Spontaneous abortion, commonly referred to as a miscarriage, is the natural loss of a pregnancy before the fetus can survive outside the womb. Miscarriages often occur in the early stages of pregnancy, typically within the first 20 weeks, with most happening within the first trimester (first 12 weeks). They can be emotionally and physically challenging for those experiencing them.
Definition of Spontaneous Abortion.
Spontaneous abortion, commonly known as a miscarriage, is a medical term used to describe the natural and involuntary loss of a pregnancy before the fetus reaches a stage of development where it can survive outside the womb. In simpler terms, it refers to the unintentional termination of a pregnancy. A miscarriage typically occurs within the first 20 weeks of gestation, with the majority happening in the first trimester (the first 12 weeks). It can be caused by various factors, including genetic abnormalities, maternal health issues, infections, and other factors, and is often characterized by symptoms such as vaginal bleeding and abdominal cramping. Miscarriages can be emotionally and physically challenging for those who experience them.
Causes of Spontaneous Abortion:
Here are some common causes and contributing factors.
- Chromosomal Abnormalities: The most common cause of miscarriages is genetic or chromosomal abnormalities in the developing embryo or fetus. These abnormalities may prevent the pregnancy from progressing normally. Most chromosomal issues are random events and not related to parental factors.
- Maternal Age: Advanced maternal age, particularly in women over 35, is associated with an increased risk of miscarriage. This is partly because older eggs have a higher chance of having chromosomal abnormalities.
- Maternal Health Conditions: Certain maternal health conditions can increase the risk of miscarriage. These include diabetes, thyroid disorders, autoimmune diseases, and clotting disorders. Poorly managed chronic health conditions may affect the pregnancy.
- Uterine Abnormalities: Structural abnormalities in the uterus, such as fibroids, polyps, or a septum, can interfere with implantation and the ability to carry a pregnancy to full term.
- Infections: Infections of the reproductive organs, such as sexually transmitted infections (STIs) or other bacterial and viral infections, can increase the risk of miscarriage, especially if left untreated.
- Hormonal Imbalances: Hormonal imbalances, including conditions like polycystic ovary syndrome (PCOS) and luteal phase defect, can disrupt the menstrual cycle and implantation, potentially leading to miscarriage.
- Lifestyle Factors: Smoking, alcohol consumption, drug use, and exposure to environmental toxins can increase the risk of miscarriage. It’s advisable for pregnant individuals to avoid these substances.
- Medications and Substances: Certain medications, such as some anti-seizure drugs, and exposure to hazardous substances, including radiation and high levels of caffeine, may contribute to miscarriage.
- Physical Trauma: Severe physical trauma or injury to the abdomen during pregnancy can sometimes result in miscarriage.
- Immune System Issues: Some immune system disorders may increase the risk of miscarriage by affecting the body’s ability to tolerate the developing embryo or fetus.
- Progesterone Insufficiency: Low levels of the hormone progesterone, which plays a crucial role in maintaining pregnancy, can sometimes lead to miscarriage.
Symptoms and Diagnosis:
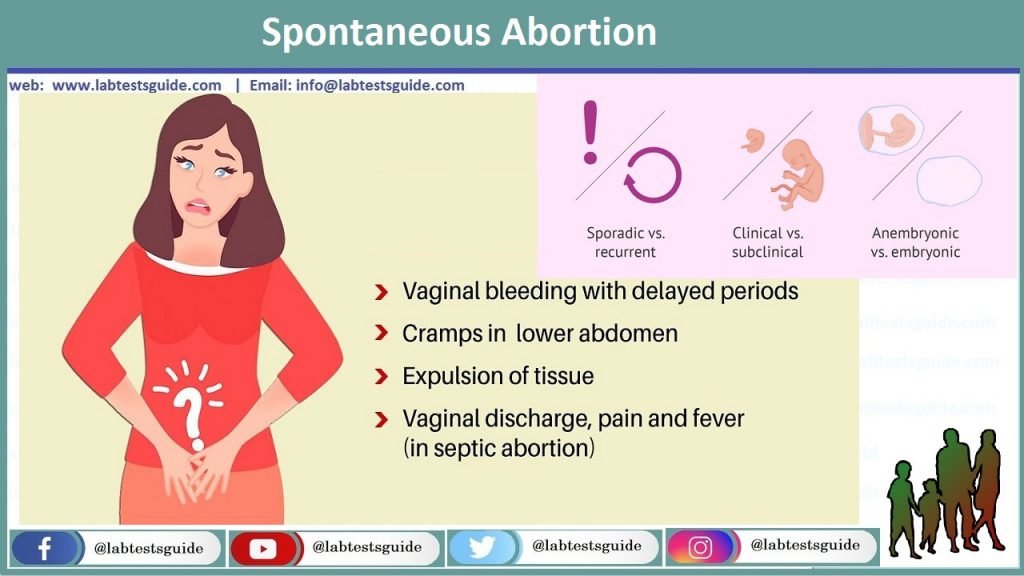
Symptoms of a Miscarriage:
- Vaginal Bleeding: One of the most common signs of a miscarriage is vaginal bleeding. The bleeding can range from light spotting to heavy bleeding, similar to a menstrual period. The color and consistency of the blood can vary.
