Staphylococcus aureus is a type of bacteria that is commonly found on the skin and in the nose of healthy people. However, it can also cause a variety of infections, including skin infections, pneumonia, and sepsis.
Staphylococcus aureus is a Gram-positive, round-shaped bacterium that is a member of the Firmicutes, and it is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin.

Staphylococcus Aureus Overview:
- Staphylococcus Aureus Overview: Staphylococcus aureus, commonly known as “Staph,” is a bacterium found on the skin and mucous membranes of humans. While often harmless, it can cause a range of infections, from mild skin issues to severe, life-threatening diseases.
- Staphylococcus Aureus Infections: Staphylococcus aureus can lead to various infections, such as skin and soft tissue infections, respiratory infections, bloodstream infections, and even more severe conditions like pneumonia and sepsis.
- MRSA – Methicillin-Resistant Staphylococcus Aureus: MRSA is a strain of Staphylococcus aureus that has become resistant to common antibiotics, making it challenging to treat and posing a significant public health concern.
- Transmission and Prevention: Staphylococcus aureus is mainly transmitted through direct contact with infected individuals or contaminated surfaces. Proper hygiene practices, such as handwashing and wound care, are essential to prevent its spread.
- Laboratory Diagnosis of Staphylococcus Aureus: Accurate diagnosis of Staphylococcus aureus involves various laboratory techniques, including Gram staining, culture, biochemical tests, and molecular methods like PCR.
- Virulence Factors and Toxins: Staphylococcus aureus produces toxins and virulence factors that contribute to its pathogenicity, causing tissue damage and evading the immune system.
- Treatment of Staphylococcus Aureus Infections: Effective treatment of Staph infections requires antibiotics, but due to increasing resistance, alternative drugs may be needed, especially in the case of MRSA infections.
- Staphylococcus Aureus in Healthcare Settings: Healthcare-associated MRSA (HA-MRSA) infections are a concern in hospitals and long-term care facilities, emphasizing the importance of infection control measures.
- Community-Acquired MRSA (CA-MRSA): CA-MRSA is acquired outside healthcare facilities, often through close skin contact in the community, and has different characteristics from HA-MRSA.
- Emerging Trends in Staphylococcus Aureus Research: Ongoing research focuses on understanding Staphylococcus aureus better, developing new diagnostic methods, and finding innovative treatments for drug-resistant strains.
Classification of Staphylococcus Aureus:
| Classification | Description |
|---|---|
| Domain | Bacteria |
| Phylum | Firmicutes |
| Class | Bacilli |
| Order | Bacillales |
| Family | Staphylococcaceae |
| Genus | Staphylococcus |
| Species | Staphylococcus aureus |
| Gram Stain | Positive (Purple) |
| Shape | Spherical (Cocci) |
| Growth Characteristics | Facultative Anaerobe (Grows with or without oxygen) |
| Catalase Test | Positive (Produces bubbles when exposed to hydrogen peroxide) |
| Coagulase Test | Positive (Forms clots in coagulase test) |
| Hemolytic Activity | Beta-hemolytic (Complete lysis of red blood cells on blood agar) |
| Motility | Non-motile |
| Toxin Production | Produces various toxins contributing to pathogenicity |
| Pathogenicity | Can cause a range of infections in humans and animals |
| Antibiotic Susceptibility | Becoming a significant concern due to antibiotic resistance, particularly MRSA (Methicillin-resistant Staphylococcus aureus) |
Transmission of Staphylococcus aureus:
Staphylococcus aureus is primarily transmitted through:
- Direct Contact: The bacteria can be transmitted through skin-to-skin contact with an infected individual.
- Contaminated Surfaces: Staphylococcus aureus can survive on surfaces, objects, and medical equipment, leading to indirect transmission if a person touches these contaminated items.
- Respiratory Droplets: In rare cases, Staphylococcus aureus can be transmitted through respiratory droplets when an infected person coughs or sneezes.
- Healthcare Settings: In hospitals and healthcare facilities, Staphylococcus aureus can spread through contaminated medical equipment or through contact with healthcare workers or patients.
