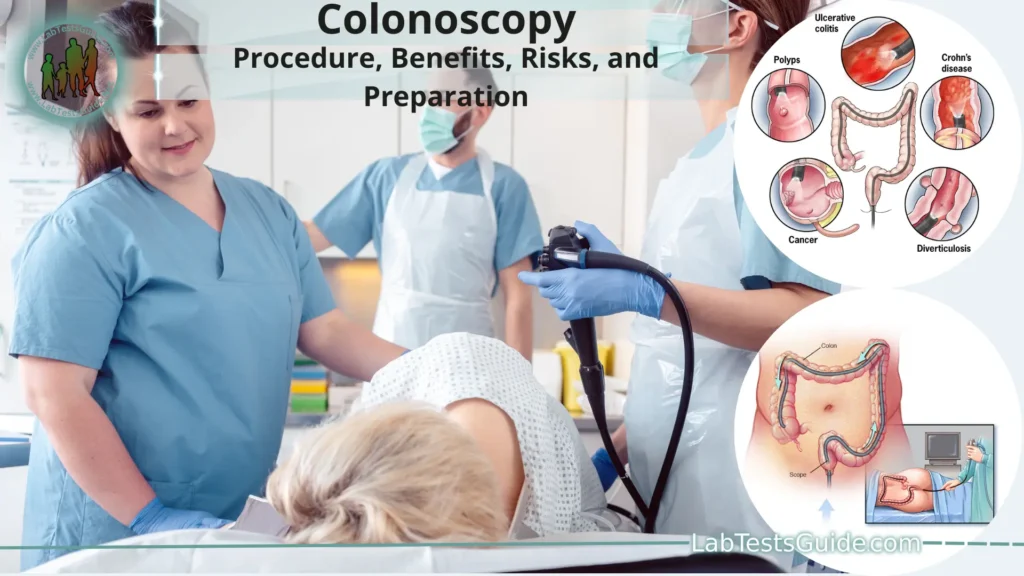
A colonoscopy is a medical procedure that involves the examination of the inside of the colon (large intestine) and rectum using a flexible, lighted tube called a colonoscope. This procedure is typically performed by a gastroenterologist, a doctor who specializes in the digestive system.
Definition of Colonoscopy.
A colonoscopy is a medical procedure in which a flexible, lighted tube called a colonoscope is used to examine the inside of the colon (large intestine) and rectum. This procedure allows healthcare professionals, usually gastroenterologists, to visually inspect the lining of the colon for signs of abnormalities, such as polyps, inflammation, ulcers, and tumors. Colonoscopies are performed for various purposes, including early detection of colorectal cancer, diagnosis of digestive disorders, and investigation of gastrointestinal symptoms. During the procedure, any identified polyps or abnormal tissue can be removed for further examination or to prevent potential development into more serious conditions.
Patient Education and Informed Consent:
Patient Education:
- Patient education involves providing patients with clear, accurate, and understandable information about their medical condition, treatment options, and procedures. This empowers patients to make informed decisions about their healthcare.
In the context of a colonoscopy:
- Patients should receive information about what a colonoscopy entails, why it’s recommended, and how it will be conducted.
- They should understand the preparation process, including dietary restrictions and bowel cleansing procedures.
- Patients should be informed about the potential discomfort or risks associated with the procedure and the use of sedation.
- The healthcare provider should explain the importance of following pre- and post-procedure instructions for a successful outcome.
- Patients should have the opportunity to ask questions to clarify any doubts or concerns they might have.
Informed Consent:
- Informed consent is the process through which a patient gives permission for a medical procedure or treatment after fully understanding its nature, potential risks, benefits, and alternatives.
In the context of a colonoscopy:
- The healthcare provider should explain the purpose of the colonoscopy, the procedure itself, and its potential benefits in detecting or preventing conditions.
- Patients should be informed about the possible risks, such as bleeding, perforation, and adverse reactions to sedation.
- Alternatives to the procedure, such as other screening methods, should be discussed.
- Patients should understand that they have the right to refuse the procedure and the implications of their decision.
