Fetal distress refers to the compromise of the fetus due to an inadequate supply of oxygen or nutrients. This can occur due to maternal, fetal, or placental factors. In its most severe form, it can lead to neonatal brain injury or fetal death. Its presence can be suspected due to several factors, but all have a high false positive rate.
Definition of Fetal Distress:
Fetal distress is a medical term that refers to a condition in which there are concerns about the well-being of a developing fetus (unborn baby) during pregnancy or labor. It typically indicates that the fetus may not be receiving adequate oxygen or nutrients, which can potentially lead to serious health issues or harm to the fetus if not addressed promptly. Fetal distress is often characterized by specific signs and symptoms, including abnormal fetal heart rate patterns, meconium-stained amniotic fluid, decreased fetal movements, and other indicators that suggest the fetus may be experiencing distress or compromise in its overall health. Prompt medical evaluation and intervention are crucial when fetal distress is suspected to protect the health and safety of both the fetus and the mother.
Causes of Fetal Distress:
Some common causes of fetal distress include.
- Uteroplacental Insufficiency: This occurs when there is inadequate blood flow and oxygen delivery from the mother to the fetus through the placenta. It can result from conditions such as preeclampsia, gestational hypertension, or placental problems (e.g., placental abruption or placenta previa).
- Maternal Health Conditions: Certain maternal health issues can contribute to fetal distress, such as chronic hypertension, diabetes, heart disease, or infections like chorioamnionitis.
- Fetal Factors: Problems related to the fetus itself can lead to distress. These may include congenital abnormalities, genetic conditions, or intrauterine growth restriction (IUGR), where the fetus is not growing at a normal rate.
- Reduced Amniotic Fluid Levels: A decrease in the volume of amniotic fluid (oligohydramnios) can lead to fetal compression and compromise. This can occur due to ruptured membranes (premature rupture of membranes or PROM), post-term pregnancy, or other factors.
- Abnormal Fetal Position: If the fetus is not in the optimal position for birth (e.g., breech presentation), it can lead to complications during labor and potential fetal distress.
- Problems with the Umbilical Cord: Issues such as cord compression or a nuchal cord (when the umbilical cord is wrapped around the baby’s neck) can restrict blood flow and oxygen supply to the fetus.
- Infections: Certain infections, like maternal fever or intrauterine infections, can affect the fetus and lead to distress.
- Multiple Pregnancies: In pregnancies with twins, triplets, or more, there is an increased risk of fetal distress due to the additional strain on the placenta and uterus.
- Drug or Substance Use: Maternal use of certain drugs or substances during pregnancy, including smoking and illegal drugs, can negatively impact fetal health and potentially lead to distress.
- Trauma or Accidents: Traumatic injuries to the mother, such as car accidents or falls, can result in fetal distress if the fetus is affected.
- Fetal Anemia: Conditions that cause fetal anemia, such as Rh incompatibility or other blood disorders, can lead to fetal distress.
Signs and Symptoms of Fetal Distress:
Some common signs and symptoms of fetal distress include.
Abnormal Fetal Heart Rate:
Abnormal heart rate patterns may include:
- Tachycardia: An unusually fast fetal heart rate (above 160 beats per minute).
- Bradycardia: An unusually slow fetal heart rate (below 110 beats per minute).
- Variable Decelerations: Abrupt and variable drops in the fetal heart rate that can be associated with cord compression.
- Late Decelerations: A consistent pattern of delayed decreases in the fetal heart rate after contractions, which may indicate insufficient oxygen supply to the baby.
- Meconium-Stained Amniotic Fluid: Meconium is the first stool passed by a newborn. When it is present in the amniotic fluid before birth, it can be a sign of fetal distress. Meconium-stained amniotic fluid can also increase the risk of respiratory issues for the baby if it is aspirated into the lungs.
- Decreased Fetal Movement: A noticeable decrease in the baby’s movements can be a sign of fetal distress. Monitoring fetal movements is important during pregnancy, and any significant reduction in activity should be reported to healthcare providers.
- Abnormal Contractions: During labor, abnormal contractions that are too frequent, too long, or too strong can reduce blood flow to the placenta and lead to fetal distress. These contractions may be detected through uterine monitoring.
