Amenorrhea is a medical term used to describe the absence or cessation of menstruation in women of reproductive age. It is not a disease itself but rather a symptom of an underlying condition. There are two main types of amenorrhea. Primary Amenorrhea and Secondary Amenorrhea.

Definition of Amenorrhea:
Amenorrhea is a medical term used to describe the absence or cessation of menstrual periods in women of reproductive age. It is a condition in which a woman does not experience regular menstrual bleeding.
There are two main types:
Primary Amenorrhea: This occurs when a young woman has not experienced her first menstrual period (menarche) by the age of 16, despite other signs of puberty, such as breast development and pubic hair growth.
Secondary Amenorrhea: This type of amenorrhea refers to the absence of menstrual periods in a woman who has previously had regular menstrual cycles. Secondary amenorrhea is diagnosed when a woman misses her periods for three or more consecutive cycles or six months if she has previously had irregular cycles.
Causes of Amenorrhea:
Here are some common causes of amenorrhea.
- Pregnancy: The most common cause of amenorrhea is pregnancy. Once a woman becomes pregnant, her menstrual periods naturally stop until after childbirth.
- Hormonal Imbalances: Disruptions in the hormonal regulation of the menstrual cycle can lead to amenorrhea. Imbalances in hormones like estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) can affect ovulation and menstruation.
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder characterized by enlarged ovaries with multiple small cysts. It can cause irregular or absent menstrual periods due to hormonal imbalances.
- Thyroid Disorders: An overactive thyroid (hyperthyroidism) or underactive thyroid (hypothyroidism) can interfere with the menstrual cycle and cause amenorrhea.
- Hypothalamic Amenorrhea: Stress, excessive exercise, rapid weight loss, or eating disorders can disrupt the hypothalamus, a part of the brain that regulates hormones, leading to amenorrhea.
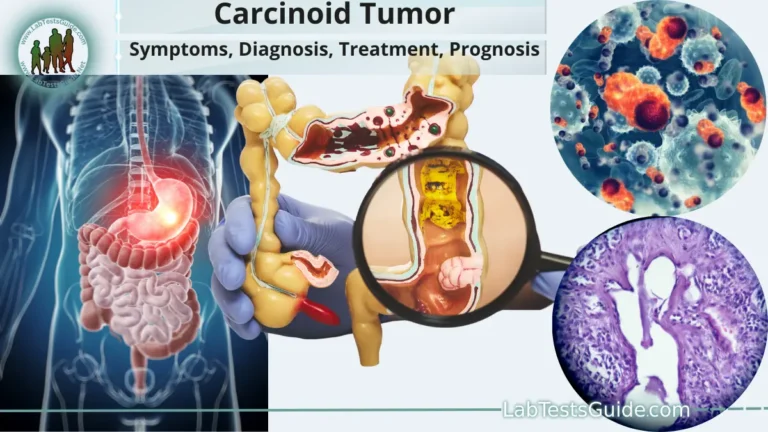
- Pituitary Disorders: Tumors or other abnormalities in the pituitary gland can affect the secretion of hormones that regulate the menstrual cycle.
- Premature Ovarian Insufficiency (POI): Also known as premature menopause, POI occurs when the ovaries stop functioning before the age of 40, leading to amenorrhea and infertility.
- Medications: Certain medications, such as hormonal contraceptives (when used continuously), antipsychotics, chemotherapy drugs, and some antidepressants, can cause amenorrhea as a side effect.
- Anatomical Abnormalities: Structural issues in the reproductive organs, such as congenital abnormalities or scarring from surgery or infections, can hinder normal menstrual function.
- Chronic Medical Conditions: Certain chronic conditions, such as Cushing’s syndrome, diabetes, and certain autoimmune diseases, can disrupt hormonal balance and cause amenorrhea.
- Asherman’s Syndrome: This condition is characterized by the formation of scar tissue within the uterus, often resulting from previous uterine surgery or infections, leading to menstrual abnormalities or amenorrhea.
- Genetic and Chromosomal Abnormalities: Some genetic conditions, such as Turner syndrome, can be associated with primary amenorrhea due to abnormal development of the ovaries.
Symptoms and Diagnosis:
These symptoms can vary from person to person and may include.
- Absence of menstrual bleeding: The hallmark symptom of amenorrhea is the absence of menstrual periods for an extended period.
- Changes in breast and body hair: In some cases, changes in breast size and the distribution of body hair may be observed, particularly if the cause is related to hormonal imbalances.
- Headaches or vision changes: If amenorrhea is caused by a pituitary disorder or tumor, headaches and visual disturbances may occur due to the impact on the pituitary gland.
- Vaginal dryness: Decreased estrogen levels may lead to vaginal dryness or discomfort during intercourse.
- Hot flashes: Hormonal imbalances, such as those seen in premature ovarian insufficiency or menopause, can cause hot flashes.
- Changes in libido: A decrease in sex drive may be associated with hormonal disruptions.
Diagnosis of Amenorrhea:
Diagnosing the underlying cause of amenorrhea involves a comprehensive evaluation by a healthcare professional.