- Abdominal Cramping: Many individuals experience abdominal cramps or pain, which can range from mild to severe. The cramping may feel similar to menstrual cramps.
- Passing Tissue: In some cases, tissue or clots may pass from the vagina along with the bleeding. This may include recognizable pregnancy tissue or a sac. The appearance can vary widely.
- Back Pain: Some individuals experience lower back pain, which may be associated with the miscarriage.
- Loss of Pregnancy Symptoms: If you were experiencing symptoms of pregnancy, such as breast tenderness or morning sickness, these symptoms may diminish or disappear.
Diagnosis of a Miscarriage:
- Medical History and Physical Examination: When you experience symptoms of a miscarriage, the first step is usually a medical evaluation. Your healthcare provider will take your medical history, including details about your pregnancy, and perform a physical examination.
- Ultrasound: An ultrasound is a common diagnostic tool for confirming a miscarriage. It can detect whether the fetus has a heartbeat and is developing properly. If the ultrasound shows that the fetus is not viable or if there is no fetal heartbeat, it may indicate a miscarriage.
- Blood Tests: Blood tests, specifically measuring the level of human chorionic gonadotropin (hCG), a hormone produced during pregnancy, can help determine if the pregnancy is progressing as expected. A lack of a normal increase in hCG levels may suggest a miscarriage.
- Pelvic Exam: A pelvic exam may be performed to check for signs of bleeding or other abnormalities in the reproductive organs.
- Additional Tests: In some cases, additional tests may be conducted to investigate the cause of the miscarriage. These tests may include genetic testing of fetal tissue, hormone level assessments, and infectious disease screening.
- Serial Monitoring: If there is uncertainty about the viability of the pregnancy, your healthcare provider may recommend serial monitoring of hCG levels and repeated ultrasounds to track the progression.
Prevention and Risk Reduction:
- Preconception Care: Before getting pregnant, it’s beneficial to consult with a healthcare provider for preconception care. This includes a thorough medical evaluation to identify and manage any existing health conditions that may affect pregnancy.
Maintain a Healthy Lifestyle:
- Diet: Consume a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and essential nutrients like folic acid. Avoid excessive caffeine and alcohol.
- Exercise: Engage in regular, moderate exercise to promote overall health. Consult your healthcare provider for exercise recommendations during pregnancy.
- Avoid Smoking and Substance Abuse: Quit smoking and avoid illicit drugs and excessive alcohol consumption, both before and during pregnancy.
- Manage Chronic Health Conditions: If you have chronic health conditions such as diabetes, thyroid disorders, or autoimmune diseases, work closely with your healthcare provider to manage them effectively during pregnancy.
- Prenatal Care: Early and consistent prenatal care is crucial. Attend all scheduled prenatal appointments, as they allow your healthcare provider to monitor your pregnancy and address any potential issues promptly.
- Medication Review: Review any medications you are taking with your healthcare provider. Some medications may need to be adjusted or discontinued during pregnancy, so it’s essential to discuss this with your doctor.
- Genetic Counseling: If you have a family history of genetic disorders or have experienced multiple miscarriages, genetic counseling may be recommended to assess potential genetic factors that could affect your pregnancy.
- Infections: Protect yourself from infections by practicing safe sex to prevent sexually transmitted infections (STIs) and maintaining good hygiene. If you suspect an infection during pregnancy, seek prompt medical attention.
- Environmental Toxins: Minimize exposure to harmful environmental toxins, such as pesticides and chemicals, both at home and in the workplace.
- Stress Reduction: Manage stress through relaxation techniques, counseling, or other stress-reduction strategies. High levels of stress may impact pregnancy outcomes.
- Proper Nutrition and Supplementation: Take prenatal vitamins and supplements, as recommended by your healthcare provider, to ensure you are meeting your nutritional needs during pregnancy. Folic acid is particularly important in early pregnancy to prevent certain birth defects.
- Cervical Health: Cervical insufficiency (an incompetent cervix) can contribute to miscarriages in some cases. If you have a history of cervical insufficiency, your healthcare provider may recommend cervical cerclage, a surgical procedure to reinforce the cervix.
- Avoidance of Trauma: Take precautions to avoid physical trauma or injuries during pregnancy, such as wearing seatbelts correctly, using protective gear, and maintaining a safe environment.
Treatment Options:
Here are the common treatment options.