- Changes in Amniotic Fluid Levels: An excessive amount of amniotic fluid (polyhydramnios) or too little amniotic fluid (oligohydramnios) can be a sign of fetal distress. These conditions can affect the baby’s ability to move and can indicate problems with the placenta or fetal development.
- Maternal Symptoms: In some cases, the mother may experience symptoms such as abdominal pain, vaginal bleeding, or high blood pressure, which can be associated with fetal distress.
- Abnormal Fetal Position: If the baby is not in the optimal position for birth, such as a breech presentation or transverse lie, it can be a sign of fetal distress and may require intervention.
Diagnosis of Fetal Distress:
Here are the key components of diagnosing fetal distress.
- Fetal Heart Rate Monitoring: Continuous electronic fetal monitoring is a fundamental tool in diagnosing fetal distress during labor. It involves placing sensors on the mother’s abdomen to track the baby’s heart rate and uterine contractions. The patterns in the fetal heart rate are closely observed for abnormalities, such as tachycardia (too fast), bradycardia (too slow), variable decelerations, or late decelerations.
- Non-Stress Test (NST): A non-stress test is a prenatal test that assesses the fetal heart rate response to the baby’s movements. During an NST, the baby’s heart rate is monitored while the mother is encouraged to report fetal movements. An increase in the heart rate with movement is a reassuring sign of fetal well-being.
- Biophysical Profile (BPP): This test combines fetal heart rate monitoring with an ultrasound to assess various aspects of fetal health. It evaluates fetal breathing movements, fetal movements, fetal muscle tone, amniotic fluid volume, and the non-stress test. Abnormalities in any of these components can indicate fetal distress.
- Doppler Studies: Doppler ultrasound may be used to measure blood flow in the umbilical artery. Changes in the blood flow pattern can provide information about fetal well-being and the potential presence of fetal distress.
- Amniotic Fluid Assessment: Abnormal amniotic fluid levels, such as polyhydramnios (too much) or oligohydramnios (too little), can be assessed through ultrasound. Deviations from normal levels may suggest fetal distress.
- Labor Progress Assessment: Monitoring the progress of labor, including the frequency, duration, and strength of contractions, is essential. Abnormal contractions or prolonged labor can contribute to fetal distress.
- Maternal Symptoms: Healthcare providers also consider any symptoms or conditions experienced by the mother, such as high blood pressure, fever, or vaginal bleeding, as they can be associated with fetal distress.
- Invasive Tests (if indicated): In some cases, additional tests or procedures may be necessary, such as fetal scalp blood sampling or fetal blood gas analysis, to directly assess the baby’s oxygen levels and acid-base status.
Prevention and Risk Reduction:
Here are some strategies for prevention and risk reduction.
- Regular Prenatal Care: Early and consistent prenatal care is essential. Regular check-ups with healthcare providers allow for the early detection and management of conditions that could lead to fetal distress, such as hypertension, diabetes, or infections.
Healthy Lifestyle Choices:
Maintain a healthy lifestyle during pregnancy. This includes.
- Eating a balanced diet rich in nutrients.
- Staying hydrated by drinking plenty of water.
- Avoiding alcohol, tobacco, and illicit drugs.
- Limiting caffeine intake.
- Engaging in regular, moderate exercise with your healthcare provider’s approval.
- Manage Chronic Health Conditions: If you have preexisting health conditions like diabetes or hypertension, work closely with your healthcare team to manage them effectively throughout pregnancy.
- Avoid Environmental Hazards: Minimize exposure to environmental hazards and toxins, such as lead, certain chemicals, and radiation, which can harm fetal development.
- Infections: Practice good hygiene and take steps to prevent infections during pregnancy, as some infections can lead to fetal distress. This includes regular handwashing and avoiding contact with individuals who have contagious illnesses.
- Manage Stress: High levels of stress can impact the health of both the mother and the baby. Find healthy ways to manage stress, such as relaxation techniques, prenatal yoga, or seeking support from a counselor or therapist.
- Monitor Fetal Movements: Pay attention to your baby’s movements. If you notice a significant decrease in fetal movements or patterns that are different from the norm, contact your healthcare provider.