- Community Settings: Staphylococcus aureus can spread in community environments, such as schools, gyms, and households, through close contact and shared items.
Habitat of Staphylococcus aureus
- The natural habitat is the body surfaces of mammals.
- They are normal flora of the skin and mucous membranes.
- Also present in the nose / anterior nostrils.
- They can also be found in Pharynx.
- It is found in stratified epithelial cells or in mucosal or serum components associated with these cells.
- It is found in the skin / nasal passages and armpits of humans.
- They act as a benign or symbiotic relationship with the hosts.
- Enterogeneric strains of S. aureus are found in various food products.
- They can survive on dry skin.
- Thirty percent (30%) of the normal healthy human population is affected by S. aureus, as it asymptomatically colonizes the skin of the human host.
Morphology of Staphylococcus Aureus:
| Morphological Characteristics | Description |
|---|---|
| Shape | Spherical (Cocci) |
| Arrangement | Grape-like clusters |
| Gram Stain | Gram-positive |
| Cell Wall | Thick peptidoglycan layer |
| Capsule | May or may not possess a capsule |
| Motility | Non-motile |
| Spore Formation | Non-spore forming |
| Size | Approximately 0.5 to 1.5 micrometers |
| Pigment Production | May produce golden-yellow pigment (staphyloxanthin) on culture media |
| Hemolytic Activity | Beta-hemolytic (complete lysis of red blood cells on blood agar) |
| Catalase Test | Positive (produces bubbles when exposed to hydrogen peroxide) |
| Coagulase Test | Positive (forms clots in coagulase test) |
Causes and Symptoms of Staphylococcus Aureus:
Causes of Staphylococcus Aureus Infections:
Staphylococcus aureus infections are caused by the bacterium Staphylococcus aureus. The bacteria can enter the body through cuts, wounds, or breaks in the skin, leading to localized infections. It can also enter the body through the respiratory tract, causing respiratory infections, or through the bloodstream, leading to more severe systemic infections. Staphylococcus aureus is highly adaptable and can colonize various body sites, making it a common cause of both community-acquired and healthcare-associated infections.
Symptoms of Staphylococcus Aureus Infections:
The symptoms of Staphylococcus aureus infections can vary depending on the type and severity of the infection. Some common symptoms include:
- Skin Infections: These may manifest as redness, swelling, warmth, and pain at the site of infection. Common skin infections caused by Staphylococcus aureus include boils, abscesses, impetigo, and cellulitis.
- Respiratory Infections: Symptoms may include cough, shortness of breath, chest pain, and fever. Pneumonia caused by Staphylococcus aureus can be severe, especially in vulnerable individuals.
- Bloodstream Infections: Also known as bacteremia, these can lead to symptoms such as fever, chills, rapid heartbeat, low blood pressure, and body aches. Bacteremia can be life-threatening and may lead to sepsis if left untreated.
- Bone and Joint Infections: Symptoms may include joint pain, swelling, redness, and limited range of motion. Osteomyelitis (bone infection) and septic arthritis are examples of bone and joint infections caused by Staphylococcus aureus.
- Toxic Shock Syndrome (TSS): In rare cases, Staphylococcus aureus can produce toxins that lead to TSS, characterized by sudden high fever, rash, low blood pressure, and multi-organ failure.
- Food Poisoning: Consumption of food contaminated with Staphylococcus aureus toxins can cause rapid-onset symptoms like nausea, vomiting, stomach cramps, and diarrhea.
Virulence Factors of Staphylococcus Aureus:
- Staphylococcal Protein A (SpA): Binds to the Fc region of immunoglobulins, interfering with the host’s immune response and preventing antibody-mediated clearance of the bacteria.
- Coagulase: Converts fibrinogen to fibrin, causing clot formation around the bacteria, protecting it from immune defenses and facilitating its persistence at the infection site.
- Hemolysins: Produces various hemolysins, including alpha-hemolysin and beta-hemolysin, which can destroy red blood cells and other host cells, leading to tissue damage and inflammation.
- Exotoxins: Staphylococcus aureus produces a range of exotoxins, such as toxic shock syndrome toxin (TSST-1) and enterotoxins, which can cause toxic shock syndrome and food poisoning, respectively.
