Escherichia coli, often abbreviated as E. coli, is a species of gram-negative bacteria commonly found in the lower intestine of warm-blooded organisms, including humans. While most strains of E. coli are harmless and play a beneficial role in digestion.
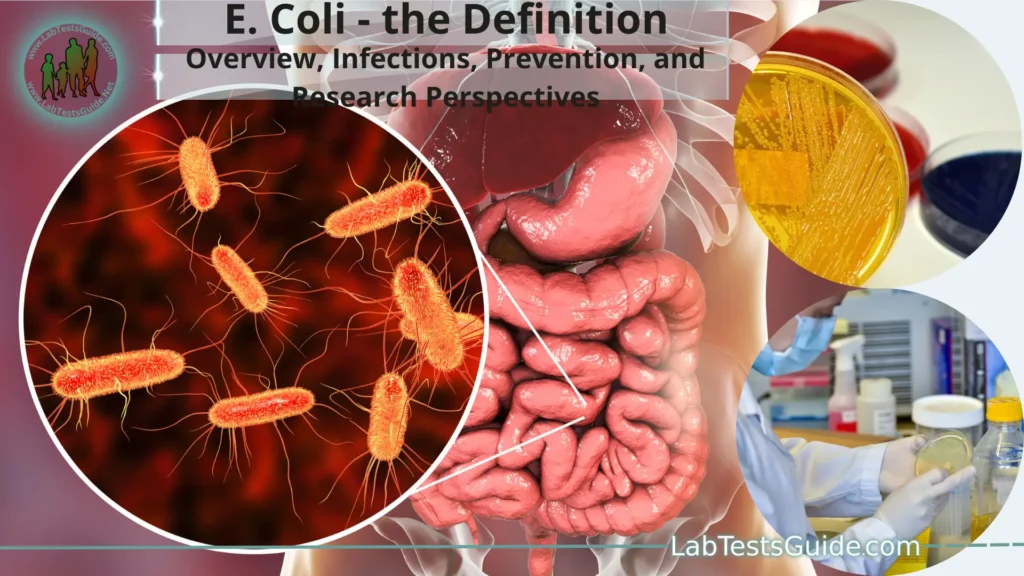
What is E. coli?
Escherichia coli, commonly known as E. coli, is a type of bacterium that belongs to the family Enterobacteriaceae. It is a gram-negative, rod-shaped bacterium that is commonly found in the lower intestines of warm-blooded animals, including humans. In the human gastrointestinal tract, E. coli is part of the normal gut flora and plays a beneficial role in digestion and nutrient absorption.
While most strains of E. coli are harmless and even beneficial, some strains can cause illness when they contaminate food, water, or the environment. These pathogenic strains of E. coli can produce toxins or possess virulence factors that allow them to cause a range of infections and diseases, especially when ingested in large numbers.
E. coli in Nature:
Here are some key points about E. coli in nature.
- Gut Microbiome: E. coli is a predominant member of the gut microbiota in mammals, including humans. It exists in symbiosis with its host, where it benefits from the nutrients in the gut environment, and in turn, it assists in the digestion of complex carbohydrates and the production of certain vitamins (e.g., vitamin K) for its host.
- Fecal Indicator: E. coli serves as a vital indicator organism for water quality and environmental hygiene. Its presence in water bodies, especially in high numbers, can indicate fecal contamination, which might contain other harmful pathogens that pose health risks.
- Decomposition and Nutrient Cycling: In the environment, E. coli plays a role in the decomposition of organic matter, breaking down complex compounds into simpler forms, and recycling nutrients back into the ecosystem.
- Ecological Balance: While E. coli is beneficial in its natural habitat, imbalances in the gut microbiome can lead to health issues. Certain factors, such as the overgrowth of pathogenic strains or the disruption of gut microbial diversity (e.g., due to antibiotics), can cause infections or digestive problems.