- Stay Hydrated: Proper hydration is crucial during pregnancy. Dehydration can lead to complications, including a reduction in amniotic fluid levels, which can increase the risk of fetal distress.
- Educate Yourself: Attend prenatal classes and educate yourself about the signs and symptoms of fetal distress. Knowing what to look for and when to seek medical attention can be invaluable.
- Positioning During Labor: If you’re experiencing a high-risk pregnancy or have concerns about fetal distress, discuss labor positions with your healthcare provider. Some positions can optimize blood flow and oxygen supply to the fetus.
- Birth Plan: Discuss your birth plan with your healthcare provider and ensure they are aware of any specific concerns or preferences you have regarding labor and delivery.
- Proper Nutrition: Ensure you are getting adequate prenatal vitamins and nutrients to support fetal growth and development.
Treatment and Care of Fetal Distress:
Here are the key aspects of treating and caring for fetal distress.
- Identification and Diagnosis: Healthcare providers use various diagnostic tools, including continuous fetal heart rate monitoring, non-stress tests, ultrasound, and clinical assessments, to identify and diagnose fetal distress.
- Maternal Positioning: In some cases, changing the mother’s position may help alleviate fetal distress. Adjusting the mother’s posture can relieve pressure on the umbilical cord or placenta, improving blood flow to the fetus.
- Oxygen Therapy: Administering oxygen to the mother can increase oxygen levels in her blood, which, in turn, can improve oxygen delivery to the fetus.
- Intravenous (IV) Fluids: IV fluids may be administered to the mother to ensure she is well-hydrated, maintain blood pressure, and improve uterine blood flow, which can benefit the fetus.
- Medications: Depending on the underlying cause of fetal distress, healthcare providers may prescribe medications to address specific issues. For example, tocolytics may be given to reduce uterine contractions if they are contributing to fetal distress.
- Monitoring and Assessment: Continuous monitoring of the fetal heart rate and maternal vital signs is crucial to assess the response to treatment and to detect any further signs of distress.
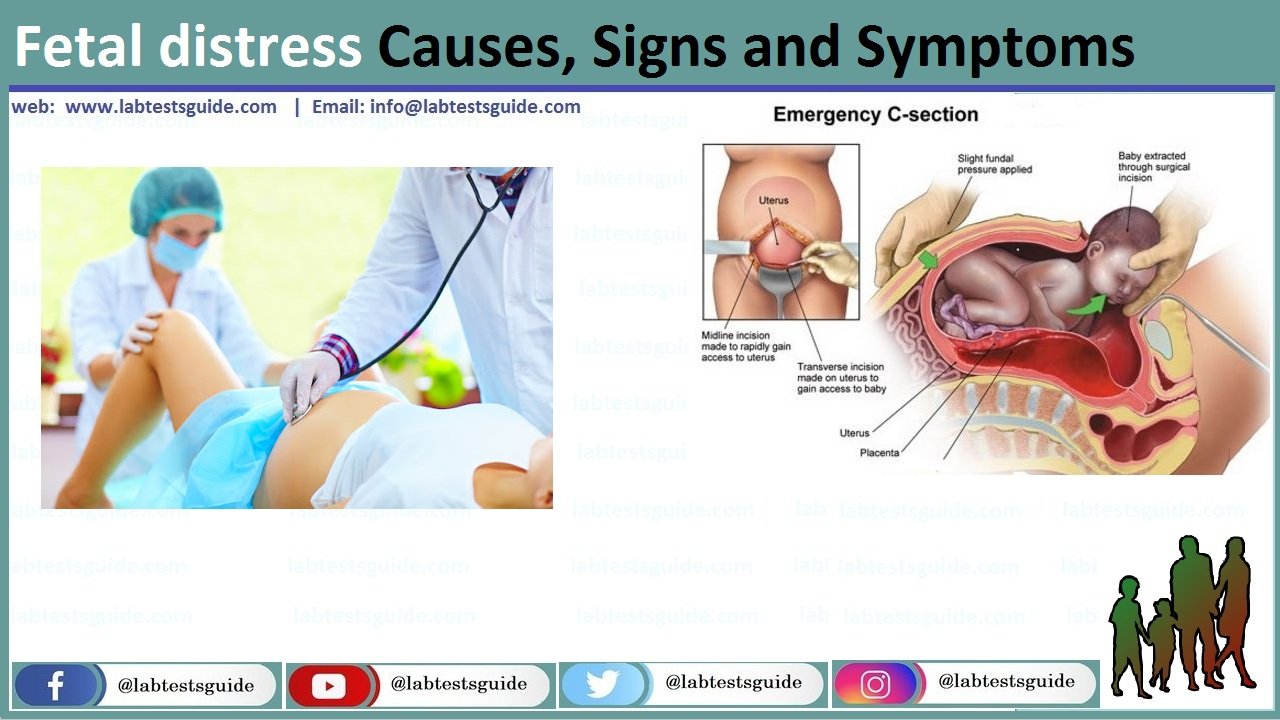
- Emergency Cesarean Section (C-Section): In severe cases of fetal distress or if other interventions are not effective, an emergency C-section may be performed to expedite delivery and protect the baby. This can be a life-saving measure when immediate delivery is necessary.
