Anti-U1 RNP (Ribonucleoprotein) antibodies are autoantibodies that target a specific cellular component called the U1 small nuclear ribonucleoprotein particle. These antibodies are commonly associated with certain autoimmune diseases, most notably mixed connective tissue disease (MCTD) and systemic lupus erythematosus (SLE).

In short, Anti-U1 RNP antibodies are autoantibodies that mistakenly target a specific cellular component called the U1 small nuclear ribonucleoprotein particle. These antibodies are associated with autoimmune diseases like mixed connective tissue disease (MCTD) and systemic lupus erythematosus (SLE). They can disrupt the normal process of mRNA splicing, potentially contributing to the development of these diseases. Detection of these antibodies in the blood helps diagnose and classify these conditions.
What is Anti-U1 RNP Antibodies:
Anti-U1 RNP (Ribonucleoprotein) antibodies are autoantibodies that target a specific cellular component known as the U1 small nuclear ribonucleoprotein particle. These antibodies are associated with certain autoimmune diseases, particularly mixed connective tissue disease (MCTD) and systemic lupus erythematosus (SLE).
Role of U1 snRNP in Spliceosome:
The U1 small nuclear ribonucleoprotein particle (U1 snRNP) plays a critical role in the process of mRNA splicing within the spliceosome complex. The spliceosome is a large and dynamic molecular machine responsible for removing non-coding sequences (introns) from pre-messenger RNA (pre-mRNA) molecules and joining together the coding sequences (exons) to create mature messenger RNA (mRNA) molecules that can be translated into proteins. The U1 snRNP is an essential component of this complex splicing process.
The role of the U1 snRNP within the spliceosome can be summarized as follows:
- Recognition of the 5′ Splice Site: The U1 snRNP binds to the 5′ splice site at the beginning of an intron in the pre-mRNA molecule. The 5′ splice site is a specific sequence that marks the start of the intron that needs to be removed. The U1 snRNP recognizes and base-pairs with this sequence, ensuring accurate positioning of the spliceosome at the correct site for splicing.
- Stabilization of Spliceosome Formation: The U1 snRNP’s binding to the 5′ splice site stabilizes the initial formation of the spliceosome complex. This allows other components of the spliceosome to assemble and interact with the pre-mRNA molecule, creating a functional splicing machinery.
- Exon Definition: The binding of the U1 snRNP to the 5′ splice site helps define the boundaries of exons and introns. This recognition contributes to the accurate selection of splice sites during the splicing process.
- Spliceosome Activation: After initial binding of the U1 snRNP and other components, the spliceosome undergoes a series of structural changes and rearrangements to bring together the splice sites for catalysis. The U1 snRNP’s role in stabilizing the initial interaction is crucial for the subsequent steps of spliceosome activation and rearrangement.
- Spliceosome Catalysis: The activated spliceosome catalyzes two transesterification reactions, known as the branching reaction and the exon ligation reaction. These reactions result in the removal of the intron and the precise joining of adjacent exons to form mature mRNA.
Significance of Anti-U1 RNP Antibodies:
Anti-U1 RNP (Ribonucleoprotein) antibodies have significant clinical and diagnostic significance due to their association with specific autoimmune diseases and their potential impact on cellular processes. Here are the key points regarding the significance of these antibodies:
- Diagnostic Marker: The presence of anti-U1 RNP antibodies in a person’s blood can serve as a diagnostic marker for certain autoimmune diseases. These antibodies are strongly associated with mixed connective tissue disease (MCTD), an autoimmune disorder that shares features with systemic lupus erythematosus (SLE), scleroderma, and polymyositis. Detecting these antibodies helps doctors in diagnosing and distinguishing MCTD from other conditions.
- Disease Classification: Anti-U1 RNP antibodies aid in classifying autoimmune diseases. Their presence can help differentiate between different types of connective tissue disorders and guide treatment strategies. For instance, their presence in a person with clinical symptoms can help confirm a diagnosis of MCTD.
- Insight into Pathogenesis: The presence of anti-U1 RNP antibodies provides insight into the underlying autoimmune processes. These antibodies specifically target the U1 snRNP particle, which is vital for proper pre-mRNA splicing. When these antibodies disrupt the function of U1 snRNP, it can lead to abnormal mRNA processing and potentially contribute to the development of autoimmune diseases like MCTD and SLE.
- Monitoring Disease Progression: Monitoring the levels of anti-U1 RNP antibodies over time can be valuable for assessing disease progression and response to treatment. Changes in antibody levels might reflect changes in the autoimmune response or disease activity.
- Predicting Clinical Manifestations: The presence of anti-U1 RNP antibodies might be associated with specific clinical manifestations within autoimmune diseases. For example, certain symptoms or complications might be more prevalent in individuals who have these antibodies.
