Mycobacteria are a group of bacteria that includes various species, some of which can cause diseases in humans and animals, such as tuberculosis and leprosy. Mycobactria Culture involves growing these bacteria in a controlled laboratory environment to study their characteristics, behaviors, and potential applications.

Purpose of Mycobactria Culture Test:
- Diagnosis of Tuberculosis (TB): Mycobacteria culture tests are essential for diagnosing TB infections. They help identify the presence of Mycobacterium tuberculosis, the bacterium responsible for TB, in patient samples like sputum, blood, or tissue.
- Drug Sensitivity Testing: Mycobacteria culture tests determine the sensitivity of the isolated strains to various antibiotics. This information guides physicians in prescribing the most effective treatment regimen for TB and other mycobacterial infections.
- Monitoring Treatment Progress: By culturing samples from patients undergoing treatment, healthcare providers can track the reduction of mycobacterial load over time. This helps assess the effectiveness of the prescribed antibiotics.
- Detection of Atypical Mycobacteria: Mycobacteria culture tests aid in identifying non-tuberculous mycobacteria (NTM) species that can cause opportunistic infections, particularly in individuals with weakened immune systems.
- Confirmation of Leprosy: Culturing samples can confirm the presence of Mycobacterium leprae, the bacterium causing leprosy. This is crucial for diagnosing and managing this chronic infectious disease.
- Epidemiological Studies: Mycobacteria culture tests are used to track the prevalence and distribution of different mycobacterial species within populations, helping researchers understand transmission patterns.
- Research and Vaccine Development: Culturing mycobacteria is vital for studying their biology, genetics, and potential targets for drug development. It also supports research into developing vaccines against TB and other mycobacterial diseases.
- Public Health Surveillance: Monitoring mycobacterial strains helps public health agencies identify outbreaks, understand antimicrobial resistance trends, and implement appropriate control measures.
- Confirmation of Active vs. Latent TB: Culture tests distinguish between active TB infections (with actively replicating bacteria) and latent TB infections (bacteria are present but not actively causing symptoms).
- Patient Isolation and Infection Control: Identifying mycobacterial infections through culture tests enables healthcare facilities to implement isolation protocols, reducing the risk of spreading these contagious diseases.
- Forensic Investigations: Mycobacteria culture can be used in forensic investigations to identify possible sources of infection and trace transmission pathways in outbreaks.
- Veterinary Medicine: Mycobacteria culture tests are employed in veterinary medicine to diagnose mycobacterial infections in animals, particularly in livestock.
Classification and Types:
| Classification | Key Types | Description |
|---|---|---|
| Genus | Mycobacterium | The genus name encompassing all mycobacterial species. |
| Pathogenic Species | M. tuberculosis | Causes tuberculosis (TB), a serious respiratory disease. |
| M. leprae | Causes leprosy (Hansen’s disease), affecting skin and nerves. | |
| M. ulcerans | Causes Buruli ulcer, a skin disease leading to tissue destruction. | |
| Non-Tuberculous Mycobacteria (NTM) | M. avium-intracellulare complex | Associated with lung and systemic infections, particularly in immunocompromised individuals. |
| M. abscessus | Commonly causes skin, lung, and soft tissue infections. | |
| M. kansasii | Causes lung infections similar to TB in certain regions. | |
| M. fortuitum | Found in soil and water, causing skin and soft tissue infections. | |
| Environmental Mycobacteria | M. smegmatis | Used in research as a model organism; not typically pathogenic to humans. |
| M. chelonae | Can cause skin and soft tissue infections; found in soil and water. | |
| Rapid Growers | M. chelonae | Rapidly growing mycobacteria associated with wound and surgical site infections. |
| M. fortuitum | Common cause of post-surgical and catheter-related infections. |
Applications of Mycobactria Culture Test:
- Tuberculosis Diagnosis: Mycobacteria culture tests are crucial for confirming the presence of Mycobacterium tuberculosis, the bacterium responsible for tuberculosis (TB). This aids in accurate diagnosis and appropriate treatment planning.
- Drug Susceptibility Testing: Culture tests determine the susceptibility of the isolated mycobacterial strains to various antibiotics. This helps guide effective treatment regimens, especially important due to the rise of drug-resistant TB strains.