- Neonatal Intensive Care: If fetal distress results in a premature birth or a baby with health issues, the neonate may require specialized care in a neonatal intensive care unit (NICU) to address any complications and provide support for the baby’s development.
- Support for the Mother: Emotional support and communication with the mother are vital during this stressful time. Healthcare providers should keep the mother informed about the situation, the treatment plan, and the baby’s condition.
- Follow-Up Care: After the baby is born, medical professionals will continue to monitor the baby’s health and address any immediate medical concerns. This includes assessing the baby’s Apgar score and providing necessary medical interventions.
Management and Interventions:
Here are some common management strategies and interventions.
- Immediate Assessment: When fetal distress is suspected, healthcare providers assess the situation promptly. This includes continuous monitoring of the fetal heart rate and uterine contractions, as well as evaluating the mother’s vital signs.
- Maternal Positioning: Changing the mother’s position can sometimes alleviate fetal distress. Adjusting her posture can relieve pressure on the umbilical cord or placenta, potentially improving blood flow to the fetus.
- Oxygen Administration: Providing supplemental oxygen to the mother via a mask or nasal cannula can increase oxygen levels in her blood, which, in turn, can improve oxygen delivery to the fetus.
- Intravenous (IV) Fluids: Administering IV fluids to the mother helps maintain her blood pressure, hydration, and uterine blood flow, which are essential for fetal well-being.
- Tocolytics: If contractions are contributing to fetal distress, tocolytic medications may be administered to reduce uterine contractions and give the baby more time to recover.
- Amnioinfusion: In cases where there is a significant decrease in amniotic fluid (oligohydramnios), amnioinfusion may be performed. This procedure involves injecting sterile fluid into the amniotic sac to improve the cushioning effect around the baby and relieve cord compression.
- Medications: Depending on the cause of fetal distress, healthcare providers may prescribe medications to address specific issues. For example, medications to control maternal blood pressure or manage infections may be administered.
- Emergency Cesarean Section (C-Section): In severe cases of fetal distress or when other interventions are ineffective, an emergency C-section may be recommended to expedite delivery and protect the baby. This is a critical decision made to ensure the baby’s safety.
- Neonatal Resuscitation: If the baby is born with signs of distress, the neonatal care team is prepared to provide immediate resuscitation and medical care to support the baby’s transition to life outside the womb.
- Continuous Monitoring: Throughout the management process, healthcare providers continue to monitor the fetal heart rate, maternal vital signs, and the overall response to interventions. Adjustments may be made as needed.
- Multidisciplinary Team: Managing fetal distress often involves a multidisciplinary approach, with obstetricians, neonatologists, nurses, and other specialists working together to provide the best care for both the mother and the baby.
- Communication and Support: Healthcare providers maintain open communication with the mother, explaining the situation, the treatment plan, and any potential risks or complications. Emotional support for the mother and her family is crucial during this stressful time.
Complications Associated with Fetal Distress:
Here are some of the complications associated with fetal distress.
For the Baby (Fetus/Newborn):
- Hypoxia: Insufficient oxygen supply to the fetus can result in hypoxia, a condition where the body’s cells and tissues do not receive enough oxygen. Hypoxia can lead to cellular damage and affect organ function.