- The discussion should be documented, and patients should sign a consent form indicating their understanding and agreement.
- Communication: Effective communication between healthcare providers and patients is crucial. It ensures that patients have realistic expectations, are emotionally prepared, and can actively participate in their healthcare decisions. Healthcare providers should use clear and simple language, avoid medical jargon, and encourage patients to ask questions.
- Respect for Autonomy: Patient education and informed consent uphold the principle of respect for autonomy, allowing patients to exercise their right to make decisions about their own bodies and healthcare. Healthcare providers should provide information without coercion and respect the patient’s choices.
- Ethical and Legal Aspects: Informed consent is not only an ethical obligation but often a legal requirement. It varies by jurisdiction and may have specific legal guidelines for how it should be obtained and documented.
Alternative Screening Methods:
Here are some common alternative screening methods.
Fecal Occult Blood Test (FOBT) and Fecal Immunochemical Test (FIT):
These tests detect hidden blood in the stool, which could be a sign of colorectal cancer or other conditions.
FOBT uses a chemical reaction to detect blood, while FIT uses antibodies specific to human blood.
These tests are non-invasive and can be done at home. Positive results usually lead to further evaluation, including colonoscopy.
Stool DNA Test (FIT-DNA Test or Cologuard):
This test combines FIT with the detection of altered DNA in stool samples, which may indicate the presence of colorectal cancer or precancerous polyps.
Stool DNA tests can be done at home and are repeated every few years if results are negative.
Flexible Sigmoidoscopy:
- Similar to a colonoscopy, this procedure uses a flexible tube with a camera to examine the lower part of the colon.
- Unlike colonoscopy, flexible sigmoidoscopy doesn’t require sedation and only examines a portion of the colon. If abnormalities are found, a colonoscopy may be recommended.
Virtual Colonoscopy (CT Colonography):
- This involves a CT scan of the colon, creating detailed images that can be used to identify polyps or tumors.
- While it’s less invasive than a traditional colonoscopy, it still requires bowel preparation and exposes patients to radiation.
Blood Tests for Colorectal Cancer Biomarkers:
- Some blood tests can detect specific biomarkers associated with colorectal cancer.
- These tests are still under development and not widely used for routine screening.
Capsule Endoscopy:
- In this procedure, a patient swallows a small camera capsule that takes pictures as it travels through the digestive tract.
- It’s primarily used for examining the small intestine and is not a common method for colorectal cancer screening.
Uses of Colonoscopy:
Here are some of the key uses of colonoscopy.
Screening for Colorectal Cancer:
- Colonoscopy is an important tool for early detection and prevention of colorectal cancer. During the procedure, gastroenterologists can identify and remove polyps—small growths on the colon lining—that may eventually develop into cancerous tumors. Regular screenings can help detect and treat precancerous lesions before they become malignant.
Diagnosis of Gastrointestinal Conditions:
Colonoscopy is used to diagnose a range of gastrointestinal disorders and conditions, including.
- Inflammatory Bowel Diseases (IBD) like Crohn’s disease and ulcerative colitis.
- Diverticulosis and diverticulitis, which involve the formation of pouches in the colon.
- Gastrointestinal bleeding or unexplained changes in bowel habits.
- Irritable Bowel Syndrome (IBS) and chronic gastrointestinal symptoms.
- Investigation of Abnormal Symptoms: When patients experience symptoms such as abdominal pain, rectal bleeding, unexplained weight loss, or persistent diarrhea, colonoscopy can help determine the underlying cause. It allows direct visualization of the colon’s lining and helps pinpoint the source of the problem.
- Polyp and Lesion Removal: During colonoscopy, gastroenterologists can remove polyps, lesions, or tissue samples for biopsy. This is crucial for both diagnosis and prevention. Polyps can be removed using specialized tools, reducing the risk of these polyps developing into cancer over time.
- Monitoring and Follow-Up: Patients who have a history of colorectal polyps, cancer, or other gastrointestinal issues may undergo regular colonoscopies to monitor their condition and ensure that no new abnormalities have developed.