- Panton-Valentine Leukocidin (PVL): A cytotoxin that targets white blood cells, causing cell lysis and tissue destruction, contributing to severe skin and soft tissue infections.
- Biofilm Formation: Staphylococcus aureus can produce a protective biofilm on surfaces, enabling bacterial adherence, colonization, and evasion of the immune system, making it difficult to treat infections associated with biofilm.
- Capsule: Some strains produce a polysaccharide capsule, protecting the bacteria from phagocytosis by immune cells, enhancing its ability to cause invasive infections.
- Superantigens: Activate a large number of T-cells, leading to an exaggerated immune response, contributing to inflammation and tissue damage in various infections.
- Protein Toxins: Staphylococcus aureus can secrete protein toxins, such as exfoliative toxins, which cause skin desquamation (peeling) in conditions like staphylococcal scalded skin syndrome.
- Enterotoxins: Associated with food poisoning, enterotoxins can cause gastrointestinal symptoms like nausea, vomiting, and diarrhea upon ingestion.
Pathogenesis of Staphylococcus Aureus:
- Adherence: Staphylococcus aureus attaches to host tissues using surface proteins and adhesins, establishing colonization sites.
- Virulence Factors: The bacterium produces toxins, enzymes, and proteins that contribute to tissue damage and evasion of the host’s immune system.
- Tissue Damage and Inflammation: Staphylococcus aureus releases toxins that damage host cells, leading to inflammation at the infection site.
- Immune Evasion: The bacterium employs various mechanisms to evade the host’s immune response, enabling its survival and persistence.
- Invasion and Dissemination: Depending on the infection site, Staphylococcus aureus can invade deeper tissues or spread through the bloodstream to other organs.
- Biofilm Formation: In some cases, the bacterium can produce biofilms, making it more resistant to antibiotics and host defenses.
- Toxin-Mediated Syndromes: Certain strains produce toxins responsible for specific syndromes, such as toxic shock syndrome and food poisoning.
Diagnosis of Staphylococcus Aureus:
- Gram Stain: A rapid test to stain the specimen and identify Staphylococcus aureus as Gram-positive cocci in clusters.
- Culture and Isolation: Placing the specimen on agar plates to allow bacterial growth and obtain characteristic colonies.
- Biochemical Tests: Tests to identify specific metabolic characteristics of Staphylococcus aureus, including the catalase test (positive) and coagulase test (positive).
- Molecular Tests: PCR and genetic testing to detect specific genes, including those related to antibiotic resistance like mecA gene in MRSA.
- Antibiotic Susceptibility Testing: Determining the sensitivity of the isolated strain to antibiotics, guiding appropriate treatment.
- Toxin Detection: In certain syndromes, toxin detection may be necessary to confirm Staphylococcus aureus as the cause, e.g., enterotoxin testing in food poisoning.
- Identification of MRSA: Additional tests to confirm methicillin-resistant Staphylococcus aureus (MRSA) strains.
- Serological Assays: In specific situations, serological tests may be used to detect antibodies against Staphylococcus aureus or its toxins.
Clinical Manifestation of Staphylococcus Aureus:
Staphylococcus aureus can cause a wide range of clinical manifestations depending on the site of infection and the virulence factors produced by the bacterium. Here are some common clinical manifestations associated with Staphylococcus aureus infections:
- Skin and Soft Tissue Infections: Staphylococcus aureus can cause various skin infections, including:
- Boils (furuncles) and abscesses
- Impetigo (superficial skin infection)
- Cellulitis (infection of deeper skin layers)
- Folliculitis (inflammation of hair follicles)
- Carbuncles (collection of interconnected boils)
- Respiratory Infections: Staphylococcus aureus can lead to respiratory tract infections, such as:
- Staphylococcal pneumonia
- Sinusitis (inflammation of the sinuses)
- Pharyngitis (sore throat)
- Bloodstream Infections: Staphylococcus aureus can cause bacteremia (bacteria in the bloodstream), which can lead to more severe conditions like sepsis.
- Bone and Joint Infections: Staphylococcus aureus can infect bones (osteomyelitis) and joints (septic arthritis), causing pain, swelling, and limited movement.