- Monitoring Treatment Efficacy: Culturing samples at different treatment stages allows healthcare professionals to assess the effectiveness of prescribed antibiotics by tracking the reduction in mycobacterial load.
- Non-Tuberculous Mycobacteria (NTM) Infections: Culture tests help diagnose and manage infections caused by non-TB mycobacteria, which can affect immunocompromised individuals or those with underlying health conditions.
- Leprosy Diagnosis: Mycobacteria culture tests aid in confirming the presence of Mycobacterium leprae, which causes leprosy or Hansen’s disease. This supports accurate diagnosis and proper treatment.
- Research and Drug Development: Culturing mycobacteria provides researchers with live samples for studying their biology, genetics, and potential targets for drug development against TB and related diseases.
- Epidemiological Studies: Mycobacteria culture data contribute to understanding disease prevalence, distribution, and transmission patterns, aiding in designing effective control measures.
- Distinguishing Active and Latent TB: Culture tests help differentiate between active TB infections (with actively replicating bacteria) and latent TB infections (bacteria are present but not causing symptoms), assisting in patient management.
- Infection Control Measures: Identifying mycobacterial infections through culture tests enables healthcare facilities to implement isolation protocols, reducing the risk of disease transmission.
- Public Health Surveillance: Mycobacteria culture tests contribute to surveillance efforts by identifying outbreaks, tracking antimicrobial resistance trends, and informing public health policies.
- Forensic Investigations: Mycobacteria culture can be used in forensic investigations to trace sources of infection, especially in outbreaks or cases involving multiple individuals.
- Veterinary Medicine: Mycobacteria culture tests are employed in diagnosing mycobacterial infections in animals, particularly in livestock, aiding in animal health management.
Mycobacterial Culture Specimins:
Mycobacterial culture specimens are samples collected from patients or environments that are used to initiate the process of growing mycobacteria in a laboratory setting. These specimens are critical for diagnosing mycobacterial infections and studying the behavior of these bacteria. Here are some common types of mycobacterial culture specimens:
- Respiratory Specimens:
- Sputum: Mucus and saliva coughed up from the lungs. Commonly used for diagnosing pulmonary tuberculosis (TB).
- Bronchoalveolar Lavage (BAL) Fluid: Fluid collected from the lungs using a bronchoscope. Useful for investigating respiratory infections.
- Tracheal Aspirates: Samples collected from the trachea, often in ventilated patients with suspected infections.
- Tissue Specimens:
- Biopsies: Tissue samples taken during procedures like bronchoscopy or skin biopsy. Used for diagnosing diseases like TB and leprosy.
- Lymph Node Aspirates: Fluid from swollen lymph nodes. Helpful in diagnosing infections affecting lymph nodes.
- Body Fluids:
- Cerebrospinal Fluid (CSF): Fluid surrounding the brain and spinal cord. Tested to diagnose TB or other mycobacterial infections affecting the central nervous system.
- Pleural Fluid: Fluid around the lungs. Tested for infections like TB and non-tuberculous mycobacterial (NTM) diseases.
- Skin Specimens:
- Skin Scrapings: Used in diagnosing skin-related mycobacterial infections like Buruli ulcer.
- Skin Biopsies: Samples taken from skin lesions to identify mycobacterial involvement.
- Blood:
- Blood Cultures: Rarely used due to the low concentration of mycobacteria in blood, but important in cases of disseminated or systemic infections.
- Urine:
- Urine Cultures: Used in certain cases of mycobacterial infections, such as urinary tract infections caused by NTM.
- Environmental Samples:
- Soil: For culturing environmental mycobacteria and studying their prevalence in different regions.
- Water: In cases of outbreaks related to waterborne mycobacteria.