- Survival and Dispersal: Outside the host’s body, E. coli can survive for short periods in soil, water, and other environmental sources. Animal and human feces are the primary sources of E. coli in the environment, and contamination can occur through improper waste disposal or through runoff into water bodies.
- Research and Biotechnology: E. coli’s adaptability and ease of manipulation in the laboratory have made it a fundamental organism in scientific research, particularly in genetics and biotechnology. Scientists have extensively studied E. coli to understand basic cellular processes and develop various biotechnological applications, including the production of recombinant proteins and genetic engineering.
Types and Strains of E. coli:
Non-pathogenic E. coli:
- These strains are commonly found in the intestines of humans and other warm-blooded animals, where they play a beneficial role in digestion and nutrient absorption.
- Non-pathogenic E. coli strains are considered harmless and do not cause disease in healthy individuals.
- They are an essential part of the gut microbiota, contributing to the maintenance of a balanced gut ecosystem.
- Non-pathogenic E. coli strains do not possess the specific genetic elements or virulence factors that enable them to cause infections.
Pathogenic E. coli:
- Pathogenic E. coli strains are those that have acquired specific virulence factors or genes, allowing them to cause various diseases and infections in humans and animals.
- These strains can produce toxins or invade tissues, leading to illness when ingested in sufficient quantities.
- Pathogenic E. coli strains are responsible for a range of diseases, including foodborne illnesses, urinary tract infections (UTIs), and more severe conditions such as hemolytic uremic syndrome (HUS).
Some common pathogenic E. coli strains include:
- Enteropathogenic E. coli (EPEC): Causes attaching and effacing (A/E) lesions on the intestinal lining, leading to diarrhea, particularly in infants.
- Enterohemorrhagic E. coli (EHEC): Produces potent toxins, such as Shiga toxins, leading to severe foodborne illnesses and potentially causing HUS, a life-threatening condition affecting the kidneys and blood.
- Enterotoxigenic E. coli (ETEC): Causes traveler’s diarrhea and produces enterotoxins that lead to fluid secretion and watery diarrhea.
- Enteroaggregative E. coli (EAEC): Forms aggregative adherence to intestinal cells and is associated with persistent diarrhea, especially in young children and travelers.
- Enteroinvasive E. coli (EIEC): Invades intestinal cells, causing symptoms similar to shigellosis (bacillary dysentery).
- Enteropathogenic E. coli (EIEC): Causes inflammatory diarrhea and shares some features with Shigella species.
Pathogenesis and Virulence Factors:
Some common virulence factors found in pathogenic E. coli strains include.
Adhesins: Adhesins are proteins or molecules on the surface of E. coli that allow the bacterium to attach to specific receptors on host cells. By adhering to the intestinal lining or other tissues, E. coli can resist flushing out and gain a foothold in the host.
Toxins:
E. coli can produce various toxins, which are harmful molecules that damage host cells or interfere with cellular processes.
Some notable toxins produced by pathogenic E. coli strains include.
- Shiga Toxins: Produced by Enterohemorrhagic E. coli (EHEC) strains, Shiga toxins cause damage to blood vessels, leading to bloody diarrhea and, in severe cases, hemolytic uremic syndrome (HUS).
- Heat-Labile Toxin (LT) and Heat-Stable Toxin (ST): Produced by Enterotoxigenic E. coli (ETEC), these toxins cause an imbalance in ion transport in the intestinal lining, leading to watery diarrhea.
- Type III Secretion System (T3SS): This is a specialized molecular syringe-like apparatus used by certain pathogenic E. coli strains to inject bacterial proteins directly into host cells. These injected proteins can manipulate host cell functions, promoting bacterial survival and invasion.
- Capsule: Some pathogenic E. coli strains produce a protective capsule around themselves, shielding them from the host’s immune system and making it difficult for immune cells to target and eliminate the bacteria.
- Iron Acquisition Systems: E. coli requires iron for its growth, but in the host’s body, iron is often sequestered by the host’s defense mechanisms. Pathogenic E. coli strains possess systems that allow them to acquire iron from the host, enhancing their ability to colonize and multiply.
