Cryoprecipitate, often referred to as “cryo,” is a blood component that is derived from blood plasma. It is prepared by slowly thawing frozen plasma at a controlled rate and then removing the frozen portion, which contains a high concentration of certain proteins and clotting factors. Cryoprecipitate is typically used in medical settings to treat bleeding disorders, particularly those related to clotting factor deficiencies.
Definition of Cryoprecipitate.
Cryoprecipitate is a blood product that is derived from plasma through a process of controlled thawing and separation. It is a component of blood that contains a high concentration of certain proteins and clotting factors essential for blood clot formation and hemostasis (the body’s process of stopping bleeding). Cryoprecipitate is obtained by slowly thawing frozen plasma and then removing the frozen portion, which contains the desired components.
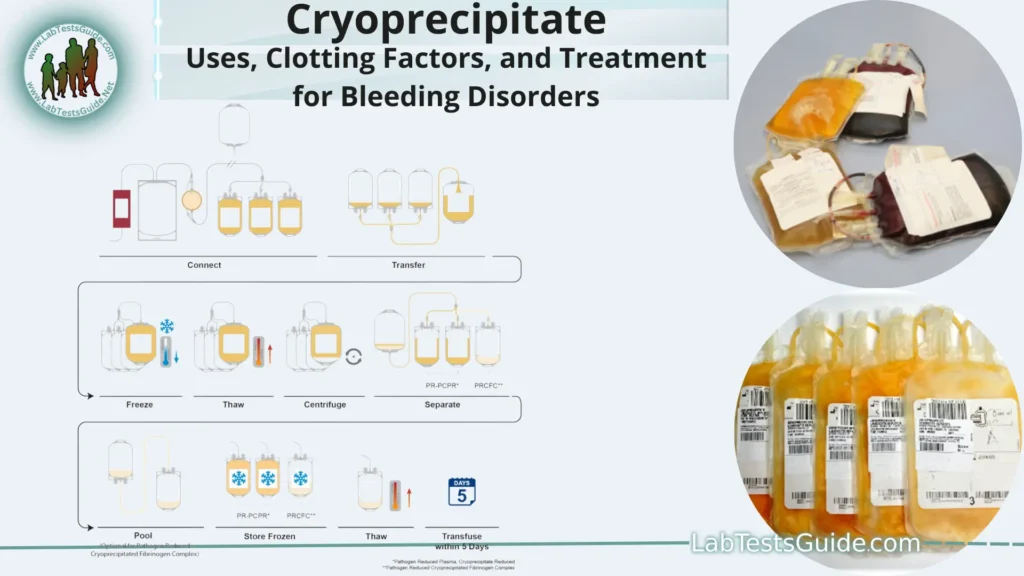
Preparation and Collection.
- Blood Donation: The process begins with voluntary blood donation. Donors provide whole blood, which is then separated into its individual components, including red blood cells, plasma, platelets, and white blood cells.
- Plasma Collection: Once the blood is collected, it undergoes a process called apheresis. During apheresis, the whole blood is separated using a centrifuge machine, which spins the blood at high speeds. This separates the plasma from the other components.
- Freezing the Plasma: The collected plasma is rapidly frozen to preserve its components. This freezing process prevents degradation and maintains the stability of the proteins and clotting factors within the plasma.
- Thawing and Fractionation: When cryoprecipitate is needed, the frozen plasma is slowly thawed at controlled temperatures. As the plasma thaws, it forms layers, and the cryoprecipitate-enriched layer is separated from the rest of the plasma.
- Cryoprecipitate Extraction: The cryoprecipitate-enriched layer, which contains higher concentrations of proteins like fibrinogen, factor VIII, von Willebrand factor, fibronectin, and factor XIII, is collected and extracted. This layer is rich in these clotting factors and proteins, making it suitable for therapeutic use.
- Pooling and Processing: Cryoprecipitate from multiple donors might be pooled together and processed to ensure consistent concentrations of clotting factors and proteins in the final product. This helps standardize the quality and effectiveness of cryoprecipitate.