- Toxic Shock Syndrome (TSS): In rare cases, certain strains of Staphylococcus aureus can produce toxins that lead to toxic shock syndrome, characterized by sudden high fever, rash, low blood pressure, and multi-organ failure.
- Food Poisoning: Staphylococcus aureus can produce heat-stable enterotoxins in food, causing rapid-onset symptoms like nausea, vomiting, stomach cramps, and diarrhea.
- Endocarditis: Staphylococcus aureus can infect the heart valves, leading to endocarditis, which may cause symptoms like fever, fatigue, and heart murmurs.
- Pneumonia: Staphylococcus aureus pneumonia can cause symptoms like cough, shortness of breath, chest pain, and fever.
- Skin and Soft Tissue Necrosis: In severe infections, Staphylococcus aureus can cause tissue necrosis (cell death), leading to conditions like necrotizing fasciitis or staphylococcal scalded skin syndrome.
Laboratory Diagnosis of Staphylococcus Aureus:
The laboratory diagnosis of Staphylococcus aureus involves a series of tests and procedures to identify and confirm the presence of the bacterium in clinical specimens. Here is an overview of the laboratory diagnostic process:
- Specimen Collection: Samples are collected from the suspected infection site, such as wound swabs, blood, respiratory secretions, or other body fluids.
- Gram Stain: A rapid initial test where the specimen is stained with crystal violet dye and iodine, followed by alcohol wash and safranin counterstain. Staphylococcus aureus appears as Gram-positive cocci in clusters.
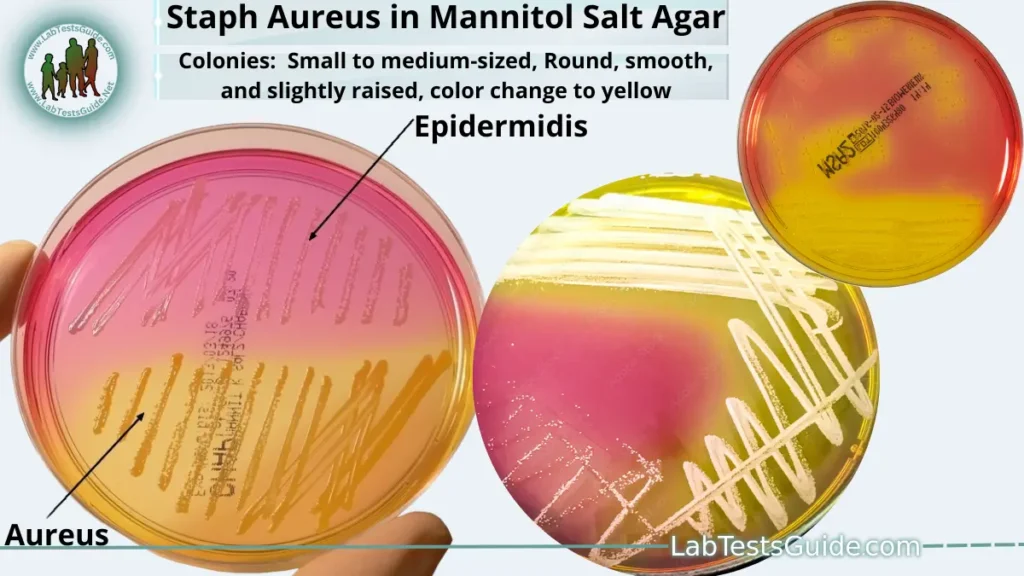
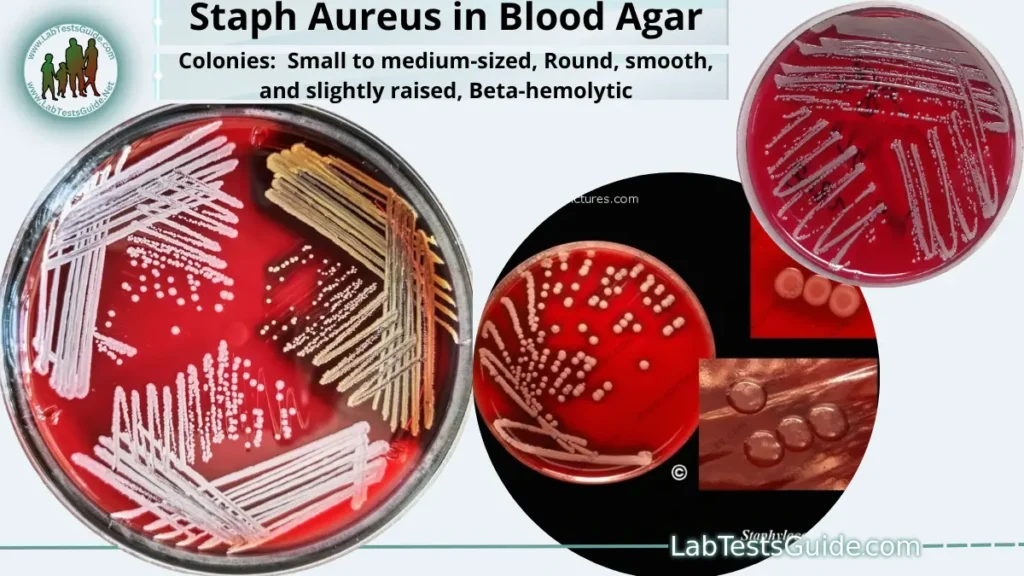
- Culture and Isolation: The collected specimens are cultured on appropriate agar plates, such as blood agar or mannitol salt agar. Staphylococcus aureus typically forms distinct colonies with characteristic features, such as golden-yellow color on mannitol salt agar.
- Biochemical Tests: Additional biochemical tests may be performed to identify specific metabolic characteristics of Staphylococcus aureus, such as fermentation of sugars and production of certain enzymes.
- Molecular Tests: Polymerase chain reaction (PCR) and other molecular methods can detect specific genetic markers of Staphylococcus aureus, including genes responsible for antibiotic resistance, such as mecA gene in MRSA.
