ingrown Hairs: Ingrown hairs, particularly in the beard area for men or the pubic area for women, can become infected and develop into boils.
- Friction and Pressure: Continual friction or pressure on the skin, such as from tight clothing or repeated shaving, can cause skin irritation and potentially lead to the development of boils.
- Underlying Skin Conditions: Certain skin conditions, such as eczema or acne, can make the skin more susceptible to bacterial infections and, consequently, the formation of boils.
- Nasal Carriage of Staph Bacteria: Carrying Staphylococcus aureus bacteria in the nasal passages without symptoms (nasal carriage) can increase the risk of recurrent skin infections, including boils.
- Poor Diet and Nutrition: A diet lacking in essential nutrients and vitamins can weaken the immune system, making the body less able to fight off infections, including those that lead to boils.
- Hot and Humid Climates: Living in hot and humid environments can promote sweat and skin friction, increasing the likelihood of skin irritation and bacterial growth, which can contribute to boil formation.
Symptoms of a Boil:
- Pain and Tenderness: A boil is often painful and tender to the touch. This pain can range from mild discomfort to significant tenderness, making it uncomfortable to press on or manipulate the affected area.
- Redness and Swelling: The skin around the boil becomes red and swollen. The redness and inflammation are signs of the body’s immune response to the infection.
- Raised Bump: A boil appears as a raised, round bump on the skin’s surface. It may feel firm to the touch initially and become progressively softer as it fills with pus.
- Pus Formation: One of the hallmark signs of a boil is the development of pus within the bump. Pus is a thick, yellow or white fluid that consists of dead white blood cells, bacteria, and tissue debris. As the boil matures, the center becomes filled with pus, causing it to look like a white or yellow bump.
- Head or “Point” Formation: As the boil progresses, a visible “head” or point often forms at the center. This is where the skin over the boil is thinnest and is more likely to rupture to allow the pus to drain. The presence of a head is a sign that the boil is nearing maturity.
- Fever (in Some Cases): In more severe cases of infection, a person may develop a low-grade fever. This is a sign that the body is actively fighting the infection, and it typically occurs with larger or more deeply infected boils.
- Pain Relief After Draining: When a boil eventually bursts and drains, there is often significant relief from the pressure and pain associated with the boil. This is a natural part of the healing process.
Diagnosis of boil:
- Visual Examination: The healthcare provider will visually inspect the affected area to assess the appearance and characteristics of the skin lesion. Boils often have distinctive features, such as redness, swelling, and a pus-filled center. The presence of these features can strongly suggest a boil.
- Medical History: The healthcare provider may ask you about your medical history and any recent skin issues or infections. They may inquire about factors such as previous boils, underlying health conditions, and recent illnesses that could weaken your immune system.
- Physical Examination: In addition to examining the affected area, the healthcare provider may perform a physical examination to assess the overall health of your skin and identify any other skin conditions or abnormalities.
- Culturing of Pus (in Some Cases): In certain situations, especially when the boil is particularly large, recurrent, or severe, the healthcare provider may decide to culture the pus from the boil. This involves taking a sample of the pus and sending it to a laboratory for analysis to determine the specific bacteria causing the infection. This information can help guide antibiotic treatment if needed.
- Evaluation for Underlying Conditions: If you have recurrent or multiple boils, the healthcare provider may investigate whether there is an underlying condition contributing to your susceptibility to skin infections. This might involve blood tests or other diagnostic procedures to assess your overall health and immune function.
Prevention of boil:
Here are some preventive measures you can take to reduce your chances of developing boils.
Maintain Proper Hygiene:
- Regularly wash your hands and body with soap and water, especially after activities that may expose your skin to dirt or bacteria.
- Keep your skin clean and dry to minimize the growth of bacteria on the skin’s surface.
- Use Antibacterial Soap: Consider using an antibacterial soap or cleanser for bathing and washing your hands, especially if you have a history of recurrent boils.
- Clean and Care for Wounds: Properly clean and dress any cuts, scrapes, or wounds to prevent bacteria from entering the skin. Apply an antiseptic or antibiotic ointment if recommended.
- Avoid Sharing Personal Items: Do not share personal items such as towels, razors, clothing, or bedding, as this can spread bacteria that may lead to skin infections.
- Practice Safe Shaving: If you shave areas of your body, use a clean razor and shaving cream to reduce the risk of nicks and cuts that can become infected.