- Packaging and Storage: The extracted cryoprecipitate is packaged in appropriate storage containers, often in small bags. These bags are typically labeled with relevant information, including donor information, batch number, and expiration date. Cryoprecipitate is stored in freezers at very low temperatures to maintain its stability.
- Distribution and Use: Once prepared, cryoprecipitate can be distributed to medical facilities where it is needed. Healthcare professionals administer cryoprecipitate to patients with bleeding disorders, such as hemophilia and von Willebrand disease, through intravenous infusion.
Components and Clotting Factors:
Here are some of the key components and clotting factors found in cryoprecipitate.
- Fibrinogen: Fibrinogen is a soluble protein and a key component of the blood clotting cascade. When bleeding occurs, fibrinogen is converted into fibrin through the action of thrombin, an enzyme. Fibrin forms a mesh-like structure that helps stabilize blood clots and prevent further bleeding.
- Factor VIII: Also known as antihemophilic factor, Factor VIII is a vital clotting factor in the intrinsic pathway of the blood clotting cascade. It is essential for the formation of stable blood clots by aiding in the activation of other clotting factors.
- von Willebrand Factor: von Willebrand factor (vWF) is a glycoprotein that serves multiple roles in blood clotting. It promotes platelet adhesion to damaged blood vessels and helps stabilize the initial platelet plug that forms at the site of injury. It also carries and protects Factor VIII in circulation.
- Fibronectin: Fibronectin is a glycoprotein that aids in cell adhesion, wound healing, and the repair of injured tissues. It plays a role in stabilizing blood clots and supporting the overall healing process.
- Factor XIII: Factor XIII is a clotting factor responsible for cross-linking fibrin strands during the final stages of clot formation. This cross-linking strengthens the clot and makes it more stable.
Indications for Use:
Here are some of the main indications for using cryoprecipitate,
- Hemophilia A: Hemophilia A is a genetic bleeding disorder caused by a deficiency or dysfunction of Factor VIII, a crucial clotting factor. Cryoprecipitate contains a concentrated amount of Factor VIII, making it an effective treatment option to help control bleeding episodes in individuals with hemophilia A.
- von Willebrand Disease: Von Willebrand disease is an inherited bleeding disorder caused by a deficiency or dysfunction of von Willebrand factor (vWF). Cryoprecipitate contains vWF, which enhances platelet adhesion and helps stabilize blood clots. Therefore, cryoprecipitate can be used to manage bleeding in individuals with von Willebrand disease.
- Fibrinogen Deficiency (Hypofibrinogenemia): Fibrinogen deficiency is a condition where the body doesn’t produce enough fibrinogen, a protein essential for blood clot formation. Cryoprecipitate is rich in fibrinogen and can be used to address bleeding associated with fibrinogen deficiency.
- Massive Blood Loss and Coagulopathy: In cases of severe trauma, surgery, or other situations involving massive blood loss, the body’s clotting factors can become depleted, leading to a condition known as coagulopathy. Cryoprecipitate can be used to rapidly replenish clotting factors and stabilize blood clotting in such critical situations.
- Congenital Clotting Factor Deficiencies: There are other rare congenital clotting factor deficiencies that can lead to bleeding disorders. Cryoprecipitate, containing a combination of clotting factors and proteins, can be used to address bleeding in these cases.
Administration and Usage:
- Preparation and Compatibility: Before administering cryoprecipitate, healthcare providers ensure that the blood product is compatible with the patient’s blood type to prevent adverse reactions. Cryoprecipitate is usually stored in frozen state and needs to be thawed prior to use.
- Thawing: Cryoprecipitate bags are placed in a controlled thawing environment, usually a blood bank refrigerator or a specially designed thawing device. Thawing is done slowly to preserve the integrity of the proteins and clotting factors.