- Antibiotic Susceptibility Testing: Testing is performed to determine the sensitivity of the isolated Staphylococcus aureus strain to various antibiotics. This helps guide appropriate antibiotic treatment.
- Toxin Detection: In some cases, detection of specific toxins (e.g., enterotoxins) may be necessary to confirm Staphylococcus aureus as the cause of certain syndromes like food poisoning.
- Identification of MRSA: Additional tests, such as the cefoxitin disk diffusion test or PCR for mecA gene, are used to confirm methicillin-resistant Staphylococcus aureus (MRSA).
Gram Stain:
A rapid initial test where the specimen is stained with crystal violet dye and iodine, followed by alcohol wash and safranin counterstain. Staphylococcus aureus appears as Gram-positive cocci in clusters.
Here’s an overview of the Gram staining procedure:
- Preparation of a Bacterial Smear: A small amount of the bacterial sample is placed on a glass slide and allowed to air-dry. Heat fixation is then performed to adhere the bacteria to the slide and kill them, making them safe for handling in the laboratory.
- Application of Crystal Violet: The slide is flooded with crystal violet, a purple-colored dye that binds to the peptidoglycan layer (cell wall) of all bacteria.
- Iodine Treatment: Iodine is applied to the slide as a mordant, forming a complex with the crystal violet inside the bacterial cells. This step enhances the retention of the dye.
- Decolorization: The slide is briefly washed with alcohol or acetone to remove the excess crystal violet-iodine complex from the Gram-negative bacteria. The thick peptidoglycan layer of Gram-positive bacteria traps the dye, making them less susceptible to decolorization.
- Counterstaining: Safranin, a red-colored dye, is applied to the slide. It serves as a counterstain, imparting a contrasting color to the Gram-negative bacteria, which lost the crystal violet-iodine complex during decolorization.
- Microscopic Examination: The slide is then observed under a light microscope. Gram-positive bacteria appear purple due to the retention of the crystal violet dye, while Gram-negative bacteria appear red, as they take up the safranin counterstain.
Culture and Isolation:
The collected specimens are cultured on appropriate agar plates, such as blood agar or mannitol salt agar. Staphylococcus aureus typically forms distinct colonies with characteristic features, such as golden-yellow color on mannitol salt agar.