- Manage Skin Conditions: If you have skin conditions like eczema, acne, or psoriasis, work with a healthcare provider to manage them effectively, as these conditions can make your skin more susceptible to infections.
- Maintain a Healthy Diet: Eating a balanced diet rich in vitamins and minerals can help support a healthy immune system, making your body better equipped to fight off infections.
- Stay Hydrated: Drinking enough water helps keep your skin hydrated and can contribute to overall skin health.
- Avoid Tight Clothing: Wearing tight-fitting clothing can create friction and pressure on the skin, which may lead to skin irritation and increased risk of developing boils.
- Treat Nasal Carriage: If you are a carrier of Staphylococcus aureus bacteria in your nasal passages (nasal carriage), discuss treatment options with your healthcare provider to reduce the risk of recurrent skin infections.
- Be Cautious in High-Risk Environments: If you work in environments where you are exposed to potential sources of infection (e.g., healthcare settings), follow recommended infection control practices, such as hand hygiene and wearing protective clothing when necessary.
- Seek Prompt Treatment: If you notice any signs of a skin infection, such as a red or painful bump, consult a healthcare provider promptly. Early treatment can help prevent the infection from worsening.
Treatment Options:
Here are common treatment options for boils.
Warm Compresses:
- Applying warm, moist compresses to the boil several times a day can help promote drainage and relieve pain.
- Soak a clean cloth or gauze pad in warm water, wring it out, and gently place it over the boil for about 20 minutes.
Antibacterial Ointments:
- Over-the-counter antibiotic ointments can be applied to the area after draining to prevent infection or as directed by a healthcare provider.
- Follow the instructions on the product label.
Pain Relief Medications:
- Over-the-counter pain relievers such as ibuprofen or acetaminophen can help reduce pain and discomfort associated with a boil. Follow the recommended dosage instructions.
Incision and Drainage:
- If the boil is large, painful, or does not improve with home care, a healthcare provider may perform a minor surgical procedure to drain the pus.
- This involves making a small incision to allow the pus to drain, relieving pressure and pain.
- The procedure is usually done after the area is numbed with a local anesthetic.
Antibiotics:
- If the infection is severe, involves multiple boils, or is recurrent, a healthcare provider may prescribe oral antibiotics to treat the underlying bacterial infection.
- Take the prescribed antibiotics exactly as directed, even if the symptoms improve before the medication is finished.
- Wound Care: After drainage or incision, keep the area clean and covered with a sterile bandage.
Change the bandage and clean the area regularly.
Follow any specific wound care instructions provided by your healthcare provider. - Avoid Squeezing or Popping: Do not attempt to squeeze or pop a boil on your own, as this can push the infection deeper into the skin or lead to complications.
- Follow-up Care: Attend any follow-up appointments recommended by your healthcare provider to monitor the healing process and ensure the infection has resolved.
- Address Underlying Health Conditions: If you have underlying health conditions that contribute to recurrent boils, such as diabetes or immune system disorders, work with your healthcare provider to manage these conditions effectively.
- Prevent Recurrence: Practice good hygiene and preventive measures to reduce the risk of future boils, as mentioned in the “Prevention” section.
Complications:
Here are some potential complications associated with boils.
- Cellulitis: Cellulitis is a bacterial skin infection that can occur when the bacteria causing the boil spread to the surrounding skin and deeper tissues. It is characterized by redness, warmth, swelling, and pain in the affected area. Cellulitis can be serious if not treated promptly with antibiotics.
- Abscess Formation: If the boil is not drained properly or if the infection is not effectively treated, it can lead to the formation of an abscess. An abscess is a collection of pus within a localized cavity, often requiring surgical drainage.
- Recurrence: Some individuals are more prone to developing recurrent boils, especially if they carry Staphylococcus aureus bacteria in their nasal passages (nasal carriage). Recurrent boils can be frustrating and may require ongoing treatment and preventive measures.
- Scarring: After a boil has healed, it can leave behind a scar, particularly if the skin was stretched significantly or if the boil was very large.
- Bloodstream Infection (Bacteremia): In rare cases, if the bacteria from a boil enter the bloodstream, it can lead to a condition known as bacteremia. This can potentially lead to more severe infections throughout the body, including sepsis, which is a life-threatening condition.
- Spread of Infection: Boils located in certain areas, such as the face or near joints, can be more concerning due to the risk of infection spreading to nearby structures, such as the eye or joint space. These situations require prompt medical attention.
- Scarring and Disfigurement (Cosmetic Concerns): Boils that are large or develop in visible areas of the body, like the face, can cause cosmetic concerns due to scarring and potential disfigurement.
