Anovulation is a medical term that refers to the absence of ovulation, which is the release of a mature egg from one of the ovaries. Ovulation is a crucial part of the menstrual cycle and is necessary for fertility because it allows for the possibility of fertilization and pregnancy.
Definition of Anovulation.
Anovulation is a medical term used to describe a condition in which a woman’s ovaries do not release a mature egg (ovum) during her menstrual cycle. In a typical menstrual cycle, ovulation is a crucial process where a mature follicle in one of the ovaries ruptures, releasing an egg that can potentially be fertilized by sperm. However, in cases of anovulation, this release of an egg does not occur.
Anovulation can lead to irregular or absent menstrual periods, and it is a common cause of fertility issues in women. It can be caused by various factors, including hormonal imbalances, disorders of the pituitary gland or hypothalamus, stress, extreme changes in body weight, and certain medical conditions such as polycystic ovary syndrome (PCOS). Accurate diagnosis and appropriate treatment are essential for managing anovulation, particularly for women who are trying to conceive.
What is Importance of Ovulation in the Menstrual Cycle?
Here are several key reasons why ovulation is important in the menstrual cycle.
- Fertility: Ovulation is the process by which a mature egg is released from one of the ovaries into the fallopian tube, where it can potentially be fertilized by sperm. Without ovulation, fertilization and conception cannot occur, making ovulation a fundamental step in achieving pregnancy.
- Regularity of Menstrual Cycles: Ovulation helps regulate the menstrual cycle. In a typical 28-day cycle, ovulation usually occurs around the midpoint (around day 14). The hormonal changes associated with ovulation trigger the shedding of the uterine lining during menstruation. Irregular or absent ovulation can lead to irregular menstrual cycles.
- Hormonal Balance: Ovulation is tightly regulated by hormonal signals, primarily involving the interplay between follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone. These hormones not only control ovulation but also maintain the health of the reproductive organs and have broader effects on overall health.
- Estrogen and Progesterone Production: After ovulation, the ruptured follicle transforms into a structure called the corpus luteum, which produces the hormone progesterone. This hormone is essential for preparing the uterine lining for possible implantation of a fertilized egg. Additionally, ovulation leads to increased estrogen levels, which have various effects on the body, including maintaining bone density and cardiovascular health.
- Predictability: For women who are trying to conceive, understanding when ovulation occurs in their menstrual cycle is essential. Tracking ovulation can help them identify their most fertile days, increasing the chances of successful conception.
- Health Monitoring: Regular ovulation is an indicator of overall reproductive health. Irregularities in ovulation may signal underlying health conditions, such as polycystic ovary syndrome (PCOS), thyroid disorders, or hormonal imbalances, which may require medical attention.
- Menopausal Transition: The cessation of ovulation marks the onset of menopause, the natural end of a woman’s reproductive years. Monitoring ovulation patterns can help women understand their transition into this life stage.
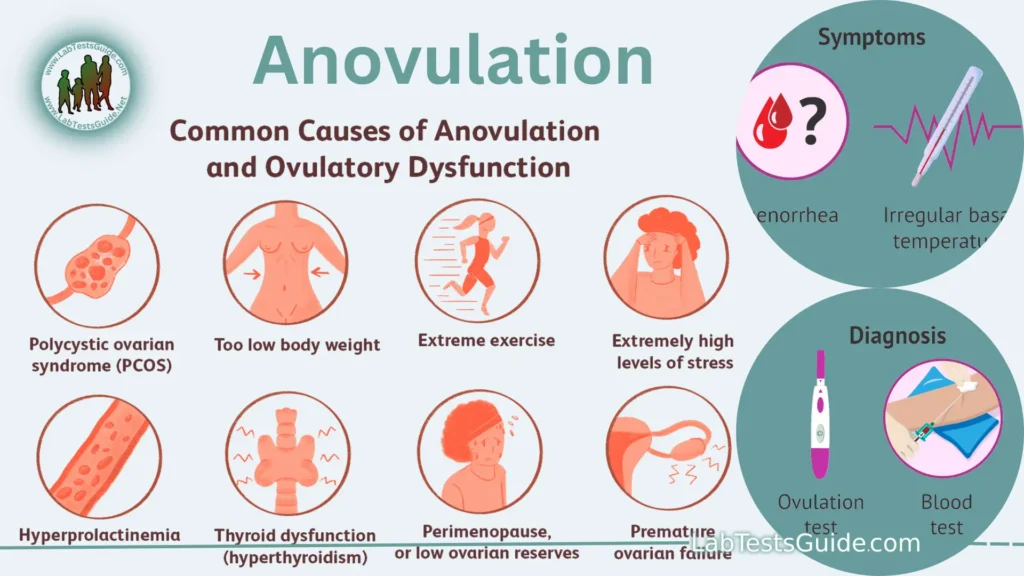
Causes of Anovulation:
Here are some common causes of anovulation.