- Research and Treatment: Studying anti-U1 RNP antibodies can provide insights into the mechanisms underlying autoimmune diseases. Researchers are investigating how these antibodies disrupt normal cellular processes and contribute to disease. Understanding these mechanisms could potentially lead to the development of targeted treatments in the future.
Role of Anti-U1 RNP Antibodies in Autoimmune Diseases:
The role of anti-U1 RNP (Ribonucleoprotein) antibodies in autoimmune diseases, particularly mixed connective tissue disease (MCTD) and systemic lupus erythematosus (SLE), is complex and not fully understood. However, researchers have made several observations about how these antibodies might contribute to the development and progression of autoimmune diseases:
- Disruption of Splicing Process: Anti-U1 RNP antibodies can interfere with the normal splicing of mRNA molecules, leading to the production of faulty proteins or nonfunctional proteins.
- Generation of Autoantigens: Aberrant splicing caused by these antibodies can result in the production of proteins with altered structures. The immune system may perceive these altered proteins as foreign, leading to immune responses against the body’s own tissues.
- Immune Response Activation: The immune system recognizes U1 snRNP-antibody complexes as foreign entities, triggering an immune response that involves B cells, T cells, and inflammatory molecules. This response contributes to tissue damage and inflammation.
- Tissue Damage and Inflammation: The immune response initiated by anti-U1 RNP antibodies contributes to tissue damage and inflammation, leading to the characteristic symptoms of autoimmune diseases affecting various organs and systems.
- Specific Disease Associations: These antibodies are strongly associated with mixed connective tissue disease (MCTD) and can also be found in systemic lupus erythematosus (SLE). Their presence can correlate with certain clinical manifestations within these diseases.
- Potential for Organ-Specific Effects: The presence of these antibodies might influence the specific organs or systems affected in autoimmune diseases, contributing to the diverse range of symptoms seen in affected individuals.
- Heterogeneity in Effects: The impact of anti-U1 RNP antibodies varies among individuals. Some individuals with these antibodies develop autoimmune diseases, while others may not, due to complex interactions between genetic factors and immune responses.
- Research for Targeted Therapies: Ongoing research aims to uncover the precise mechanisms by which these antibodies contribute to autoimmune diseases. Understanding these mechanisms could lead to targeted therapies addressing the root causes of these conditions.
Autoimmune Diseases Associated with Anti-U1 RNP Antibodies:
- Mixed Connective Tissue Disease (MCTD): Anti-U1 RNP antibodies are strongly linked to MCTD, a condition characterized by a combination of symptoms from different connective tissue disorders, such as lupus, scleroderma, and polymyositis.
- Systemic Lupus Erythematosus (SLE): While more commonly associated with MCTD, anti-U1 RNP antibodies can also be found in some cases of SLE, a chronic autoimmune disease affecting multiple organs and systems.
These antibodies play a significant role in the diagnosis and classification of these diseases, and their presence helps healthcare providers differentiate between various autoimmune conditions and guide appropriate treatment strategies.
Laboratory Detection of Anti-U1 RNP Antibodies:
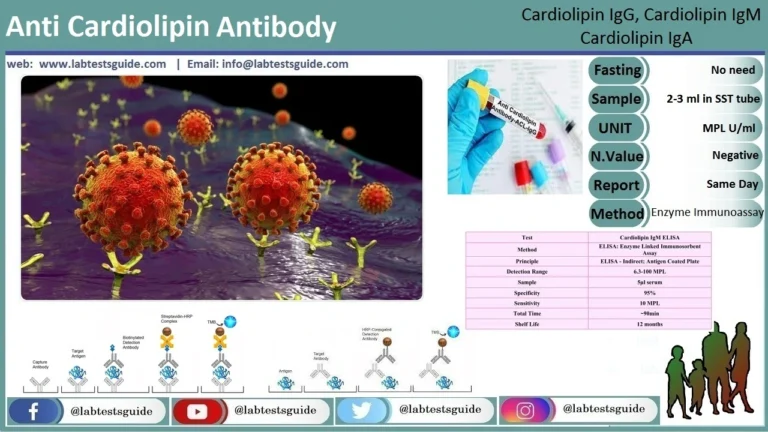
The laboratory detection of anti-U1 RNP (Ribonucleoprotein) antibodies involves specific tests that help identify the presence of these antibodies in a person’s blood. These tests are crucial for diagnosing and classifying autoimmune diseases, particularly mixed connective tissue disease (MCTD) and systemic lupus erythematosus (SLE), where these antibodies are associated. Here’s how the laboratory detection process works:
- Enzyme-Linked Immunosorbent Assay (ELISA): ELISA is a commonly used technique to detect and quantify antibodies in a sample. In the case of anti-U1 RNP antibodies, ELISA involves the following steps:
- A sample of the patient’s blood serum (which contains antibodies) is collected.