- Biofilm Formation: E. coli can form biofilms, which are communities of bacteria embedded in a protective matrix. Biofilms enable E. coli to adhere to surfaces and protect themselves from antibiotics and the host’s immune system.
E. coli-Related Diseases and Infections:
Some common E. coli-related diseases and infections include.
Gastrointestinal Infections:
- Traveler’s Diarrhea: Caused by Enterotoxigenic E. coli (ETEC), this infection is commonly associated with consuming contaminated food or water during travel. Symptoms include watery diarrhea, abdominal cramps, and fever.
- Food Poisoning: Enterohemorrhagic E. coli (EHEC) strains, such as E. coli O157:H7, are responsible for foodborne outbreaks. Ingestion of contaminated undercooked beef, raw vegetables, unpasteurized milk, or contaminated water can lead to severe abdominal pain, bloody diarrhea, and in some cases, hemolytic uremic syndrome (HUS).
- Urinary Tract Infections (UTIs): E. coli is a common cause of UTIs, especially in women. The bacteria can ascend the urethra and infect the bladder, causing symptoms like frequent and painful urination, lower abdominal pain, and cloudy or bloody urine.
- Neonatal Meningitis: In newborns, E. coli can cause meningitis, an inflammation of the membranes surrounding the brain and spinal cord. Neonatal meningitis can lead to serious neurological complications and requires immediate medical attention.
- Hemolytic Uremic Syndrome (HUS): This life-threatening condition can develop in some cases of EHEC infection, particularly in young children and the elderly. HUS is characterized by the destruction of red blood cells, low platelet counts, and acute kidney failure.
- Invasive Infections: In certain situations, E. coli can enter the bloodstream and cause sepsis, a severe and potentially fatal infection. This can occur when the bacteria spread from an initial infection site, such as the urinary tract or intestines, to other parts of the body.
- Uncomplicated Cystitis: E. coli is the most common cause of uncomplicated cystitis, a lower urinary tract infection that affects the bladder. It is prevalent in otherwise healthy women.
Transmission and Contamination:
The main modes of transmission and contamination include.
Foodborne Transmission:
- One of the most common ways E. coli infections occur is through the consumption of contaminated food. Contaminated raw or undercooked meat (especially ground beef), unpasteurized milk, and raw vegetables and fruits are primary sources of foodborne E. coli infections.
- Contamination can occur during food production, processing, or handling, often through contact with fecal matter from infected animals or contaminated water sources.
Waterborne Transmission:
- E. coli can be transmitted through the ingestion of contaminated water. This is particularly common in areas with poor sanitation or inadequate water treatment.
- Sewage runoff, fecal contamination of water sources, or improper waste disposal can lead to the presence of E. coli in water bodies.
Person-to-Person Transmission:
- E. coli infections, especially those causing gastroenteritis, can be easily transmitted from person to person through the fecal-oral route.
- Poor hygiene practices, such as inadequate handwashing after using the toilet, can lead to the spread of E. coli to surfaces and objects, facilitating its transmission to others.
Contact with Animals:
- E. coli can be transmitted from animals to humans through direct contact with infected animals or their environments.
- Petting zoos, farms, and animal handling activities can pose a risk of E. coli transmission, particularly for young children.
Environmental Contamination:
- E. coli can survive in the environment for a limited time outside of a host’s body. Contamination of soil, surfaces, or recreational water bodies with fecal matter can lead to potential exposure and infection.
Cross-Contamination:
- Cross-contamination occurs when pathogens from one surface or food item are transferred to another. For example, if raw meat is not handled separately from ready-to-eat foods, it can contaminate the latter with E. coli.
Preventing E. coli transmission and contamination involves several measures, including:
- Cooking meats thoroughly: Properly cooking meat, especially ground beef, to a safe internal temperature can kill E. coli and other harmful bacteria.
- Practicing good hygiene: Frequent and thorough handwashing with soap and water before eating, after using the toilet, and after handling animals is essential in preventing E. coli infections.