Hormonal Imbalances:
- Polycystic Ovary Syndrome (PCOS): PCOS is a common cause of anovulation. It is characterized by high levels of androgens (male hormones) in women, insulin resistance, and the presence of multiple small cysts on the ovaries. These factors can disrupt regular ovulation.
- Thyroid Disorders: Conditions like hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid) can affect the balance of hormones necessary for ovulation.
- Hyperprolactinemia: Elevated levels of the hormone prolactin, often due to a pituitary gland disorder, can interfere with ovulation.
Pituitary and Hypothalamic Dysfunction:
- Hypothalamic Amenorrhea: Stress, excessive exercise, or low body weight can disrupt the hypothalamus, a part of the brain that regulates the menstrual cycle, leading to anovulation.
- Pituitary Tumors: Tumors in the pituitary gland can affect the production of hormones like luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which are essential for ovulation.
Weight-Related Factors:
- Extreme Weight Loss: Rapid weight loss, severe calorie restriction, or eating disorders like anorexia nervosa can lead to anovulation. In these cases, the body may prioritize energy conservation over reproductive function.
- Obesity: Excess body fat can disrupt hormonal balance and lead to anovulation. Obesity is often associated with insulin resistance, which further compounds the issue.
Stress:
- Physical and Emotional Stress: High levels of stress, whether due to physical illness, emotional strain, or other factors, can disrupt the normal hormonal signals that trigger ovulation.
Medical Conditions:
- Premature Ovarian Insufficiency (POI): Sometimes referred to as early menopause, POI occurs when the ovaries stop functioning before the age of 40, leading to anovulation.
- Chronic Medical Conditions: Certain chronic illnesses, such as diabetes and autoimmune disorders, can impact hormonal balance and interfere with ovulation.
Medications and Treatments:
- Certain Medications: Some drugs, including certain antidepressants, antipsychotics, and chemotherapy agents, can disrupt ovulation.
- Radiation or Chemotherapy: Cancer treatments can damage ovarian tissue and impair ovulation.
Symptoms and Diagnosis:
Here are the symptoms and methods of diagnosis associated with anovulation.
Symptoms:
Irregular Menstrual Cycles: The most common and noticeable symptom of anovulation is irregular menstrual periods.
These irregularities can manifest as.
- Cycles that are consistently shorter or longer than the usual 21-35 days.
- Skipping menstrual periods (amenorrhea) for several months.
- Unpredictable or inconsistent bleeding.
Abnormal Bleeding:
Women with anovulation may experience abnormal bleeding patterns.
- Heavy menstrual bleeding (menorrhagia).
- Light or scanty periods (oligomenorrhea).
- Spotting between periods.
- Absence of Ovulation Signs: Absence of typical signs of ovulation, such as changes in cervical mucus consistency, a noticeable increase in basal body temperature, or ovulatory pain (mittelschmerz).
- Fertility Challenges: For women trying to conceive, anovulation can lead to difficulty getting pregnant due to the absence of egg release.
Diagnosis:
Medical History and Physical Examination: A healthcare provider will start by taking a detailed medical history, including menstrual history and any underlying medical conditions or medications. A physical examination may also be conducted to check for signs of hormonal imbalances, such as excessive body hair growth (hirsutism) or acne, which may be indicative of conditions like PCOS.
Hormone Blood Tests:
- Progesterone Levels: Measuring progesterone levels in the blood during the luteal phase (the second half of the menstrual cycle) can help confirm ovulation. Low progesterone levels may indicate anovulation.
- Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH): Abnormal levels of these hormones can provide insights into hormonal imbalances that may be causing anovulation.
- Thyroid Hormone Levels: Testing thyroid hormone levels (TSH, T3, T4) can identify thyroid disorders as a potential cause.