- U1 snRNP antigens (components of the U1 snRNP particle) are immobilized on a solid surface.
- The patient’s serum is added to the surface, allowing any anti-U1 RNP antibodies to bind to the immobilized antigens.
- Enzyme-labeled secondary antibodies that specifically recognize human antibodies are added. These secondary antibodies will bind to any anti-U1 RNP antibodies that have attached to the immobilized antigens.
- A substrate is added that reacts with the enzyme label, producing a measurable signal (e.g., color change) that indicates the presence and quantity of anti-U1 RNP antibodies.
- Immunoblotting (Western Blot): This technique involves separating proteins from a sample using gel electrophoresis and then transferring them onto a membrane. The membrane is then incubated with the patient’s serum to detect antibodies that bind to the U1 snRNP antigens. This method can provide information about the specific antibodies present and their molecular weights.
- Immunoprecipitation: In this method, U1 snRNP antigens are tagged with a solid support and incubated with the patient’s serum. Antibodies that specifically bind to the antigens are captured on the support, and the immune complexes are then isolated. The antibodies are then detected and analyzed to determine their presence and concentration.
- Indirect Immunofluorescence (IIF): IIF is another method used to detect antibodies in patient serum. It involves incubating patient serum with tissue or cell samples that contain U1 snRNP antigens. Fluorescently labeled secondary antibodies are then used to detect any binding of anti-U1 RNP antibodies to the antigens. The pattern of fluorescence can provide additional information about the reactivity of the antibodies.
Sample Collection:
Collect blood in a serum-collection (red-top) tube.
Allow the blood to clot; separate the serum by centrifugation.
Although hemolysis and lipemia do not interfere with this assay, they are best avoided.
Anticoagulants and an elevated bilirubin levels also do not interfere with results.
Specimens may be stored at 2-8°C for up to 5 days or -20°C for up to 6 months.
Clinical Significance and Diagnosis:
The clinical significance of anti-U1 RNP (Ribonucleoprotein) antibodies lies in their association with specific autoimmune diseases and their role in diagnosing and understanding these conditions. Here’s how they are clinically significant and contribute to the diagnosis:
- Diagnostic Marker: The presence of anti-U1 RNP antibodies in a patient’s blood can serve as an important diagnostic marker for certain autoimmune diseases, primarily mixed connective tissue disease (MCTD). Detecting these antibodies can provide strong evidence in support of a diagnosis of MCTD, as they are a characteristic feature of the disease.
- Differentiation of Autoimmune Diseases: Anti-U1 RNP antibodies help distinguish between various autoimmune diseases. Their presence is strongly associated with MCTD and less commonly found in systemic lupus erythematosus (SLE). By identifying these antibodies, healthcare providers can differentiate between these autoimmune conditions and tailor treatment approaches accordingly.
- Clinical Correlation: While the presence of anti-U1 RNP antibodies is significant, it’s important to note that clinical correlation is crucial for diagnosis. This means that healthcare providers consider a patient’s clinical symptoms, medical history, and other laboratory findings alongside the antibody results to arrive at an accurate diagnosis.
- Understanding Disease Mechanisms: Anti-U1 RNP antibodies provide insight into the underlying mechanisms of autoimmune diseases. These antibodies target the U1 snRNP particle, which is essential for proper pre-mRNA splicing. When the splicing process is disrupted, it can contribute to the development of autoimmune responses and tissue damage.
- Predicting Disease Course: In some cases, the presence of anti-U1 RNP antibodies might be associated with specific clinical manifestations within autoimmune diseases. This association can help healthcare providers predict potential disease outcomes and tailor management strategies.
- Monitoring Disease Activity: Tracking the levels of anti-U1 RNP antibodies over time can provide information about disease activity and response to treatment. Changes in antibody levels might correlate with changes in disease symptoms and overall condition.
- Treatment Approach: The presence of these antibodies can influence treatment decisions. For instance, if a patient is diagnosed with MCTD based on anti-U1 RNP antibody presence, healthcare providers can develop a targeted treatment plan to manage the specific symptoms associated with the disease.