- Evaluation of Treatment Effectiveness: For individuals with known gastrointestinal conditions, colonoscopy can be used to assess the effectiveness of treatments, surgeries, or interventions. It helps doctors determine if the treatment plan is working as expected.
- Guidance for Surgery: In some cases, colonoscopy can guide surgeons in planning procedures related to the colon, such as the removal of sections of the colon affected by disease.
- Management of Gastrointestinal Bleeding: Colonoscopy can be used to identify the source of gastrointestinal bleeding and, in some cases, to perform interventions to stop the bleeding.
- Health Monitoring for High-Risk Individuals: Individuals with a family history of colorectal cancer or certain genetic conditions may need more frequent or earlier colonoscopies as part of their health monitoring.
- Preventive Care for Elderly Patients: In some cases, elderly patients may undergo colonoscopy to ensure their overall health and to identify and address any gastrointestinal concerns that might arise.
Preparation for Colonoscopy:
- Consultation with Healthcare Provider: Before the colonoscopy, you will have a consultation with your healthcare provider to discuss the procedure, review your medical history, and address any questions or concerns you may have.
- Dietary Restrictions: Several days before the colonoscopy, you will need to follow a special diet that typically involves avoiding high-fiber foods, nuts, seeds, and foods with tough skins. This helps reduce the amount of residue in your colon.
- Bowel Preparation Medication: Your healthcare provider will prescribe a bowel preparation medication, often in the form of a powder that you mix with water. This medication will cause your bowel movements to be watery and help cleanse your colon. You will receive specific instructions on how to take the medication.
- Hydration: Staying hydrated is important during the preparation process. Drink plenty of clear liquids like water, clear broths, and clear juices. Avoid colored or red liquids, which could be mistaken for blood during the procedure.
- Clear Liquid Diet: The day before the colonoscopy, you will need to follow a clear liquid diet. This may include clear juices, broth, plain gelatin, and water. Avoid red or purple-colored liquids.
- Bowel Preparation Schedule: You will receive instructions on when to start taking the bowel preparation medication and when to finish. Typically, you will need to take the medication in divided doses over a few hours.
- Stay Close to a Bathroom: Expect to have frequent and urgent bowel movements as the bowel preparation takes effect. Stay near a bathroom during this time.
- Follow Instructions Carefully: It’s crucial to follow the preparation instructions provided by your healthcare provider to ensure that your colon is thoroughly cleansed. Inadequate preparation could lead to an incomplete or less effective colonoscopy.
- Medication Adjustments: Inform your healthcare provider about any medications you’re taking, as they might need to be adjusted during the preparation process.
- Transportation and Support: Since the procedure requires sedation or anesthesia, arrange for someone to drive you home afterward. You may not be fully alert for a few hours after the procedure.
- Preparation Kit: Some medical facilities provide preparation kits that include instructions, medications, and other supplies needed for the process.
Benefits of Colonoscopy:
Here are some key benefits of colonoscopy.
- Early Detection of Colorectal Cancer: Colonoscopy is one of the most effective methods for detecting colorectal cancer in its early stages. It allows for the identification and removal of precancerous polyps, which can significantly reduce the risk of cancer development.
- Polyp Identification and Removal: During a colonoscopy, gastroenterologists can identify and remove polyps before they become cancerous. This preventive measure reduces the likelihood of colorectal cancer development over time.
- Comprehensive Visualization: Colonoscopy provides a direct and thorough view of the entire colon’s lining. This comprehensive visualization allows for the detection of abnormalities, lesions, and other issues that might not be identified through other methods.
- Diagnosis of Gastrointestinal Conditions: Colonoscopy aids in the diagnosis of various gastrointestinal disorders, including inflammatory bowel diseases (IBD), diverticulosis, and other conditions. It allows for direct visualization and biopsy collection for accurate diagnosis.
- Treatment Planning: For individuals with known gastrointestinal conditions, colonoscopy helps healthcare providers evaluate the effectiveness of treatments, surgeries, or interventions. This information informs ongoing care and treatment plans.
- Personalized Risk Assessment: Colonoscopy can provide valuable information about an individual’s risk for colorectal cancer based on the presence of polyps, their size, and other factors. This information guides future screening recommendations.