- Administration: Once thawed, cryoprecipitate is prepared for administration. It’s typically infused through a dedicated intravenous line. The rate of infusion can vary based on the patient’s condition and the medical facility’s protocols. A healthcare professional, such as a nurse or doctor, will closely monitor the infusion process.
- Dosage: The dosage of cryoprecipitate depends on factors such as the patient’s weight, the severity of bleeding, and the specific clotting factor deficiency. Healthcare providers use established guidelines and protocols to determine the appropriate dosage for each individual.
- Monitoring: During the infusion, the patient’s vital signs are closely monitored to ensure there are no adverse reactions. Monitoring may include tracking heart rate, blood pressure, and respiratory rate.
- Response and Adjustments: The response to cryoprecipitate treatment is evaluated. In some cases, additional doses may be needed to achieve the desired clotting factor levels and control bleeding. The decision to administer more doses is made based on the patient’s clinical response and laboratory test results.
- Post-Infusion Care: After the infusion is complete, the intravenous line is removed, and the patient is monitored for any potential side effects or complications.
- Follow-Up: Patients who receive cryoprecipitate are often monitored for a period of time to ensure that bleeding is effectively controlled. Laboratory tests may be performed to assess the levels of clotting factors and determine the success of the treatment.
Advantages and Considerations:
- Concentrated Clotting Factors: Cryoprecipitate contains a high concentration of clotting factors and proteins, making it effective in rapidly raising the levels of essential components needed for blood clotting.
- Rapid Action: Cryoprecipitate can quickly address bleeding episodes in patients with clotting factor deficiencies, making it especially useful in emergency situations.
- Broad Spectrum: Since cryoprecipitate contains a combination of clotting factors and proteins, it can be used to address bleeding disorders caused by various deficiencies.
- Readily Available: Cryoprecipitate can be prepared relatively quickly from plasma donations, making it more accessible in comparison to other clotting factor concentrates.
- Cost-Effective: In some settings, cryoprecipitate may be more cost-effective than alternative treatments, especially for managing acute bleeding episodes.
Considerations and Limitations:
- Risk of Infection: Cryoprecipitate, like other blood products, carries a risk of transmitting infections. Though stringent testing and processing protocols are in place to minimize this risk, it’s important to be cautious.
- Variable Clotting Factor Levels: The concentration of clotting factors in cryoprecipitate can vary between donors and batches, which might lead to variability in treatment efficacy.
- Limited Precision: Cryoprecipitate does not allow precise control over dosages of individual clotting factors, which newer therapies like recombinant clotting factors offer.
- Volume Considerations: Administering cryoprecipitate might require the infusion of a larger volume of fluid compared to other clotting factor concentrates, potentially impacting patients with volume-sensitive conditions.
- Storage and Thawing Requirements: Proper storage and thawing procedures are critical to maintaining the efficacy of cryoprecipitate. Improper handling can lead to reduced clotting factor activity.
- Risk of Allergic Reactions: Although rare, allergic reactions to cryoprecipitate can occur, particularly in individuals who are sensitive to blood products.
- Availability of Alternatives: Advances in medical science have led to the development of more targeted and safer treatments, such as recombinant clotting factors, that offer better control over dosages and reduced risks of complications.
- Patient-Specific Factors: The appropriateness of using cryoprecipitate depends on individual patient factors, including their medical history, underlying conditions, and response to treatment.
Alternatives and Advances:
Here are some notable alternatives and advances.
- Recombinant Clotting Factors: Recombinant clotting factors are genetically engineered versions of specific clotting factors that are manufactured in a laboratory. These products provide a highly purified and standardized source of the deficient clotting factor. They offer precise dosing, lower risk of infections, and reduced variability compared to cryoprecipitate.
- Factor Concentrates: Factor concentrates are purified and concentrated forms of specific clotting factors, often derived from human plasma or produced through recombinant technology. They allow for more targeted treatment by delivering the exact clotting factor needed, minimizing the risk of over-administration.