- Avoiding unpasteurized products: Consuming only pasteurized dairy products and juices can reduce the risk of contamination.
- Ensuring water safety: Drinking water from safe and treated sources is crucial in preventing waterborne E. coli infections.
- Following proper food safety practices: Handling and storing food correctly, washing fruits and vegetables before consumption, and preventing cross-contamination in the kitchen are essential in reducing the risk of foodborne E. coli infections.
Prevention and Control Measures:
Here are some key prevention and control measures.
Food Safety Practices:
- Cook meats thoroughly: Properly cook meat, especially ground beef, to a safe internal temperature (usually 160°F or 71°C) to kill E. coli and other harmful bacteria.
- Avoid cross-contamination: Separate raw meat from other foods during storage and preparation to prevent cross-contamination.
- Wash hands and surfaces: Regularly wash hands with soap and water before and after handling food, and clean kitchen surfaces, utensils, and cutting boards thoroughly to prevent the spread of bacteria.
Safe Water and Sanitation:
- Consume safe water: Ensure that drinking water comes from a safe and treated source to prevent waterborne E. coli infections.
- Practice good hygiene: Promote proper sanitation and hygiene practices, especially in areas with inadequate access to clean water and sanitation facilities.
Personal Hygiene:
- Frequent handwashing: Encourage regular and thorough handwashing with soap and water, especially after using the toilet, changing diapers, and before eating or preparing food.
- Educate about proper handwashing techniques: Proper handwashing should include scrubbing all parts of the hands, including under the nails and between fingers, for at least 20 seconds.
Safe Food Handling at Home and Restaurants:
- Train food handlers: Educate food handlers in restaurants and food service establishments about proper food safety practices to prevent foodborne illnesses.
- Temperature control: Ensure that perishable foods are stored at appropriate temperatures to prevent bacterial growth.
Avoiding Unpasteurized Products:
- Consume pasteurized dairy products and juices, as they have been heat-treated to kill harmful bacteria like E. coli.
Petting Zoo and Animal Contact Safety:
- Practice hand hygiene: Encourage handwashing after handling animals or coming into contact with their environments in places like petting zoos and farms.
Public Health Surveillance and Outbreak Investigation:
- Monitor and investigate outbreaks: Public health authorities should track cases of E. coli infections to identify outbreaks and sources of contamination promptly.
- Implement control measures: During outbreaks, appropriate measures should be taken to prevent further transmission, such as product recalls or temporary closures of affected facilities.
Education and Awareness:
- Public awareness campaigns: Educate the public about the risks of E. coli infections and the importance of adopting preventive measures.
- Healthcare provider education: Train healthcare professionals to recognize and manage E. coli infections effectively.
Laboratory Diagnosis of E. coli Infections:
Here are some common methods used in the laboratory diagnosis of E. coli infections.
Microscopic Examination:
- A preliminary step in the diagnosis involves the examination of clinical specimens under a microscope. Gram staining can help identify the bacteria as gram-negative rods, which is a characteristic feature of E. coli.
Culture and Isolation:
- Clinical specimens, such as stool samples for gastrointestinal infections or urine samples for urinary tract infections, are cultured on selective media that encourage the growth of E. coli. MacConkey agar is commonly used, as E. coli produces pink colonies on this medium due to lactose fermentation.
- Once isolated, further tests are conducted to confirm the identity of the bacterium as E. coli.
Biochemical Tests:
- Biochemical tests are performed to differentiate E. coli from other similar bacteria. E. coli is characterized by its ability to ferment lactose and produce gas from glucose fermentation.
- Common tests include the IMViC (Indole, Methyl Red, Voges-Proskauer, Citrate) tests, which help distinguish E. coli from other members of the Enterobacteriaceae family.
Antigen Detection:
- In some cases, specific antigens of E. coli can be detected in clinical specimens using immunoassays or rapid diagnostic tests. These tests are often used in point-of-care settings to provide quick results.