A 4-test ENA panel will include:
| Autoantibody Test | Formally Known As |
|---|---|
| Anti-RNP | Anti-U(1)RNP, Anti-Ribonucleoprotein |
| Anti-Sm | Smith Antibody |
| Anti-SS-A (Ro) | Anti-Sjögren Syndrome A |
| Anti-SS-B (La) | Anti-Sjögren Syndrome B |
A 6-test ENA panel will include:
| Autoantibody Test | Formally Known As |
|---|---|
| Anti-RNP | Anti-U(1)RNP, Anti-Ribonucleoprotein |
| Anti-Sm | Smith Antibody |
| Anti-SS-A (Ro) | Anti-Sjögren Syndrome A |
| Anti-SS-B (La) | Anti-Sjögren Syndrome B |
| Anti-Scl-70 | Scleroderma Antibodies; anti-topoisomerase |
| Anti-Jo-1 | Anti-Histidyl Transfer RNA Synthase Antibodies |
When this Test Ordered
An ENA panel is ordered when a person has signs and symptoms that could be due to an autoimmune disorder and has a positive ANA test. The signs and symptoms of autoimmune disorders are highly variable and can affect many different areas of the body. They may include:
- Fever and persistent fatigue
- Muscle pain
- Joint swelling and/or pain
- Skin rash
- Hair loss or loss of scalp hair
- Sensitivity to ultraviolet light
- Raynaud phenomenon
- Protein in the urine (proteinuria)
- Neurologic symptoms such as seizures, depression, psychoses
- Hemolytic anemia (low red blood cell count) or leukopenia (low white blood cell count)
Normal Values:
The normal values for specific ENA (Extractable Nuclear Antigen) antibodies can vary depending on the laboratory performing the tests and the units of measurement used. These values are often reported as “negative” when the antibodies are not detected. However, it’s important to remember that the interpretation of results can be complex and requires clinical context.
Here’s a simplified table of normal values for some ENA antibodies:
| Antibody | Normal Value |
|---|---|
| Anti-Smith (Sm) | Negative |
| Anti-RNP | Negative |
| Anti-SSA (Ro) | Negative |
| Anti-SSB (La) | Negative |
| Anti-Scl-70 (Topo I) | Negative |
| Anti-Jo-1 | Negative |
| Anti-Centromere | Negative |
| Anti-PM-Scl | Negative |
| Anti-Ro52 | Negative |
| Anti-U3RNP | Negative |
| Anti-Th/To | Negative |
Keep in mind that the absence of these antibodies does not necessarily rule out an autoimmune disease, and the interpretation of results should be done by a qualified healthcare professional in the context of your medical history and symptoms. Normal values might differ between labs, and certain antibodies might not be routinely tested in all facilities.
For the most accurate and relevant information, consult your healthcare provider or the specific laboratory where the tests are being conducted.
FAQs:
What are Anti-U1 RNP antibodies?
Anti-U1 RNP antibodies are autoantibodies that target the U1 small nuclear ribonucleoprotein particle, a component of the cellular machinery involved in mRNA splicing.
What is the role of U1 snRNP?
U1 snRNP recognizes the 5′ splice site of introns in pre-mRNA, initiating proper splicing during mRNA maturation.
What diseases are associated with Anti-U1 RNP antibodies?
These antibodies are linked to mixed connective tissue disease (MCTD) and occasionally systemic lupus erythematosus (SLE).
How are Anti-U1 RNP antibodies detected?
They are detected through laboratory tests like ELISA, immunoblotting, immunoprecipitation, and indirect immunofluorescence.
What is the significance of these antibodies in MCTD diagnosis?
Anti-U1 RNP antibodies are a hallmark of MCTD and aid in confirming its diagnosis.
How do these antibodies contribute to autoimmune diseases?
They can disrupt mRNA splicing, generating abnormal proteins and triggering autoimmune responses that damage tissues.
Are Anti-U1 RNP antibodies specific to MCTD?
While primarily associated with MCTD, they can also be found in some SLE cases and other autoimmune conditions.
Do all individuals with these antibodies develop autoimmune diseases?
No, the presence of antibodies does not guarantee disease development; other factors play a role.
Can these antibodies help predict disease progression?
Monitoring antibody levels may offer insights into disease activity and potential outcomes.
Are Anti-U1 RNP antibodies treatable?
The antibodies themselves are not treated directly; management focuses on controlling autoimmune disease symptoms and immune responses.
Do these antibodies vary among individuals?
Yes, individuals may have different levels of antibodies, which can impact disease severity and clinical manifestations.
Are there potential targeted therapies based on these antibodies?
Research into the mechanisms may eventually lead to targeted treatments, but current management focuses on symptom control.
What is the role of clinical correlation in diagnosis?
Clinical correlation involves assessing antibody results alongside symptoms, medical history, and other findings to make an accurate diagnosis.
Conclusion:
In conclusion, Anti-U1 RNP antibodies play a pivotal role in the landscape of autoimmune diseases, notably mixed connective tissue disease (MCTD) and sometimes systemic lupus erythematosus (SLE). Their specific targeting of the U1 small nuclear ribonucleoprotein particle disrupts mRNA splicing, potentially leading to altered protein production and autoimmunity. As diagnostic markers, they aid in confirming MCTD diagnoses and guiding treatment strategies, while also offering insights into disease mechanisms. While further research may unveil targeted therapies, their significance lies in their contribution to understanding autoimmune responses and providing valuable clinical information for patient care.
Possible References Used