Expectant Management (No Intervention):
- In some cases, especially for early miscarriages, the body may naturally expel the pregnancy tissue without medical intervention.
- A healthcare provider may recommend close monitoring through follow-up appointments to ensure that the miscarriage is complete.
Medication Management:
- Medications such as misoprostol or mifepristone can be prescribed to help the body expel the pregnancy tissue in cases where expectant management is not progressing or for missed miscarriages.
- These medications can be taken at home or administered in a healthcare setting, depending on the provider’s recommendations.
- It’s essential to follow your healthcare provider’s instructions carefully when using these medications.
Surgical Procedures:
- Surgical intervention is typically recommended for incomplete or inevitable miscarriages, where the body does not expel all of the pregnancy tissue on its own.
- Two common surgical procedures used for miscarriages are:
- Dilation and Curettage (D&C): During a D&C, the cervix is dilated, and the pregnancy tissue is gently scraped or suctioned from the uterus. It is usually performed in a hospital or outpatient surgical center.
- Dilation and Evacuation (D&E): Similar to a D&C but performed later in pregnancy, a D&E involves dilating the cervix and removing pregnancy tissue using suction and medical instruments.
- Surgical procedures are often done under local or general anesthesia.
Hysteroscopy:
- In some cases, a hysteroscopy may be performed to visualize the inside of the uterus and remove any remaining pregnancy tissue.
- This procedure is less common than D&C or D&E but may be recommended in certain situations.
Emotional and Psychological Support:
- Emotional support is a crucial aspect of miscarriage treatment. Many healthcare providers will offer or recommend counseling or support groups to help individuals and couples cope with the emotional aftermath of a miscarriage.
Testing and Evaluation:
- After a miscarriage, healthcare providers may perform tests on the pregnancy tissue to identify any genetic or chromosomal abnormalities that may have contributed to the miscarriage.
- These tests can help provide insight into potential underlying causes, but they may not always yield definitive answers.
Future Pregnancy Planning:
- Following a miscarriage, it’s important to discuss future pregnancy plans with your healthcare provider. They can provide guidance on timing and any additional steps or precautions that may be needed.
Management of Complications:
- In rare cases, complications such as infection or excessive bleeding may arise during or after a miscarriage. Immediate medical attention is necessary if you experience severe pain, heavy bleeding, fever, or other concerning symptoms.
Types of Spontaneous Abortion:
Here are the main types of spontaneous abortion.
Missed Miscarriage (Missed Abortion):
- In a missed miscarriage, the embryo or fetus has stopped developing, but the body does not recognize the loss immediately.
- Symptoms may be absent, or pregnancy symptoms such as breast tenderness and morning sickness may persist.
- Diagnosis is typically made during a routine ultrasound when no fetal heartbeat or growth is detected.
Threatened Miscarriage:
- A threatened miscarriage occurs when there is vaginal bleeding and/or abdominal cramping during pregnancy, but the cervix remains closed.
- The pregnancy may continue without progressing to a complete miscarriage, or it may progress to other types of miscarriage.
Inevitable Miscarriage:
- In an inevitable miscarriage, the miscarriage is in progress, and symptoms such as heavy bleeding and abdominal cramping are present.
- The cervix may begin to dilate (open), and pregnancy tissue may start to pass from the uterus.
Incomplete Miscarriage:
- An incomplete miscarriage occurs when only part of the pregnancy tissue passes from the uterus.
- Symptoms may include heavy bleeding and cramping, and there may be retained tissue in the uterus.
- Medical or surgical intervention is often needed to complete the miscarriage and remove any remaining tissue.
Complete Miscarriage:
- In a complete miscarriage, all of the pregnancy tissue is expelled from the uterus.
- Symptoms such as bleeding and cramping may have been present but have now resolved.
- In some cases, no further intervention is necessary, although follow-up may still be recommended to ensure the uterus is empty.
Recurrent Miscarriage (Recurrent Pregnancy Loss):
- Recurrent miscarriage is defined as the loss of three or more consecutive pregnancies before 20 weeks of gestation.
- It may be associated with underlying factors such as genetic abnormalities, hormonal imbalances, uterine abnormalities, or other health conditions.
Septic Miscarriage:
- A septic miscarriage is a rare but serious complication where an infection occurs in the uterus following a miscarriage.
- Symptoms may include fever, severe abdominal pain, foul-smelling discharge, and a general feeling of illness.
- Immediate medical attention is crucial to treat the infection and prevent complications.
Blighted Ovum (Anembryonic Pregnancy):
- In a blighted ovum, a gestational sac forms in the uterus, but there is no embryo or fetal development.
- It may be diagnosed during an ultrasound when only an empty gestational sac is visible.
Emotional Impact:
Here are some of the common emotional responses and factors associated with the emotional impact of a miscarriage.