- Acidosis: Prolonged hypoxia can lead to acidosis, a condition characterized by an excessive buildup of acid in the baby’s blood. Acidosis can harm various organs and systems, including the brain, heart, and kidneys.
- Neurological Damage: Fetal distress, if severe and prolonged, can lead to brain damage in the baby. This can result in developmental delays, intellectual disabilities, cerebral palsy, or other neurological conditions.
- Meconium Aspiration Syndrome: In cases where meconium (the baby’s first stool) is present in the amniotic fluid and the baby inhales it during labor, meconium aspiration syndrome can occur. This can lead to breathing difficulties, lung infections, and respiratory distress in the newborn.
- Birth Injuries: The stress and complications associated with fetal distress can increase the risk of birth injuries, such as brachial plexus injuries or fractures, during delivery.
- Preterm Birth: In some cases, fetal distress may necessitate an early delivery, which can lead to prematurity. Premature infants may face a range of health challenges due to their underdeveloped organ systems.
For the Mother:
- Emotional Distress: Mothers who experience fetal distress may undergo significant emotional distress and anxiety during pregnancy, labor, and childbirth.
- Post-Traumatic Stress Disorder (PTSD): In severe cases or in situations involving emergency interventions like emergency C-sections, mothers may be at risk of developing PTSD as a result of the traumatic experience.
- Complications from Emergency C-Section: If a C-section becomes necessary due to fetal distress, the mother may face surgical complications, such as infection, bleeding, or anesthesia-related issues.
Emotional and Psychological Aspects:
Here are some of the emotional and psychological aspects to consider.
- Anxiety and Fear: The diagnosis of fetal distress often brings anxiety and fear for expectant parents. They may worry about the health and well-being of their baby, the potential complications, and the impact on their family.
- Stress: The stress associated with fetal distress can be overwhelming. Parents may feel overwhelmed by medical decisions, uncertainty about the future, and the need for immediate interventions.
- Grief and Loss: Parents may experience a sense of grief and loss if they had envisioned a different birth experience. This can be particularly true if a planned natural birth must be changed to an emergency C-section.
- Guilt and Self-Blame: Some parents may grapple with feelings of guilt or self-blame, wondering if they did something to cause the distress or if they could have prevented it.
- Post-Traumatic Stress: In severe cases or when there are traumatic interventions or complications, some parents may develop post-traumatic stress disorder (PTSD). This can lead to flashbacks, nightmares, and persistent anxiety related to the birth experience.
- Concern for the Baby’s Future: Parents may worry about the long-term health and development of their baby if fetal distress has led to complications or birth injuries.
- Impact on Bonding: The emotional distress associated with fetal distress can impact the initial bonding between parents and their newborn. It may take time for parents to bond with their baby, particularly if the baby requires medical attention or stays in the neonatal intensive care unit (NICU).
- Need for Support: Expectant parents facing fetal distress often benefit from emotional support. This can come from healthcare providers, family, friends, support groups, or mental health professionals. Seeking support is crucial for processing emotions and coping effectively.
- Communication with Healthcare Providers: Open and honest communication with healthcare providers can help alleviate anxiety and provide clarity about the situation, treatment options, and the baby’s condition.
- Postpartum Depression: Fetal distress and the associated stress can increase the risk of postpartum depression in new mothers. It’s essential to recognize the signs of postpartum depression and seek help if needed.
Research and Advances in Fetal Monitoring:
Here are some key areas of research and advances in fetal monitoring.
- Non-Invasive Monitoring Techniques: Researchers are continually exploring non-invasive methods for monitoring fetal health. This includes innovations in wearable devices that can provide continuous monitoring of the fetal heart rate and other parameters without the need for intrusive procedures.
- Artificial Intelligence (AI) and Machine Learning: AI and machine learning algorithms are being developed to analyze fetal monitoring data in real-time. These technologies can help healthcare providers identify patterns and deviations more accurately, potentially leading to earlier detection of fetal distress.
- Advanced Ultrasound Technology: Ultrasound imaging continues to advance, offering clearer and more detailed images of the fetus. 3D and 4D ultrasound technology provide valuable information about fetal development and well-being.
- Doppler Ultrasound: Doppler ultrasound is used to measure blood flow in the umbilical cord and other fetal vessels. Ongoing research aims to refine this technique to better assess blood flow patterns and detect abnormalities.