The diagnostic process typically includes the following.
- Medical History: The doctor will inquire about the patient’s menstrual history, medical history, medications, exercise routine, and any symptoms or changes in health.
- Physical Examination: A physical examination may be performed to assess signs of hormonal imbalances, such as changes in body hair or breast development.
- Hormone Testing: Blood tests may be conducted to measure hormone levels, including estrogen, progesterone, FSH, LH, thyroid hormones, and prolactin. These tests help identify hormonal imbalances and potential causes of amenorrhea.
- Pregnancy Test: A pregnancy test is usually the first step in evaluating amenorrhea to rule out pregnancy as the cause.
- Imaging Studies: In certain cases, imaging studies like pelvic ultrasound or MRI may be ordered to assess the reproductive organs and identify any structural abnormalities.
- Ovarian Reserve Testing: For women with suspected premature ovarian insufficiency, testing may be done to evaluate the quantity and quality of remaining eggs in the ovaries.
- Gonadotropin-Releasing Hormone (GnRH) Stimulation Test: This test may be used to differentiate between hypothalamic and pituitary causes of amenorrhea.
- Hysteroscopy or Hysterosalpingography: These procedures involve the insertion of a thin, flexible tube with a camera into the uterus (hysteroscopy) or injection of contrast dye into the uterus and fallopian tubes (hysterosalpingography) to examine the uterine cavity and check for structural abnormalities.
Prevention of Amenorrhea
Here are some preventive measures.
- Balanced Diet: Eating a well-balanced diet that includes a variety of nutrients is essential for hormonal balance and overall health. Adequate intake of vitamins, minerals, proteins, healthy fats, and carbohydrates supports normal hormone production and function.
- Manage Stress: Chronic stress can disrupt the hypothalamic-pituitary-ovarian axis, leading to hormonal imbalances and amenorrhea. Practicing stress-reducing techniques such as yoga, meditation, mindfulness, and regular exercise can be beneficial.
- Maintain Healthy Body Weight: Both excess body weight (obesity) and very low body weight (underweight) can contribute to hormonal imbalances and amenorrhea. Maintaining a healthy weight through balanced nutrition and regular exercise is important for reproductive health.
- Exercise Moderately: While regular exercise is essential for overall health, excessive and intense exercise can negatively affect the menstrual cycle. Strive for a balanced exercise routine that includes both cardiovascular activities and strength training without overdoing it.
- Avoid Excessive Alcohol and Substance Use: Alcohol and certain drugs can disrupt hormonal balance and interfere with the menstrual cycle. Avoid excessive alcohol consumption and illegal drug use.
- Regular Check-ups: Regular visits to a healthcare provider can help detect and address any underlying health issues that may affect menstrual regularity.
- Birth Control and Hormonal Methods: Some women may choose to use hormonal birth control methods (e.g., oral contraceptives, patches, or hormonal IUDs) to regulate their menstrual cycles. However, it’s essential to discuss the options and potential side effects with a healthcare professional.
- Timely Management of Underlying Health Conditions: If you have underlying medical conditions like thyroid disorders or polycystic ovary syndrome (PCOS), it’s crucial to follow your doctor’s recommendations and treatment plan to manage these conditions effectively.
- Avoid Smoking: Smoking can impact reproductive health and hormonal balance, so quitting smoking or avoiding exposure to secondhand smoke is beneficial.
Treatment and Management:
Here are some common approaches for treating and managing amenorrhea.
- Hormone Therapy: In cases where hormonal imbalances are the cause of amenorrhea, hormone replacement therapy (HRT) may be prescribed. HRT can help regulate the menstrual cycle and restore normal hormone levels. It can involve taking estrogen, progesterone, or a combination of both, depending on the specific hormonal deficiencies.
- Weight Management: For individuals with amenorrhea related to weight issues, achieving and maintaining a healthy body weight through proper nutrition and regular exercise can help restore regular menstrual cycles.
- Addressing Underlying Medical Conditions: If amenorrhea is caused by certain medical conditions like thyroid disorders or polycystic ovary syndrome (PCOS), managing and treating these conditions can often lead to the return of regular menstrual periods.
- Fertility Treatment: For women who desire to become pregnant, fertility treatments such as ovulation induction with medications, intrauterine insemination (IUI), or in vitro fertilization (IVF) may be recommended in certain cases of infertility-related amenorrhea.
- Surgical Interventions: In some instances, surgical procedures may be required to address structural abnormalities in the reproductive organs, such as removing uterine adhesions or cysts.
- Lifestyle Changes: Adopting a healthy lifestyle that includes a balanced diet, stress management, and moderate exercise can support hormonal balance and menstrual regularity.
- Psychological Support: For cases of amenorrhea related to stress, eating disorders, or emotional factors, counseling or therapy may be beneficial to address underlying psychological issues.
- Medication Adjustment: If amenorrhea is caused by certain medications, the healthcare provider may consider adjusting the dosage or switching to alternative medications with fewer adverse effects on the menstrual cycle.