Molecular Methods:
- Polymerase Chain Reaction (PCR) is a sensitive and specific method used to detect and identify E. coli DNA in clinical specimens. It can identify specific virulence factors associated with pathogenic strains of E. coli.
- Real-time PCR allows for rapid detection and quantification of E. coli DNA and is especially useful in outbreak investigations.
Serological Testing:
- Serological tests can detect antibodies against specific E. coli antigens in patient serum. These tests are used in certain cases, such as diagnosing hemolytic uremic syndrome (HUS).
Susceptibility Testing:
- In cases where antibiotic treatment is necessary, susceptibility testing is performed to determine the most appropriate antibiotics to use.
Treatment and Management:
Here are some general guidelines for the treatment and management of E. coli infections.
Supportive Care:
- For mild cases of E. coli infection, such as gastroenteritis with mild symptoms, supportive care may be sufficient. This includes staying hydrated by drinking plenty of fluids to replace lost fluids from diarrhea and vomiting.
Antibiotic Therapy:
- Antibiotics are not always recommended for all types of E. coli infections. In fact, they may be contraindicated for certain strains, such as Enterohemorrhagic E. coli (EHEC) infections, as antibiotic use can increase the risk of developing hemolytic uremic syndrome (HUS).
- For certain severe infections or cases where antibiotics are deemed appropriate, the choice of antibiotic will depend on the susceptibility of the bacterial strain to the drug. Antibiotic susceptibility testing helps determine the most effective treatment.
Hemolytic Uremic Syndrome (HUS) Management:
- For patients with HUS, which can result from certain E. coli infections, hospitalization and supportive care are often necessary. Treatment may include fluid and electrolyte management and blood transfusions.
- In severe cases, patients may require kidney dialysis to support kidney function until they recover.
Urinary Tract Infections (UTIs) and Neonatal Meningitis:
- E. coli UTIs and neonatal meningitis are generally treated with appropriate antibiotics based on susceptibility testing.
Avoid Anti-diarrheal Medications:
- Anti-diarrheal medications (e.g., loperamide) should be avoided in cases of severe diarrhea caused by E. coli infections, especially when there is blood in the stool. These medications can delay the elimination of bacteria and toxins from the body.
Isolation and Infection Control Measures:
- In cases of highly contagious E. coli infections or outbreaks, isolation precautions may be necessary to prevent the spread of the bacteria to others. This is particularly important in healthcare settings.
Monitoring and Follow-up:
- Patients with E. coli infections, especially those who develop complications, need close monitoring by healthcare professionals.
- Follow-up visits are essential to ensure that the infection is resolving and to manage any potential long-term complications.
Research and Future Perspectives:
Some key areas of research and future perspectives related to E. coli include:
Antimicrobial Resistance (AMR):
- As with many bacterial pathogens, the emergence of antimicrobial-resistant E. coli strains is a significant concern. Researchers are studying the mechanisms of resistance and searching for new strategies to combat AMR, such as developing novel antibiotics or alternative therapies.
Vaccine Development:
- The development of vaccines against pathogenic E. coli strains, particularly those causing severe foodborne illnesses and HUS, is an ongoing research focus. Vaccination could potentially prevent infections and reduce the burden of E. coli-related diseases.
One Health Approach:
- The “One Health” approach emphasizes the interconnectedness of human, animal, and environmental health. Research in this area explores the role of E. coli in various ecosystems and the transmission dynamics between animals and humans.
Gut Microbiome Studies:
- Advancements in genomic technologies have enabled researchers to explore the gut microbiome composition and function in greater detail. Studying the interplay between E. coli and other gut microbes can provide insights into the health implications of altered gut microbiota and potential therapeutic interventions.
Phage Therapy:
- Phage therapy, the use of bacteriophages to target and kill specific bacteria, is gaining attention as a potential alternative to antibiotics in treating E. coli infections. Researchers are investigating phage therapy’s effectiveness, safety, and practical applications.