- Biophysical Profile (BPP): The BPP is a combination of tests used to assess fetal health. Research is ongoing to improve the accuracy and reliability of the BPP in identifying fetal distress and predicting adverse outcomes.
- Telemedicine and Remote Monitoring: Telemedicine and remote monitoring technologies allow healthcare providers to monitor fetal health and maternal conditions from a distance. This can be especially valuable in rural or underserved areas.
- Home Monitoring Devices: Advances in technology have led to the development of home monitoring devices that allow pregnant individuals to monitor fetal movements and heart rate at home. This can provide peace of mind and early alerts for potential issues.
- Genetic and Biomarker Screening: Research is ongoing to identify genetic markers and biomarkers that may indicate fetal distress or an increased risk of complications. These markers can be detected through maternal blood tests and may aid in early diagnosis.
- Placental Assessment: Innovative techniques for assessing placental health and function are being researched to better understand how the placenta affects fetal well-being.
- Integration of Data: The integration of data from various monitoring devices and tests is a focus of research. This holistic approach allows healthcare providers to have a comprehensive view of fetal and maternal health.
- Standardization of Protocols: Research efforts are dedicated to developing standardized protocols and guidelines for fetal monitoring to ensure consistency and best practices across healthcare settings.
FAQs:
What is fetal distress?
Fetal distress is a medical condition during pregnancy or labor in which there are concerns about the well-being of the developing fetus. It suggests that the fetus may not be receiving enough oxygen or nutrients, potentially leading to complications.
What are the common signs of fetal distress?
Common signs of fetal distress include abnormal fetal heart rate patterns, meconium-stained amniotic fluid, decreased fetal movements, abnormal contractions, and changes in amniotic fluid levels.
How is fetal distress diagnosed?
Fetal distress is diagnosed through a combination of continuous fetal heart rate monitoring, non-stress tests, ultrasound, and clinical assessments. Healthcare providers use these tools to assess fetal well-being.
What are the causes of fetal distress?
Fetal distress can result from various causes, including uteroplacental insufficiency, maternal health conditions, fetal factors, reduced amniotic fluid levels, abnormal fetal position, problems with the umbilical cord, infections, and more.
How is fetal distress managed and treated?
Management and treatment of fetal distress may involve changing the mother’s position, administering oxygen, providing IV fluids, using medications to improve uterine blood flow, and, in severe cases, performing an emergency C-section.
Are there long-term complications associated with fetal distress?
In some cases, fetal distress can lead to complications such as hypoxia, acidosis, neurological damage, meconium aspiration syndrome, birth injuries, and developmental issues for the baby.
Can fetal distress be prevented?
While not all cases of fetal distress can be prevented, maintaining regular prenatal care, adopting a healthy lifestyle, managing chronic health conditions, and avoiding environmental hazards can help reduce the risk.
How can expectant parents cope with the emotional aspects of fetal distress?
Coping with the emotional aspects of fetal distress may involve seeking emotional support, counseling, and self-care. Open communication with healthcare providers and staying informed can also help.
What are the latest advances in fetal monitoring?
Advances in fetal monitoring include non-invasive monitoring techniques, artificial intelligence and machine learning, advanced ultrasound technology, telemedicine, home monitoring devices, genetic and biomarker screening, and more.
Is fetal distress always an emergency?
Fetal distress can range from mild to severe. In some cases, it may necessitate immediate intervention, such as an emergency C-section, while in others, less invasive measures may be effective. The severity of distress determines the urgency of the response.
Conclusion:
In conclusion, fetal distress is a critical medical condition during pregnancy or labor that necessitates vigilant monitoring, prompt diagnosis, and appropriate intervention to safeguard the health and well-being of both the developing fetus and the mother. It can arise from various factors, including placental insufficiency, maternal health conditions, and fetal issues, and may manifest through signs such as abnormal heart rate patterns or meconium-stained amniotic fluid. While advancements in monitoring and medical technology continue to improve the early detection and management of fetal distress, its potential complications underscore the importance of comprehensive prenatal care, timely intervention, and emotional support for expectant parents facing this challenging situation.
Possible References Used