- Fertility Preservation: In cases of premature ovarian insufficiency or other conditions that may lead to infertility, women may consider fertility preservation options, such as egg or embryo freezing, to preserve the possibility of future pregnancy.
Complications and Outlook:
Here are some potential complications and outlook for individuals with amenorrhea.
- Infertility: For women who desire to become pregnant, certain causes of amenorrhea can significantly impact fertility. If the underlying condition affects ovulation or disrupts the menstrual cycle, it may hinder natural conception. Timely diagnosis and appropriate management can increase the chances of restoring fertility in some cases.
- Osteoporosis: Prolonged amenorrhea, especially if caused by hormonal imbalances or premature ovarian insufficiency, can lead to decreased estrogen levels. Low estrogen levels can contribute to decreased bone density, increasing the risk of osteoporosis and fractures over time.
- Cardiovascular Health: Estrogen plays a protective role in cardiovascular health. Reduced estrogen levels due to amenorrhea may increase the risk of certain cardiovascular conditions if left unaddressed.
- Psychological Effects: Amenorrhea, especially when related to eating disorders or stress, can have significant psychological impacts. Women may experience emotional distress, anxiety, or depression. Addressing the underlying psychological factors through counseling or therapy can be essential for improving mental well-being.
- Hormonal Imbalances: Chronic amenorrhea caused by hormonal imbalances can have broader effects on the endocrine system. Hormones play a crucial role in regulating various bodily functions, and disruptions can lead to other health issues.
Outlook:
- The outlook for amenorrhea varies depending on the underlying cause and how it is managed. In some cases, amenorrhea may be temporary, such as when it occurs due to stress, excessive exercise, or certain medications. Once these factors are addressed, the menstrual cycle may return to normal.
- For other causes of amenorrhea, such as premature ovarian insufficiency or certain structural abnormalities, the outlook for restoring regular menstrual cycles may be more challenging. However, with proper medical management, lifestyle adjustments, and support, many women can lead healthy lives despite amenorrhea.
FAQs:
What is amenorrhea?
Amenorrhea is a medical term used to describe the absence or cessation of menstrual periods in women of reproductive age. There are two main types: primary amenorrhea (no menstruation by age 16) and secondary amenorrhea (absence of periods in a woman who previously had regular cycles).
What are the common causes of amenorrhea?
Amenorrhea can be caused by various factors, including pregnancy, hormonal imbalances, polycystic ovary syndrome (PCOS), thyroid disorders, excessive exercise, stress, certain medications, pituitary disorders, and structural abnormalities in the reproductive organs.
Is amenorrhea a sign of infertility?
In some cases, amenorrhea can be associated with infertility, especially if it is caused by issues with ovulation or hormonal imbalances. However, the relationship between amenorrhea and infertility varies depending on the underlying cause and individual factors. Timely diagnosis and appropriate management can help address fertility concerns in some cases.
When should I seek medical attention for amenorrhea?
If you experience irregular menstrual cycles or the absence of periods, especially if it persists for several months, it’s essential to consult a healthcare professional. Seeking medical attention can help identify the underlying cause and determine appropriate treatment or management.
Can stress cause amenorrhea?
Yes, chronic stress can disrupt the hormonal balance and the hypothalamic-pituitary-ovarian axis, leading to amenorrhea. Stress reduction techniques and lifestyle changes can be beneficial in managing stress-related amenorrhea.
How is amenorrhea diagnosed?
Amenorrhea is diagnosed through a combination of medical history, physical examination, and various tests, including hormonal analysis, pregnancy tests, imaging studies, and other specialized tests based on the suspected cause.
Can amenorrhea be treated?
The treatment of amenorrhea depends on the underlying cause. Hormone therapy, lifestyle changes, addressing medical conditions, and fertility treatments may be employed to manage amenorrhea effectively.
Is amenorrhea reversible?
The reversibility of amenorrhea depends on its cause. In some cases, amenorrhea can be reversed with appropriate treatment, especially if it is due to factors like stress, excessive exercise, or certain medications. However, some causes, such as premature ovarian insufficiency or certain structural abnormalities, may have more limited reversibility.
Does birth control cause amenorrhea?
Certain types of birth control, such as hormonal contraceptives taken continuously or long-term, can lead to amenorrhea as a side effect. However, not all forms of birth control cause amenorrhea, and the absence of periods while using birth control should be discussed with a healthcare provider.
Can amenorrhea lead to health complications?
Untreated or chronic amenorrhea can lead to potential health complications, including infertility, osteoporosis (bone loss), cardiovascular issues, and psychological effects due to hormonal imbalances.
Conclusion:
In conclusion, amenorrhea, the absence or cessation of menstrual periods, can result from various factors, including hormonal imbalances, medical conditions, stress, and lifestyle choices. While amenorrhea itself is not a disease, it can be a symptom of underlying health issues. Early diagnosis, appropriate treatment, and lifestyle modifications are crucial in managing amenorrhea effectively and preventing potential complications. Seeking medical attention and understanding the individual’s unique circumstances are essential steps towards improving reproductive health and overall well-being for women experiencing amenorrhea.
Possible References Used