- Preventive Health: Regular colonoscopies are an essential part of preventive healthcare, especially for individuals at higher risk due to factors such as family history or certain genetic conditions.
- Patient Peace of Mind: A clear colonoscopy result can provide reassurance and peace of mind, reducing anxiety about potential colorectal health concerns.
- Less Frequent Screening: If no significant findings are observed during a colonoscopy, individuals may not need to undergo another for several years, depending on their risk profile.
- Guidance for Future Care: Colonoscopy findings can guide healthcare providers in developing appropriate health management plans and strategies for individuals with specific risk factors or conditions.
- Focused Intervention: If polyps or lesions are identified during the colonoscopy, they can often be removed during the same procedure. This minimizes the need for additional invasive procedures.
Risks and Considerations:
Here are some risks and considerations associated with colonoscopy.
- Bleeding: During the removal of polyps or tissue samples, there is a small risk of bleeding. Most cases of bleeding are minor and resolve on their own, but in rare cases, additional medical intervention might be needed.
- Perforation: There is a small risk of perforation (puncture) of the colon or rectum during the procedure. This risk is higher when polyps are removed or when there are underlying gastrointestinal conditions. Perforation might require surgery to repair.
- Reaction to Sedation: The sedation or anesthesia used during the procedure can cause adverse reactions in some individuals. These reactions might include breathing difficulties, changes in heart rate, or low blood pressure. Healthcare providers carefully monitor patients during the procedure to minimize these risks.
- Infection: While rare, there’s a very small risk of infection at the site where the colonoscope was inserted. Healthcare providers take precautions to minimize infection risks.
- Incomplete Examination: Sometimes, due to factors like anatomic variations or discomfort, a complete examination of the colon might not be possible. This might necessitate repeat testing or alternative procedures.
- Discomfort and Cramping: Mild discomfort or cramping might occur during and after the procedure due to the air used to inflate the colon for better visualization. This discomfort is usually temporary.
- Preparation Challenges: The bowel preparation process can be challenging for some patients due to dietary restrictions and bowel cleansing medications. Inadequate preparation can affect the quality of the procedure.
- Allergic Reactions: In rare cases, patients might have an allergic reaction to medications used during the procedure or to the materials in the colonoscope.
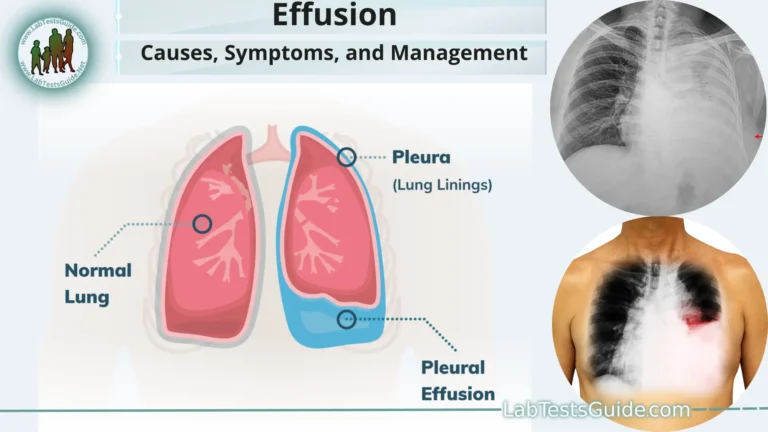
- Cardiovascular and Respiratory Risks: While colonoscopy is generally safe, any medical procedure carries a slight risk to individuals with pre-existing heart or lung conditions.
- Rare Complications: Extremely rare complications, such as adverse reactions to sedation, electrolyte imbalances, or other unforeseen issues, might occur.
The Colonoscopy Procedure:
- Preparation: Before the procedure, you will need to undergo thorough bowel preparation to ensure that your colon is clean and clear of stool, allowing for optimal visualization. This usually involves dietary restrictions and the use of bowel preparation medications to induce bowel movements that cleanse the colon.
- Arrival and Check-In: On the day of the procedure, you’ll arrive at the medical facility. You’ll complete any necessary paperwork and provide information about your medical history, allergies, and medications.