- Pelvic Ultrasound: Transvaginal or abdominal ultrasound can be used to visualize the ovaries and the presence of ovarian cysts or follicles. In women with PCOS, multiple small follicles may be visible.
Ovulation Prediction Methods:
- Tracking basal body temperature (BBT) to detect a rise in temperature after ovulation.
- Monitoring cervical mucus changes to identify fertile cervical mucus.
- Using ovulation predictor kits (OPKs) that measure LH surge levels in urine.
- Endometrial Biopsy: In some cases, an endometrial biopsy may be performed to assess the effects of progesterone on the uterine lining, which can help confirm or rule out ovulation.
- Additional Tests: Depending on the suspected cause, additional tests like blood glucose testing (for insulin resistance in PCOS) or imaging studies of the pituitary gland (in cases of suspected pituitary disorders) may be conducted.
Prevention and Management:
Here are some prevention and management approaches.
Prevention:
- Maintain a Healthy Weight: Achieving and maintaining a healthy body weight can help prevent anovulation, especially in cases where obesity or extreme underweight is a contributing factor. A balanced diet and regular exercise can aid in weight management.
- Stress Reduction: Chronic stress can disrupt hormonal balance and contribute to anovulation. Implementing stress management techniques such as relaxation exercises, meditation, yoga, and counseling can be beneficial.
- Regular Exercise: Engaging in regular, moderate-intensity exercise can help regulate menstrual cycles and improve overall health. However, excessive exercise can have the opposite effect, so it’s important to strike a balance.
- Healthy Diet: A nutritious diet with a focus on whole foods, fruits, vegetables, lean proteins, and whole grains can support hormonal balance. In some cases, dietary changes may be recommended to address specific conditions like insulin resistance.
- Limit Alcohol and Caffeine: Excessive alcohol and caffeine consumption can disrupt hormonal balance. Reducing or eliminating these substances may be advisable for some individuals.
- Avoid Smoking and Illicit Drugs: Smoking and drug use can negatively impact fertility and reproductive health. Quitting smoking and avoiding illicit drugs are essential for overall well-being.
Management:
Medical Treatment: The management of anovulation often involves medical intervention tailored to the underlying cause.
- Hormonal therapy, such as birth control pills or hormone replacement therapy, may be prescribed to regulate menstrual cycles.
- Fertility drugs like Clomiphene or Letrozole may be used to induce ovulation in women trying to conceive.
- Medications to address specific hormonal imbalances or underlying medical conditions, such as thyroid disorders, may be prescribed.
- Assisted Reproductive Technologies (ART): In cases of infertility due to anovulation, fertility treatments like intrauterine insemination (IUI) or in vitro fertilization (IVF) may be recommended to increase the chances of conception.
- Lifestyle Modifications: Continuing to make healthy lifestyle choices is essential for managing anovulation and promoting overall reproductive health. This includes maintaining a healthy weight, managing stress, and avoiding excessive alcohol and caffeine.
- Monitoring and Tracking: Women trying to conceive may use methods like ovulation predictor kits (OPKs), tracking basal body temperature (BBT), and monitoring cervical mucus to identify fertile periods and optimize their chances of getting pregnant.
- Regular Medical Checkups: Routine checkups with a healthcare provider are essential for monitoring the progress of treatment, addressing any complications, and ensuring overall health.
- Patient Education and Support: It’s important for individuals with anovulation to educate themselves about their condition, treatment options, and fertility planning. Support groups and counseling can provide emotional support during the journey.
Treatment Options:
Here are various treatment options for anovulation:
Lifestyle Modifications:
- Weight Management: Achieving and maintaining a healthy body weight through diet and exercise can help regulate ovulation. This is particularly important for individuals with obesity or extreme underweight.
- Stress Reduction: Managing stress through relaxation techniques, mindfulness, yoga, or counseling can help restore hormonal balance.
- Dietary Changes: For conditions like insulin resistance or PCOS, dietary modifications may be recommended to improve insulin sensitivity and regulate ovulation.
Medications:
- Oral Contraceptives: Birth control pills can be used to regulate menstrual cycles and provide relief from symptoms like irregular bleeding and hormonal imbalances.
- Fertility Drugs: Medications like Clomiphene citrate, Letrozole, or Gonadotropins can stimulate ovulation in women trying to conceive.