- Desmopressin (DDAVP): Desmopressin is a synthetic hormone that can stimulate the release of von Willebrand factor and Factor VIII from the body’s stores. It is often used to treat mild forms of von Willebrand disease and some cases of mild hemophilia A.
- Hemostatic Agents: Hemostatic agents, such as topical agents or fibrin sealants, are used to promote blood clotting at the site of bleeding. These agents can be particularly helpful in managing localized bleeding during surgical procedures.
- Targeted Therapies: Ongoing research is exploring targeted therapies that aim to correct the underlying genetic mutations responsible for bleeding disorders. Gene therapy, for instance, involves introducing functional copies of defective genes into a patient’s cells to restore normal clotting factor production.
- Pharmacologic Agents: Pharmacologic agents, such as antifibrinolytic medications (e.g., tranexamic acid), can be used to prevent the breakdown of blood clots and control bleeding in certain situations.
- Personalized Treatment Plans: Advances in understanding bleeding disorders and genetics allow for more personalized treatment plans tailored to individual patient needs. This includes selecting the most appropriate treatment based on factors like the severity of the disorder, the patient’s medical history, and the presence of inhibitors.
- Improved Monitoring Techniques: Advanced laboratory techniques and assays allow for more accurate and timely monitoring of clotting factor levels, ensuring that treatment is tailored to each patient’s specific needs.
Clinical Practices and Guidelines:
Here are some key aspects of clinical practices and guidelines
- Diagnosis and Assessment: Accurate diagnosis is essential for determining the appropriate treatment plan. Healthcare providers conduct thorough assessments, including medical history, physical examinations, and laboratory tests to identify the specific bleeding disorder and its severity.
- Treatment Selection: Treatment decisions are based on the type of bleeding disorder, the patient’s age, medical history, and overall health. Clinical guidelines help healthcare professionals choose the most appropriate treatment option, whether it’s cryoprecipitate, recombinant clotting factors, or other therapies.
- Dosing and Administration: Clinical guidelines provide dosing recommendations for various treatments. Specific dosages depend on the patient’s weight, the severity of bleeding, and the desired increase in clotting factor levels.
- Monitoring and Follow-Up: Monitoring is crucial to assess the effectiveness of treatment and ensure patient safety. Regular laboratory tests are used to measure clotting factor levels and adjust treatment as needed. Follow-up appointments help healthcare providers evaluate the patient’s response to treatment over time.
- Emergency Protocols: For patients with severe bleeding disorders, emergency protocols outline rapid and appropriate treatment strategies to manage life-threatening bleeding episodes.
- Patient Education: Patients and their families are educated about the nature of their bleeding disorder, treatment options, how to administer treatments (if applicable), and when to seek medical help.
- Inhibitor Management: Inhibitors, antibodies that neutralize clotting factors, can develop in some patients with bleeding disorders. Clinical guidelines address strategies for managing and treating patients with inhibitors.
- Special Populations: Guidelines consider special populations, such as pediatric patients, pregnant individuals, and the elderly, and provide tailored recommendations for their treatment.
- Treatment Centers and Multidisciplinary Care: Many bleeding disorders are managed through specialized treatment centers that provide multidisciplinary care. These centers include hematologists, nurses, genetic counselors, and other specialists to offer comprehensive care.
- Regular Updates: Clinical practices and guidelines are regularly updated based on new research findings and advancements in medical science. This ensures that healthcare providers have access to the latest evidence-based information.
Research and Future Directions:
Here are some areas of research and future directions in this field.
- Gene Therapy: Gene therapy involves introducing functional copies of genes responsible for producing clotting factors into a patient’s cells. This approach aims to provide a long-term solution by addressing the underlying genetic cause of bleeding disorders.
- Targeted Therapies: Researchers are investigating targeted therapies that can specifically enhance the production of deficient clotting factors, potentially reducing the need for frequent infusions.
- Small Molecule Therapies: Small molecules and pharmacologic agents are being developed to enhance blood clotting by targeting specific pathways involved in the coagulation process.