- Grief and Loss: Many individuals and couples experience a deep sense of grief and loss after a miscarriage. The loss of a pregnancy can be emotionally akin to losing a loved one, and people may mourn the dreams and expectations they had for their child.
- Sadness and Depression: Feelings of sadness, despair, and depression are common reactions to a miscarriage. These emotions may be especially intense in the days and weeks following the loss.
- Anger and Guilt: Some individuals may experience anger, particularly if they feel that the miscarriage was unjust or unfair. Feelings of guilt can also arise, with individuals questioning whether they did something to cause the miscarriage, even when it’s typically beyond their control.
- Isolation and Loneliness: A miscarriage can sometimes lead to feelings of isolation and loneliness. It may seem like others do not understand the depth of the grief, which can create a sense of emotional isolation.
- Anxiety and Fear: For those who wish to become parents or have experienced multiple miscarriages, anxiety and fear about future pregnancies may be heightened. There may be a constant worry about the possibility of another miscarriage.
- Impact on Relationships: Miscarriages can affect relationships, including those with partners, family members, and friends. Couples may grieve differently, leading to misunderstandings and strain on the relationship.
- Body Image and Self-esteem: Some individuals may experience changes in body image and self-esteem, especially if they blame themselves for the miscarriage or if their bodies underwent physical changes during the pregnancy.
- Coping Mechanisms: People employ various coping mechanisms to deal with the emotional impact of a miscarriage. These may include seeking support from loved ones, participating in counseling or therapy, engaging in rituals to commemorate the loss, or finding solace in creative outlets.
- Time and Healing: Grief and healing do not have a fixed timeline. Some individuals may process their emotions relatively quickly, while others may take much longer to come to terms with their loss.
FAQs:
What is a miscarriage?
A miscarriage, medically known as a spontaneous abortion, is the natural and involuntary loss of a pregnancy before the fetus can survive outside the womb. It often occurs in the early stages of pregnancy.
What are the common signs and symptoms of a miscarriage?
Common signs and symptoms include vaginal bleeding, abdominal cramping or pain, passing of tissue from the vagina, and a decrease or loss of pregnancy symptoms.
What causes a miscarriage?
Miscarriages can be caused by various factors, including chromosomal abnormalities, maternal health conditions, uterine abnormalities, infections, hormonal imbalances, lifestyle factors, and more.
Can miscarriages be prevented?
While not all miscarriages can be prevented, there are steps individuals can take to reduce their risk, such as maintaining a healthy lifestyle, managing chronic health conditions, and avoiding harmful substances during pregnancy.
How is a miscarriage diagnosed?
Diagnosis typically involves a combination of medical history, physical examination, ultrasounds, and blood tests to determine the type and stage of the miscarriage.
What are the different types of miscarriages?
Common types include missed miscarriage, threatened miscarriage, inevitable miscarriage, incomplete miscarriage, complete miscarriage, recurrent miscarriage, and others. Each type has specific characteristics.
What are the treatment options for a miscarriage?
Treatment options depend on the type and stage of the miscarriage. They can include expectant management (no intervention), medication management, surgical procedures (such as D&C or D&E), and emotional support.
How can I cope with the emotional impact of a miscarriage?
Coping strategies may include seeking emotional support from loved ones, joining support groups, participating in counseling or therapy, and allowing yourself time to grieve and heal.
When can I try to conceive again after a miscarriage?
The timing for trying to conceive again varies but is often recommended after the individual’s body has healed physically and they are emotionally ready. Healthcare providers can offer guidance on when it is safe to try again.
Is there a higher risk of future miscarriages after experiencing one?
Not necessarily. Many individuals go on to have successful pregnancies after experiencing a single miscarriage. However, recurrent miscarriages may require additional evaluation and medical intervention.
Are there any risk factors that increase the chances of a miscarriage?
Yes, several factors, such as advanced maternal age, certain health conditions, lifestyle factors like smoking and substance abuse, and previous miscarriages, can increase the risk of miscarriage.
Can a miscarriage be painful?
Yes, miscarriages can be associated with abdominal cramping and pain. The level of pain can vary from mild to severe, depending on the individual and the type of miscarriage.
Conclusion:
In conclusion, spontaneous abortion, commonly known as a miscarriage, is a heartbreaking and emotionally challenging event characterized by the natural loss of a pregnancy before the fetus can survive outside the womb. It can occur for various reasons, many of which are beyond an individual’s control, and its impact is deeply personal. Understanding the causes, types, and emotional consequences of miscarriage is crucial, as is seeking appropriate medical care, emotional support, and time for healing. While miscarriages are a sadly common experience, each journey is unique, and individuals should not hesitate to reach out to healthcare providers, support networks, and resources to navigate the physical and emotional aspects of this difficult loss.
Possible References Used