Genetic Engineering and Biotechnology:
- E. coli remains a valuable model organism in genetic engineering and biotechnology. Researchers continue to modify and improve E. coli strains for various applications, such as producing biofuels, pharmaceuticals, and other useful compounds.
Epidemiology and Outbreak Investigations:
- Understanding the epidemiology of E. coli infections, including sources of contamination and transmission routes, is crucial for outbreak prevention and control. Ongoing surveillance and investigation of outbreaks help inform public health measures.
Innovative Diagnostics:
- Research is focused on developing rapid and sensitive diagnostic methods for identifying E. coli strains and detecting specific virulence factors. These advancements can aid in early diagnosis, outbreak response, and targeted treatment.
Climate Change Impacts:
- Climate change can influence the prevalence and distribution of infectious diseases, including E. coli infections. Researchers are investigating how climate-related factors may impact E. coli dynamics and the risk of transmission.
Health Policy and Guidelines:
- Evidence-based research informs health policies, guidelines, and interventions to prevent and manage E. coli infections. Continual evaluation and updates to these measures are essential to address evolving challenges.
FAQs:
What is E. coli?
E. coli, short for Escherichia coli, is a type of bacterium commonly found in the lower intestine of warm-blooded animals, including humans. While most strains are harmless and beneficial, some can cause infections and diseases when they contaminate food or water.
What are the symptoms of an E. coli infection?
Symptoms of an E. coli infection can vary depending on the strain and severity. Common symptoms include diarrhea (sometimes bloody), abdominal cramps, nausea, vomiting, and fever.
How do you get infected with E. coli?
E. coli infections are typically acquired by consuming contaminated food, water, or other infected substances. Person-to-person transmission is also possible through fecal-oral routes.
What foods are most commonly associated with E. coli outbreaks?
Foods commonly associated with E. coli outbreaks include undercooked ground beef, raw vegetables, raw milk, unpasteurized juices, and contaminated water.
Can E. coli infections be treated with antibiotics?
While some E. coli infections may require antibiotic treatment, it’s important to note that antibiotics are not recommended for certain strains, such as Enterohemorrhagic E. coli (EHEC), as they can worsen the infection.
How can I prevent E. coli infections?
Preventive measures include practicing good food safety, thoroughly cooking meat, washing fruits and vegetables, avoiding unpasteurized products, maintaining proper hygiene, and ensuring safe water sources.
What is the difference between pathogenic and non-pathogenic E. coli?
Non-pathogenic E. coli strains are harmless and typically found in the gut as part of the normal flora. Pathogenic strains have acquired specific genes or virulence factors, enabling them to cause infections and diseases.
Is E. coli dangerous for everyone?
Most E. coli strains are harmless for healthy individuals. However, some pathogenic strains can cause severe illnesses, particularly in young children, the elderly, and individuals with weakened immune systems.
Are there any vaccines for E. coli infections?
Vaccine development for specific pathogenic E. coli strains, such as Enterotoxigenic E. coli (ETEC) and Enterohemorrhagic E. coli (EHEC), is ongoing. Currently, no licensed vaccines are widely available.
What should I do if I suspect an E. coli infection?
If you suspect you have an E. coli infection and experience severe or persistent symptoms, seek medical attention promptly. Your healthcare provider can evaluate your condition and provide appropriate care.
Conclusion:
In conclusion, Escherichia coli (E. coli) is a versatile bacterium commonly found in the intestines of warm-blooded animals, including humans. While most strains are harmless and even beneficial, certain pathogenic strains can cause infections and diseases, leading to gastroenteritis, urinary tract infections, and potentially life-threatening conditions like hemolytic uremic syndrome (HUS). Prevention and control measures, such as proper food safety practices, hygiene, and surveillance, are crucial in minimizing the risk of E. coli-related infections. Ongoing research in areas like antimicrobial resistance, vaccine development, and the gut microbiome promises to deepen our understanding and improve management strategies for E. coli infections, safeguarding public health in the future.
Possible References Used