- Pre-Procedure Assessment: A nurse or healthcare provider will take your vital signs (such as blood pressure, heart rate, and oxygen levels) and review the procedure details with you. You may need to change into a hospital gown.
- Intravenous (IV) Line Placement: An IV line will be inserted into your arm. This will allow the administration of sedation and fluids during the procedure.
- Sedation: Most colonoscopies are performed under sedation to keep you comfortable and relaxed during the procedure. You’ll be given medications through the IV to induce a state of mild sedation or deeper anesthesia, depending on your provider’s approach and your preference.
- Positioning: You will be positioned on your side with your knees drawn up towards your chest. This position allows for easier insertion of the colonoscope.
- Insertion of the Colonoscope: The gastroenterologist will gently insert the colonoscope, which is a long, flexible tube with a light and camera at the end, through the anus and into the rectum. The scope is then carefully advanced through the colon.
- Visual Inspection: As the colonoscope is advanced, the camera captures real-time images of the colon’s lining. The images are displayed on a monitor, allowing the gastroenterologist to carefully examine the entire colon for abnormalities, such as polyps, inflammation, or tumors.
- Air or Carbon Dioxide Insufflation: To expand the colon and improve visualization, a small amount of air or carbon dioxide is gently pumped into the colon through the colonoscope.
- Biopsies or Polyp Removal: If any abnormalities are identified, the gastroenterologist can take biopsies (tiny tissue samples) for further examination. Polyps, if found, can often be removed during the procedure using specialized tools.
- Completion and Withdrawal: Once the examination is complete, the colonoscope is slowly withdrawn while the colon is carefully examined again.
- Recovery and Observation: After the procedure, you will be moved to a recovery area to allow the sedation to wear off. Your vital signs will be monitored, and you’ll rest until you are alert and able to tolerate fluids.
- Post-Procedure Discussion: The gastroenterologist will discuss the findings with you, including any biopsies taken or polyps removed. If necessary, further treatment or follow-up recommendations will be provided.
- Discharge: Once you are fully awake and meet the discharge criteria, you will be allowed to go home. If sedation was used, you will need someone to drive you.
After the Colonoscopy:
- Recovery Area: After the procedure is complete, you’ll be moved to a recovery area. Healthcare professionals will monitor your vital signs and ensure that you are waking up from any sedation or anesthesia safely.
- Post-Procedure Rest: You may feel groggy or drowsy after the procedure due to the sedation. Rest and take your time before attempting to get up or move around.
- Bloating and Gas: Some patients might experience bloating or gas after the procedure due to the air or carbon dioxide that was used to inflate the colon during the exam. This is temporary and should subside on its own.
- Clear Liquid Diet: You might start with clear liquids like water, clear broths, and clear juices as you recover. Avoid heavy or greasy foods until you feel more comfortable.
- Discharge Instructions: Before you’re discharged, the healthcare team will provide you with instructions for your recovery, including any dietary restrictions or other specific guidelines you should follow.
- Recovery Time: Recovery times vary, but many people are able to leave the medical facility within a few hours after the procedure, once they are fully alert and their vital signs are stable.
- Transportation: If you were sedated, you must arrange for someone to drive you home. The sedation can impair your ability to drive safely.
- Resuming Normal Activities: Depending on the sedation used and your comfort level, you might need to rest for the remainder of the day. Most people can resume normal activities the following day.
- Side Effects: It’s normal to experience mild cramping, bloating, or gas for a short time after the procedure. These symptoms should improve within a day or two.
- Biopsy Results: If biopsies were taken during the procedure, your doctor will discuss the results with you once they are available. This might happen during a follow-up appointment.
- Follow-Up Care: If any abnormalities were found, or if you had biopsies or polyps removed, your doctor will provide guidance on any necessary follow-up care, including future screenings.
- Stay Hydrated: Drink plenty of fluids to stay hydrated after the procedure.
- Contact Your Doctor: If you experience severe pain, bleeding, fever, or other concerning symptoms, contact your healthcare provider promptly.