Mycobacterial Culture Techniques:
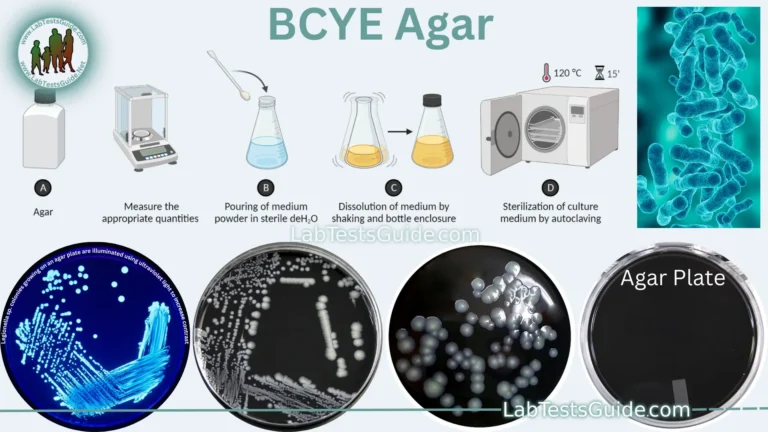
- Solid Culture Media:
- Lowenstein-Jensen Medium: A widely used solid medium for mycobacteria. It contains egg-based nutrients and selective agents to promote mycobacterial growth.
- Middlebrook Agar: Enriched agar media developed for mycobacteria. Variants like 7H10 and 7H11 provide optimal conditions for growth and drug susceptibility testing.
- Liquid Culture Media:
- Middlebrook Broth: Liquid media with nutrients, supplements, and growth factors. Suitable for liquid cultures and rapid growth detection systems.
- Automated Systems:
- BACTEC™ MGIT™ System: A popular automated system that uses liquid media and fluorescence-based technology to monitor growth and detect mycobacterial presence.
- BD BACTEC™ MGIT™ 960 System: A newer version of the MGIT™ system with enhanced features.
- GeneXpert® System:
- A molecular diagnostic platform that uses real-time PCR to rapidly detect and identify Mycobacterium tuberculosis and rifampicin resistance directly from clinical specimens.
- MALDI-TOF Mass Spectrometry:
- Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry can identify mycobacterial species by analyzing unique protein profiles.
- Phage-Based Methods:
- Bacteriophages specific to mycobacteria can be used to isolate and identify different species. The phage infects the bacteria and produces visible plaques on a lawn of mycobacteria.
- Liquid Culture for Slow Growers:
- For slow-growing mycobacteria, liquid culture systems like Middlebrook broth with agitation (shaking) can help enhance growth rates and isolate viable cultures.
- Biofilm Culture:
- Some mycobacteria, like Mycobacterium avium, form biofilms. Specialized culture techniques are used to study biofilm development and drug resistance.
- Solid-State Culture:
- Used for certain environmental mycobacteria, solid-state cultures involve growing bacteria on surfaces like agar sticks or sand.
- Selective Media:
- Media with specific additives or antibiotics to inhibit the growth of contaminating bacteria and promote mycobacterial growth.
- Drug-Containing Media:
- Used to differentiate different mycobacterial species based on their response to specific antibiotics.
Laboratory Safety and Considerations:
Laboratory safety is of paramount importance when working with mycobacteria due to their potential to cause infections. Adhering to strict biosafety measures ensures the protection of laboratory personnel and prevents the accidental spread of mycobacterial infections. Here are some key laboratory safety considerations when working with mycobacteria:
- Biosafety Level (BSL) Classification: Mycobacteria are classified into different biosafety levels based on their pathogenicity and potential to cause harm. Typically, pathogenic mycobacteria like M. tuberculosis are handled at Biosafety Level 3 (BSL-3) or higher.
- Personal Protective Equipment (PPE): Lab personnel should wear appropriate PPE, including lab coats, gloves, masks, and safety goggles, to prevent contact with mycobacteria and aerosols.
- Engineering Controls: Work should be conducted in a certified biosafety cabinet or enclosed space to minimize the risk of contamination and exposure.
- Handling Procedures: All procedures should be performed meticulously to prevent spills and aerosol generation. Pipetting and mixing should be conducted carefully.
- Aerosol Management: Aerosol-generating procedures, such as opening culture plates or tubes, should be done within a biosafety cabinet to prevent the release of infectious particles.
- Decontamination and Disinfection: Surfaces, equipment, and materials that come into contact with mycobacteria should be properly decontaminated using disinfectants effective against mycobacteria.
- Waste Management: Contaminated waste materials should be autoclaved or treated according to appropriate protocols before disposal.