- Hormone Replacement Therapy (HRT): For women with hormonal imbalances, such as those associated with menopause or premature ovarian insufficiency, HRT can help manage symptoms and restore hormonal levels.
- Metformin: This medication is commonly used to improve insulin sensitivity in individuals with PCOS and insulin resistance, which can help regulate ovulation.
Surgical Interventions:
- Ovulation Induction Surgery: Some women with PCOS may benefit from a surgical procedure called ovarian drilling, which can help restore regular ovulation by reducing the number of ovarian cysts.
- Laparoscopic Surgery: In cases where anovulation is due to conditions like endometriosis or fibroids, laparoscopic surgery can be performed to remove or treat the underlying issues.
Assisted Reproductive Technologies (ART):
- Intrauterine Insemination (IUI): IUI involves placing sperm directly into the uterus during a woman’s fertile period to increase the chances of fertilization.
- In Vitro Fertilization (IVF): IVF is a more advanced fertility treatment that involves fertilizing an egg outside the body and transferring the resulting embryo(s) into the uterus.
Hormonal Therapy:
- Progesterone: Progesterone supplementation may be prescribed to regulate menstrual cycles and promote uterine lining development in preparation for pregnancy.
Lifestyle Support:
- Ovulation Monitoring: Tracking ovulation through methods like basal body temperature charting, cervical mucus monitoring, and ovulation predictor kits can help individuals identify their fertile window and optimize conception attempts.
- Counseling and Support Groups: Emotional support and counseling can be valuable for individuals coping with the emotional challenges of anovulation and infertility.
Effects of Anovulation:
Here are some of the effects of anovulation.
- Infertility: One of the most significant effects of anovulation is infertility. Without the release of a mature egg from the ovaries, fertilization cannot occur, making it difficult for women to conceive naturally. Anovulation is a common cause of female infertility.
- Irregular Menstrual Cycles: Anovulation often leads to irregular menstrual cycles. Women with anovulation may experience cycles that are too long, too short, or unpredictable. This can result in difficulty predicting when menstruation will occur, which can be emotionally distressing.
- Amenorrhea: Some women with anovulation may experience amenorrhea, which is the absence of menstrual periods for several months or longer. Prolonged amenorrhea can have implications for bone health and may increase the risk of conditions like osteoporosis.
- Hormonal Imbalances: Anovulation is frequently associated with hormonal imbalances, such as high levels of androgens (male hormones) or insulin resistance. These imbalances can lead to symptoms like hirsutism (excessive body hair growth), acne, and skin changes.
- Polycystic Ovary Syndrome (PCOS): PCOS is a common condition characterized by anovulation, along with other symptoms like irregular periods, ovarian cysts, and hormonal imbalances. It can have broader health effects, including an increased risk of diabetes and heart disease.
- Impact on Fertility Treatments: For women undergoing fertility treatments, anovulation can complicate the process. Treatments like in vitro fertilization (IVF) often rely on controlled ovulation induction, which may be more challenging for women with underlying anovulation issues.
- Emotional and Psychological Effects: The fertility challenges associated with anovulation can have emotional and psychological effects. Dealing with infertility and the uncertainty of conceiving can be emotionally distressing and lead to stress, anxiety, and depression.
- Health Risks: Some of the conditions associated with anovulation, such as PCOS and insulin resistance, can increase the risk of long-term health issues, including type 2 diabetes, cardiovascular disease, and metabolic syndrome.
Fertility and Anovulation:
Here are some key points regarding fertility and anovulation.
- Impact on Fertility: Anovulation disrupts the normal menstrual cycle, leading to irregular or absent menstrual periods. Without ovulation, there is no egg available for fertilization, which significantly reduces the chances of conception. Therefore, anovulation is a common underlying cause of female infertility.
- Primary Cause of Infertility: Anovulation is often the primary cause of infertility in women, accounting for a substantial percentage of cases. Other factors contributing to infertility, such as blocked fallopian tubes or male fertility issues, can sometimes coexist with anovulation.
- Polycystic Ovary Syndrome (PCOS): PCOS is a leading cause of anovulation and infertility. It is characterized by hormonal imbalances, multiple small cysts on the ovaries, and insulin resistance. Women with PCOS often experience irregular menstrual cycles and difficulty conceiving.