When to Seek Medical Attention:
Here are specific situations in which you should seek medical attention for a boil.
- Large Boil: If the boil is larger than a half-inch in diameter or is growing rapidly, it may require medical attention, especially if it is causing significant pain or discomfort.
- Boil on the Face, Neck, or Spine: Boils in these areas can be more concerning due to the risk of complications or the spread of infection to critical structures. Prompt medical evaluation is advisable.
- High Fever: If you develop a fever along with a boil, it can be a sign that the infection is spreading and becoming more severe. Seek medical attention if your temperature is elevated.
- Multiple Boils: If you have multiple boils that are occurring simultaneously or one after another, especially if they are recurrent, it may be a sign of an underlying issue that requires investigation and treatment.
- Boil Near a Joint: Boils near a joint can be particularly problematic, as the infection can spread to the joint space, leading to joint damage. Seek medical care if a boil is near a joint or causing joint pain.
- Signs of Spreading Infection: If you notice red streaks extending from the boil, increasing redness and swelling, or experience symptoms like chills, nausea, or confusion, these can be signs of a spreading infection, and immediate medical attention is needed.
- Eye or Genital Area Boils: Boils in or around the eyes, as well as those in the genital area, require prompt medical evaluation due to the potential for complications and risks associated with these sensitive areas.
- Underlying Health Conditions: If you have underlying health conditions that weaken your immune system (e.g., diabetes, HIV/AIDS) or if you are taking medications that suppress your immune system, consult your healthcare provider promptly if you develop a boil.
- Recurrent Boils: If you experience recurrent boils or have a history of frequent boils, it’s advisable to consult with a healthcare provider to determine the underlying cause and establish a management plan.
- Severe Pain: If you are experiencing severe pain associated with the boil that is not relieved by over-the-counter pain relievers, consider seeking medical attention.
FAQs:
What is a boil?
A boil is a painful, pus-filled bump that forms beneath the skin due to a bacterial infection, often caused by Staphylococcus aureus bacteria.
What are the common symptoms of a boil?
Common symptoms include pain, redness, swelling, the formation of pus, and the development of a “head” or point at the center.
How are boils diagnosed?
Boils are typically diagnosed through a visual examination by a healthcare provider. In some cases, a culture of the pus may be taken to identify the specific bacteria causing the infection.
What causes boils?
Boils are primarily caused by bacterial infections, often when bacteria enter the skin through cuts, breaks, or hair follicles. Poor hygiene, weakened immune systems, and underlying health conditions can increase the risk.
Can I treat a boil at home?
Yes, small and uncomplicated boils can often be treated at home with warm compresses, over-the-counter pain relievers, and proper wound care. It’s important to avoid squeezing or popping a boil.
When should I seek medical attention for a boil?
Seek medical attention if the boil is large, extremely painful, near sensitive areas (e.g., face, genitals), accompanied by a fever, or if you have multiple boils. Also, consult a healthcare provider if you have recurrent boils or underlying health conditions.
How are boils treated by healthcare providers?
Treatment options may include incision and drainage, prescription antibiotics, and wound care. The specific treatment depends on the size and severity of the boil.
Can boils lead to complications?
Yes, untreated or improperly managed boils can lead to complications such as cellulitis, abscess formation, recurrence, and in rare cases, bloodstream infections.
How can I prevent boils?
Preventive measures include maintaining proper hygiene, using antibacterial soap, avoiding sharing personal items, managing underlying skin conditions, and seeking medical care for recurrent boils.
Are boils contagious?
Boils themselves are not highly contagious, but the bacteria causing boils (Staphylococcus aureus) can be transmitted through close skin-to-skin contact, so it’s advisable to avoid sharing personal items with someone who has a boil.
Conclusion:
In conclusion, boils are painful, pus-filled skin bumps caused by bacterial infections, most commonly Staphylococcus aureus. They typically present with symptoms such as redness, swelling, pain, and the formation of pus. While many boils can be managed at home with warm compresses and over-the-counter pain relievers, it’s crucial to seek medical attention in certain situations, especially if the boil is large, painful, near sensitive areas, or if you have a fever.
Prompt diagnosis and treatment are essential to prevent complications such as cellulitis, abscess formation, recurrence, and bloodstream infections. Preventive measures, including good hygiene practices and addressing underlying health conditions, can help reduce the risk of developing boils.
Possible References Used