- Training and Education: Laboratory personnel should receive proper training in mycobacterial handling, biosafety procedures, and emergency response protocols.
- Emergency Procedures: Laboratories should have clear protocols for handling accidents, spills, and potential exposures, including access to medical treatment.
- Ventilation and Airflow: BSL-3 laboratories should have controlled ventilation systems to minimize the spread of aerosols and ensure air quality.
- Regulations and Guidelines: Laboratories should adhere to national and international regulations and guidelines for handling mycobacteria and other infectious agents.
- Restricted Access: Access to the laboratory should be restricted to authorized personnel only, and appropriate signage should be posted.
- Medical Surveillance: Laboratory personnel working with mycobacteria should undergo regular medical surveillance to monitor for potential infections or adverse health effects.
Advances in Mycobacteria Culture:
- Automated Culture Systems: Automated systems, such as the BACTEC™ MGIT™ and BD BACTEC™ MGIT™ 960, utilize liquid culture media and fluorescence-based detection for continuous monitoring of mycobacterial growth. These systems provide faster results and reduce the need for manual monitoring.
- Microfluidics and Lab-on-a-Chip: Microfluidic devices and lab-on-a-chip technologies allow for miniaturized and controlled culture environments. These systems enable real-time monitoring, precise manipulation of growth conditions, and even single-cell analysis.
- Alternative Culture Media: Researchers are developing innovative culture media formulations to enhance the growth of slow-growing mycobacteria and improve recovery rates.
- MALDI-TOF Mass Spectrometry: Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry has emerged as a rapid and accurate method for identifying mycobacterial species by analyzing unique protein profiles.
- Molecular Techniques for Drug Susceptibility Testing: Molecular assays can quickly identify drug resistance mutations in mycobacteria, allowing for rapid and targeted treatment decisions.
- Genomic Techniques: Advances in genomics have led to whole-genome sequencing of mycobacterial isolates. This provides insights into genetic diversity, transmission patterns, and drug resistance mechanisms.
- Phage-Based Detection: Phage-based methods are being developed for rapid detection of mycobacteria. Bacteriophages specific to mycobacteria can be used to detect the presence of viable bacteria.
- High-Throughput Screening: Automation and robotics enable high-throughput screening of mycobacterial cultures, allowing for the simultaneous processing of multiple samples and rapid data analysis.
- Point-of-Care Testing: Portable and rapid diagnostic tools are being developed for point-of-care testing. These devices can provide on-the-spot diagnosis and reduce the time to treatment initiation.
- Advanced Imaging Techniques: Techniques like live-cell imaging and advanced microscopy allow researchers to observe mycobacterial growth and interactions with host cells in real time.
- Metabolomics and Proteomics: Metabolomic and proteomic analyses provide insights into the metabolic activities of mycobacteria, aiding in understanding their behavior and response to different conditions.
Clinical Significance of Mycobacteria Culture:
The clinical significance of mycobacteria culture lies in its crucial role in diagnosing and managing mycobacterial infections, which can range from mild to severe diseases. Here’s how mycobacteria culture impacts clinical practice:
- Tuberculosis (TB) Diagnosis and Management: Mycobacteria culture is the gold standard for diagnosing TB. It confirms the presence of Mycobacterium tuberculosis and allows for drug susceptibility testing to determine effective antibiotics. This is vital for appropriate treatment planning and preventing the spread of drug-resistant strains.
- Leprosy Diagnosis: Mycobacteria culture confirms the presence of Mycobacterium leprae in suspected cases of leprosy. Accurate diagnosis enables timely treatment and helps prevent complications.
- Atypical Mycobacterial Infections: Culture tests identify non-tuberculous mycobacteria (NTM) responsible for opportunistic infections in immunocompromised individuals. Proper identification informs treatment choices.
- Monitoring Treatment Efficacy: Culturing mycobacteria during treatment helps assess the effectiveness of prescribed antibiotics by tracking reductions in bacterial load over time.
- Distinguishing Active vs. Latent Infections: Mycobacteria culture aids in differentiating between active and latent TB infections, helping clinicians tailor appropriate treatment strategies.
- Epidemiological Studies and Outbreak Control: Mycobacteria culture data contributes to tracking disease prevalence, transmission patterns, and identifying outbreaks, allowing public health interventions and control measures.