- Treatment for Infertility Due to Anovulation: The treatment of infertility caused by anovulation typically involves inducing ovulation. Fertility medications like Clomiphene citrate, Letrozole, or Gonadotropins can stimulate the ovaries to produce and release eggs. Monitoring of the menstrual cycle and ovulation is essential during treatment to time intercourse or fertility procedures correctly.
- Assisted Reproductive Technologies (ART): In cases where medications alone are not effective, advanced fertility treatments such as intrauterine insemination (IUI) and in vitro fertilization (IVF) may be considered. These procedures can help overcome infertility caused by anovulation by bypassing some of the natural barriers to conception.
- Lifestyle Factors: Lifestyle modifications, such as achieving and maintaining a healthy weight, managing stress, and adopting a balanced diet, can play a significant role in restoring regular ovulation and improving fertility in some cases.
- Emotional Impact: Dealing with anovulation and infertility can be emotionally challenging for individuals and couples. The stress and emotional strain associated with fertility struggles should not be underestimated, and seeking support from healthcare providers, counselors, or support groups can be valuable.
- Prognosis: The prognosis for achieving pregnancy in cases of anovulation depends on several factors, including the underlying cause, the effectiveness of treatment, and individual factors. With appropriate medical care and treatment, many women with anovulation can successfully conceive and have healthy pregnancies.
FAQs:
What is anovulation?
Anovulation is a medical term referring to the absence of ovulation, the process where a mature egg is released from the ovaries during the menstrual cycle.
What causes anovulation?
Anovulation can result from various factors, including hormonal imbalances (e.g., PCOS, thyroid disorders), stress, extreme weight changes, pituitary or hypothalamic dysfunction, and certain medications.
What are the common symptoms of anovulation?
Common symptoms include irregular menstrual cycles, absent menstrual periods (amenorrhea), abnormal bleeding, and fertility challenges.
How is anovulation diagnosed?
Diagnosis often involves a medical history, physical examination, hormone blood tests, pelvic ultrasound, ovulation prediction methods (e.g., basal body temperature tracking), and sometimes endometrial biopsy.
Can anovulation be treated?
Yes, anovulation can often be treated. Treatment options include lifestyle modifications, medications to induce ovulation, hormone therapy, and, in some cases, surgery or assisted reproductive technologies (ART).
What is the impact of anovulation on fertility?
Anovulation is a common cause of female infertility because without ovulation, there is no egg available for fertilization.
Is anovulation associated with any specific medical conditions?
Yes, anovulation is associated with conditions like polycystic ovary syndrome (PCOS), thyroid disorders, and premature ovarian insufficiency, among others.
Can lifestyle changes help manage anovulation?
Yes, lifestyle modifications such as achieving a healthy weight, stress reduction, regular exercise, and a balanced diet can help manage anovulation and improve overall reproductive health.
What are the treatment options for infertility due to anovulation?
Treatment options may include fertility medications (e.g., Clomiphene, Letrozole), assisted reproductive technologies (e.g., IUI, IVF), and lifestyle changes.
How can I track my ovulation if I suspect anovulation?
Methods for tracking ovulation include basal body temperature charting, monitoring cervical mucus changes, and using ovulation predictor kits (OPKs).
Are there support groups or counseling available for individuals dealing with anovulation and infertility?
Yes, there are support groups and counseling services that provide emotional and psychological support for individuals and couples facing fertility challenges.
What is the outlook for women with anovulation?
The outlook depends on the underlying cause, the effectiveness of treatment, and individual factors. With appropriate care, many women with anovulation can achieve pregnancy.
Conclusion:
In conclusion, anovulation is a significant and common reproductive issue that can have far-reaching implications for a woman’s health and fertility. It refers to the absence of ovulation, which is the release of a mature egg from the ovaries during the menstrual cycle. Anovulation can result from various factors, including hormonal imbalances, stress, weight-related issues, and medical conditions like polycystic ovary syndrome (PCOS).
Anovulation, characterized by the absence of ovulation, poses significant challenges to women’s reproductive health, impacting menstrual regularity, hormonal balance, and fertility. Its diverse underlying causes demand a multifaceted approach to diagnosis and treatment, encompassing lifestyle adjustments, medications, and, when necessary, advanced reproductive technologies. Recognizing the emotional toll it can take, supportive care and counseling are essential components of managing anovulation. With proper medical intervention and personalized strategies, many individuals facing anovulation can regain control of their reproductive health, optimize fertility, and work towards their family planning goals.
Possible References Used