Frequency and Follow-Up:
The general guideline for colonoscopy frequency and follow-up.
- Normal Screening: For individuals with no significant findings during their first colonoscopy, the next screening is typically recommended in 10 years.
- History of Polyps: If small, low-risk polyps are found and removed, a follow-up colonoscopy might be recommended in 5 to 10 years.
If larger or higher-risk polyps are found, the follow-up interval might be shorter, usually around 3 years. - Inflammatory Bowel Disease (IBD): Individuals with IBD, such as Crohn’s disease or ulcerative colitis, might require more frequent colonoscopies to monitor for inflammation, complications, or cancerous changes.
- Family History: Individuals with a family history of colorectal cancer or certain genetic conditions might need to start screenings earlier and have more frequent exams.
- Personal History of Colorectal Cancer: Individuals with a personal history of colorectal cancer might require more frequent colonoscopies to monitor for recurrence.
- High-Risk Conditions: Some genetic conditions, such as Lynch syndrome, increase the risk of colorectal cancer. Individuals with these conditions might need more frequent and earlier screenings.
- Age Considerations: In general, regular colonoscopies are recommended for individuals starting at age 50 for those with average risk. The frequency and timing might vary based on other factors.
- Alternatives to Colonoscopy: Depending on the results of other colorectal cancer screening methods, individuals might need colonoscopies sooner or more frequently.
FAQs:
What is a colonoscopy?
A colonoscopy is a medical procedure that uses a flexible tube with a camera (colonoscope) to visually examine the inside of the colon and rectum.
Why is a colonoscopy done?
Colonoscopy is performed for various reasons, including screening for colorectal cancer, diagnosing gastrointestinal disorders, investigating gastrointestinal symptoms, and removing polyps.
How do I prepare for a colonoscopy?
Preparation involves dietary restrictions and bowel cleansing using medications prescribed by your healthcare provider. Clear instructions will be provided.
Is sedation used during a colonoscopy?
Yes, sedation or anesthesia is often used to keep you comfortable and relaxed during the procedure.
How long does a colonoscopy take?
The procedure usually takes about 30 minutes to an hour, but this can vary based on factors like the complexity of the examination.
Does a colonoscopy hurt?
Most patients don’t experience pain during the procedure. You might feel mild discomfort or cramping.
What happens if polyps are found?
If polyps are found, they can often be removed during the same procedure. This is important for preventing potential cancer development.
When can I eat after the procedure?
You’ll typically start with clear liquids and progress to a regular diet as you feel comfortable, usually within a day after the procedure.
How often do I need a colonoscopy?
The frequency depends on your age, medical history, and the findings of previous screenings. Generally, if no significant findings are observed, a repeat colonoscopy might be recommended in 10 years.
What are the risks of a colonoscopy?
Risks include bleeding, perforation, reaction to sedation, and rare complications. Your healthcare provider will discuss these with you.
Can I drive myself home after the procedure?
If sedation is used, you’ll need someone to drive you home as you might not be fully alert.
Is there an alternative to colonoscopy for colorectal cancer screening?
Yes, there are alternatives like fecal occult blood tests (FOBT), fecal immunochemical tests (FIT), and virtual colonoscopy. Your provider can discuss which is best for you.
How should I choose a healthcare provider for a colonoscopy?
Choose a qualified gastroenterologist with experience in performing colonoscopies. Ask about their credentials and approach to patient care.
What should I do if I’m anxious about the procedure?
It’s natural to feel anxious. Discuss your concerns with your healthcare provider, and they can provide information and strategies to help ease your anxiety.
Conclusion:
In conclusion, a colonoscopy is a vital and effective medical procedure used for the early detection, diagnosis, and prevention of colorectal conditions, including colorectal cancer. By allowing direct visualization of the colon and rectum, it enables healthcare providers to identify abnormalities, remove polyps, and provide timely interventions, ultimately leading to improved health outcomes and reduced risks associated with colorectal diseases. While the procedure involves preparation and potential risks, its benefits in terms of disease prevention and management underscore its importance as a cornerstone of gastrointestinal healthcare.
Possible References Used