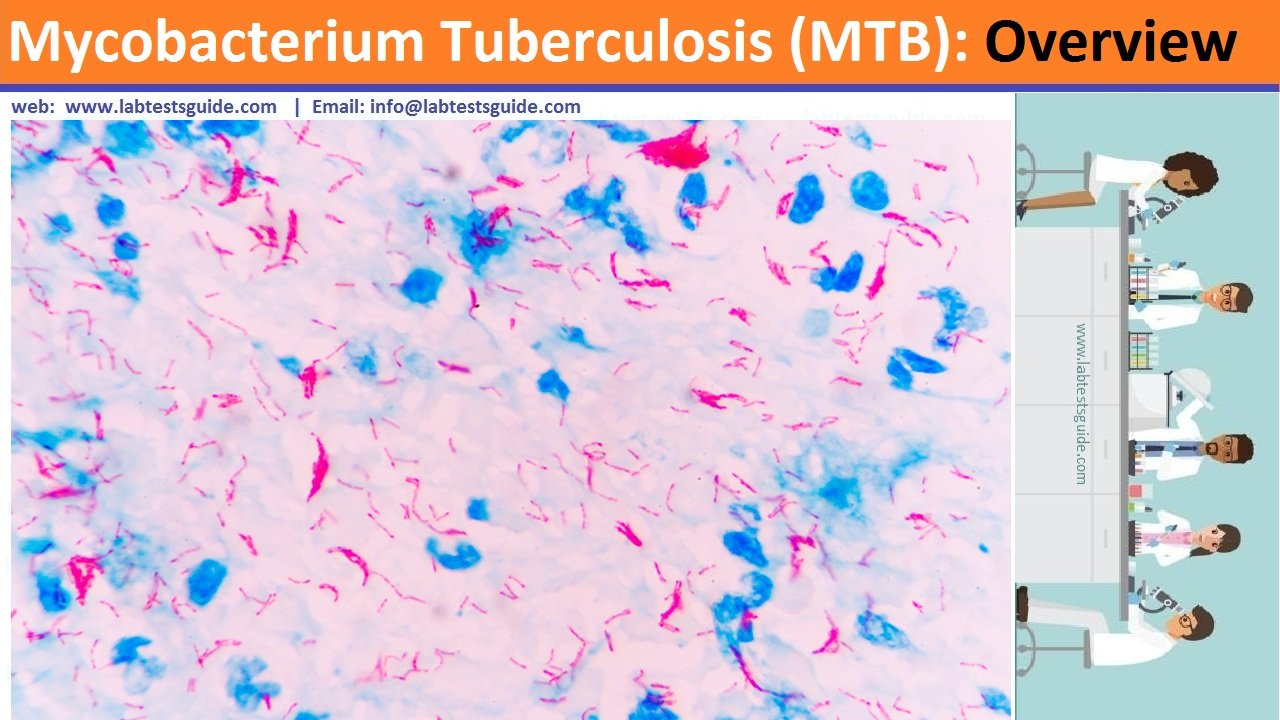
Mycobacterium Tuberculosis (MTB)has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear either Gram-negative or Gram-positive. Acid-fast stains such as Ziehl-Neelsen, or fluorescent stains such as auramine are used instead to identify M. tuberculosis with a microscope. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs. The most frequently used diagnostic methods for tuberculosis are the tuberculin skin test, acid-fast stain, culture, and polymerase chain reaction.
Important Facts
- Mycobacterium tuberculosis is the causative agent.
- It is estimated that 20 to 43 % of the world population is suffering from TB.
- In the USA 15 million people are infected (Old statics).
- TB occurs in :
- Poor community, considered to be the disease of poor people.
- Malnourished people.
- Homeless.
- Overcrowded community.
- Substandard housing.
- Mode of spread: This is an airborne disease.
- Primary TB = Clinically and radiologically is silent.
- Latent TB = Do not have active disease and can not spread the disease to others.
- Active TB = 10% of the latent TB develop active TB when not given treatment.
- Progressive primary TB = 5 % of the primary active TB with sign and symptoms.
- This is thought that 90% of the disease is a reactivation of latent TB.
Sign and Symptoms
- The patient will have :
- Malaise.
- Anorexia.
- Weight loss.
- Fever.
- Night sweating.
- A chronic cough is the common presentation of pulmonary TB.
- Blood streaked sputum is common.
- The patient may have hemoptysis.
- Rarely patients are asymptomatic.
- In advanced disease:
- There may be clubbing of nails.
- Enlarged lymph nodes in the neck.
- The patient may develop a pleural effusion.
Laboratory diagnosis
- Definite diagnosis depends upon the demonstration of T.Bacilli by:
- Culture.
- Culture on solid media needs 12 weeks.
- Culture on liquid media needs several days.
- PCR by DNA or RNA amplification method.
- Sputum, three consecutive sample is recommended for:
- Fluorochrome staining with rhodamine-auramine.
- AFB stain or Ziehl-Neelsen stain.
- Early morning specimen is recommended.
- Bronchoscopy is advised for bronchial washing in case of negative sputum.
- Transbronchial lung biopsy increases the diagnostic yield.
- Gastric aspiration. Early morning sample is an alternative to bronchoscopy.
- Blood culture, 15 % of the case may give a positive culture to T.bacilli.
- Sensitivity should be done once the culture is positive.
- Sensitivity should be done if the sputum culture is positive after the treatment for 2 months.
- Needle biopsy of the pleura shows the granulomas in 60 % of the cases.
- Pleural fluid cultures are positive in < 25 % of the cases.
- Radiology, X-ray chest shows small homogenous opacity.
- Mantoux test or Tuberculin test (TT).
- TT will not distinguish between latent or active TB.
- 0.1 ml (5 tuberculin units) of PPD should be injected intradermally.
- The best site is the volar surface of the arm.
- Injected with 27 G needle.
- Read after 48 to 72 hours for induration (thickening of the injected area).
- It takes 2 to 10 weeks to develop an immune response to PPD after the infection.
- Other specimens can also be used are:
- Urine. The first-morning clean catch is collected for three consecutive days.
- Stool. This should be collected in a clean sterile container.
- Blood. Lysed centrifuged blood is used for culture.
- Niacin test. Mycobacterium produces Niacin. This can be tested by commercially available kits.





0 Comments