- Inhibitor Management: Managing inhibitors, antibodies that neutralize clotting factors, remains a challenge. Research focuses on developing strategies to prevent and overcome inhibitor development.
- Personalized Medicine: Advances in genetics and personalized medicine enable tailored treatment plans based on individual patient profiles. This includes selecting the most suitable treatment option and dosage for each patient.
- Improved Clotting Factor Concentrates: Researchers are working on refining clotting factor concentrates to improve their stability, shelf life, and effectiveness.
- Hemostatic Agents: Further research is being conducted to develop novel hemostatic agents that can promote clotting and wound healing.
- Bleeding Disorder Registries: The establishment of national and international bleeding disorder registries helps gather comprehensive data on patient outcomes, treatment responses, and disease trends.
- Enhanced Monitoring Techniques: Advances in laboratory techniques allow for more precise and rapid monitoring of clotting factor levels, enabling quicker adjustments to treatment regimens.
- Patient Quality of Life: Research is focusing on understanding the impact of bleeding disorders on patients’ quality of life and psychological well-being, leading to improved support and care strategies.
- Preventive Measures: Education and awareness campaigns aim to prevent unnecessary bleeding by promoting safety measures and prompt treatment.
- Global Access to Treatment: Efforts continue to ensure that individuals with bleeding disorders, especially in underserved regions, have access to appropriate treatment and care.
FAQs:
What is cryoprecipitate?
Cryoprecipitate is a blood product derived from plasma that contains high concentrations of clotting factors and proteins essential for blood clot formation. It is used to treat bleeding disorders.
Which clotting factors are present in cryoprecipitate?
Cryoprecipitate contains clotting factors such as fibrinogen, Factor VIII, von Willebrand factor, fibronectin, and Factor XIII.
What are the indications for using cryoprecipitate?
Cryoprecipitate is used to treat bleeding disorders such as hemophilia A, von Willebrand disease, fibrinogen deficiency, and coagulopathy due to massive blood loss.
How is cryoprecipitate administered?
Cryoprecipitate is administered intravenously through a dedicated line. It is thawed, prepared, and infused at a controlled rate.
What are the advantages of using cryoprecipitate?
Cryoprecipitate offers concentrated clotting factors, rapid action in controlling bleeding, and a broad spectrum of applications in various bleeding disorders.
What are the limitations of cryoprecipitate?
Limitations include variability in clotting factor levels, risk of infections, volume considerations, and the availability of more precise alternatives.
Are there alternatives to cryoprecipitate?
Yes, alternatives include recombinant clotting factors, factor concentrates, desmopressin, hemostatic agents, and targeted therapies. These offer advantages such as precise dosing and reduced infection risk.
How are clinical practices and guidelines established for bleeding disorders?
Clinical practices and guidelines are based on scientific research, expert consensus, and advancements in medical science. They provide recommendations for diagnosis, treatment selection, dosing, monitoring, and patient education.
What are some future directions in bleeding disorder research?
Research is focused on gene therapy, targeted therapies, small molecule treatments, inhibitor management, personalized medicine, and improving clotting factor concentrates.
How can patients with bleeding disorders stay informed and receive optimal care?
Patients should work closely with their healthcare providers, follow recommended treatment plans, stay informed about advancements, and participate in patient advocacy groups.
Conclusion:
In conclusion, cryoprecipitate is a valuable blood product derived from plasma, enriched with essential clotting factors and proteins that play a vital role in promoting blood clot formation and managing bleeding disorders such as hemophilia A, von Willebrand disease, and fibrinogen deficiency. While it has been an effective treatment option, advancements in medical science have introduced alternatives like recombinant clotting factors and targeted therapies that offer improved precision, reduced infection risk, and enhanced patient care. The field of bleeding disorder management continues to evolve through ongoing research, personalized treatment approaches, and a commitment to improving patient outcomes and quality of life.
Possible References Used