- Development of Targeted Therapies: Mycobacteria culture is essential for researching new drugs and treatments. Understanding bacterial behavior informs the design of targeted therapies.
- Diagnosis in Immune-Compromised Patients: Culture tests aid in diagnosing mycobacterial infections in individuals with weakened immune systems, such as those with HIV/AIDS.
- Confirmation of Environmental Exposures: In cases of environmental mycobacterial infections, culture tests confirm exposure sources, such as water or soil, helping manage and prevent further infections.
- Forensic Investigations: Culture tests can assist in forensic investigations, identifying sources of infections and tracing transmission pathways in outbreaks.
- Research and Vaccine Development: Mycobacteria culture supports research into understanding bacterial biology, genetics, and potential vaccine targets.
- Veterinary Medicine: Culture tests aid in diagnosing mycobacterial infections in animals, which can have implications for animal health and zoonotic transmission.
FAQs:
Q1: What is mycobacteria culture?
A1: Mycobacteria culture involves growing mycobacterial organisms in a controlled laboratory setting to diagnose infections, study their characteristics, and conduct research.
Q2: Why is mycobacteria culture important?
A2: Mycobacteria culture is crucial for diagnosing tuberculosis (TB), atypical mycobacterial infections, and other mycobacterial diseases. It helps determine effective antibiotics and guides patient treatment.
Q3: How is mycobacteria culture performed?
A3: Clinical specimens are collected, decontaminated, and inoculated onto specialized media. The cultures are incubated for weeks to months, and growth is observed and identified.
Q4: What are the types of mycobacteria commonly cultured?
A4: Mycobacterium tuberculosis (causing TB), M. leprae (causing leprosy), and various non-tuberculous mycobacteria (NTM) are commonly cultured.
Q5: What is the purpose of drug susceptibility testing in mycobacteria culture?
A5: Drug susceptibility testing helps determine which antibiotics are effective against mycobacterial strains, guiding appropriate treatment regimens.
Q6: How does mycobacteria culture contribute to public health?
A6: Mycobacteria culture aids in tracking disease prevalence, identifying outbreaks, understanding transmission patterns, and developing effective control measures.
Q7: What biosafety measures are essential for mycobacteria culture?
A7: Biosafety measures include using Biosafety Level 3 (BSL-3) facilities, wearing appropriate PPE, and adhering to strict procedures to prevent laboratory-acquired infections.
Q8: What are the challenges of mycobacteria culture?
A8: Mycobacteria are slow-growing, and culture results take time. Contamination and working with pathogenic strains pose challenges in maintaining safety and accuracy.
Q9: Can mycobacteria culture distinguish between active and latent TB infections?
A9: Yes, mycobacteria culture can differentiate between active infections (with actively replicating bacteria) and latent infections (bacteria are present but not actively causing symptoms).
Q10: How has technology improved mycobacteria culture?
A10: Automation, molecular techniques, high-throughput systems, and advanced imaging have accelerated culture, identification, and drug susceptibility testing processes.
Q11: Can mycobacteria culture be used in veterinary medicine?
A11: Yes, mycobacteria culture tests are used to diagnose mycobacterial infections in animals, particularly livestock.
Q12: What is the role of mycobacteria culture in drug development?
A12: Mycobacteria culture aids in studying bacterial biology, genetics, and drug targets, facilitating the development of new antibiotics and treatments.
Q13: Are there point-of-care mycobacteria culture methods?
A13: While culture methods typically take time, there’s ongoing research into developing point-of-care tests that offer rapid results for specific mycobacterial infections.
Conclusion:
In conclusion, mycobacteria culture is a vital tool in diagnosing mycobacterial infections, studying their behavior, and advancing medical research. This technique’s contributions to accurate diagnoses, effective treatment strategies, and public health efforts are undeniable. With technological advancements, mycobacteria culture has become more efficient, allowing for faster results and deeper insights. However, maintaining strict biosafety measures remains crucial to ensure the safety of laboratory personnel and prevent the spread of infections. Mycobacteria culture continues to shape medical practices, driving progress in the understanding and management of mycobacterial diseases.
Possible References Used