Culture and isolation are fundamental techniques used in microbiology to grow and separate bacteria from a mixed sample, allowing for the identification and study of specific bacterial species. Here’s an overview of the culture and isolation process:
- Sample Collection: A specimen or sample containing bacteria is collected from the source of interest, such as a patient’s wound, blood, sputum, or environmental source.
- Inoculation: The collected sample is inoculated onto a culture medium, which provides the necessary nutrients for bacterial growth. Different types of culture media can support the growth of various bacteria and help isolate specific species.
- Incubation: The inoculated culture medium is placed in a controlled incubator at an optimal temperature, usually around 37°C for most human pathogens. This promotes the growth and multiplication of bacteria over time.
- Colonial Growth: Bacteria from the original sample multiply and form visible colonies on the surface of the culture medium. Each colony typically originates from a single bacterial cell or a few genetically identical cells.
- Isolation Streaking: To obtain pure cultures of specific bacteria, a technique called isolation streaking is used. A loop or sterile swab is used to streak a small sample from a single colony onto a new area of the culture medium. This process is repeated several times, each time transferring fewer bacteria to separate individual colonies.
- Incubation of Isolated Colonies: The culture medium with isolated colonies is again incubated to allow the growth of distinct bacterial isolates.
- Observation and Identification: After sufficient growth, the isolated colonies are observed for their appearance, color, shape, size, and other characteristics. Bacterial identification may involve performing Gram staining, biochemical tests, and other specific tests to identify the species.
Colony Characteristics of Staphylococcus Aureus:
| Colony Characteristics | Description |
|---|---|
| Shape | Circular, small to medium-sized colonies |
| Color | Typically off-white, cream, or yellowish color Some strains may produce golden-yellow pigment |
| Surface Texture | Smooth or slightly rough |
| Elevation | Raised or convex |
| Margin | Entire and well-defined |
| Hemolysis | Beta-hemolytic on blood agar (complete lysis of red blood cells) |
| Growth on Mannitol Salt Agar | Ferments mannitol, causing a change in agar color to yellow |
| Coagulase Test | Positive (causes clots in coagulase test) |
| Catalase Test | Positive (produces bubbles when exposed to hydrogen peroxide) |
Colonies on Different Agars:
| Agar Type | Colony Appearance |
|---|---|
| Blood Agar | Small to medium-sized colonies Round, smooth, and slightly raised Beta-hemolytic (clear zone around colonies) |
| Mannitol Salt Agar | Small to medium-sized colonies Round, smooth, and raised Ferments mannitol, causing agar color change to yellow |
| MacConkey Agar | Does not grow (Staphylococcus aureus is gram-positive) |
| Eosin Methylene Blue Agar | Does not grow (Staphylococcus aureus is gram-positive) |
| Sabouraud Agar | Does not grow (selective for fungi) |
| Chocolate Agar | Small to medium-sized colonies Round, smooth, and raised Non-hemolytic (no change in agar color) |
Antibiotic Susceptibility Testing (AST):
Testing is performed to determine the sensitivity of the isolated Staphylococcus aureus strain to various antibiotics. This helps guide appropriate antibiotic treatment.
- Ampicillin/sulbactam
- Amoxicillin/clavulanate
- Oxacillin
- Nafcillin
- Cefazolin
- Ceftriaxone
- Macrolides
- Clindamycin
- vancomycin
- teicoplanin
- linezolid
- quinupristin/dalfopristin
- TMP-SMX
- Rifampicin
Biochemical Test of Staphylococcus aureus:
Additional biochemical tests may be performed to identify specific metabolic characteristics of Staphylococcus aureus, such as fermentation of sugars and production of certain enzymes.
| Basic Characteristics | Staphylococcus aureus |
|---|---|
| Capsule | Non-Capsulated |
| Catalase | Positive (+ve) |
| Citrate | Positive (+ve) |
| Coagulase | Positive (+ve) |
| Gas | Negative (-ve) |
| Gelatin Hydrolysis | Positive (+ve) |
| Gram Staining | Positive (+ve) |
| H2S | Negative (-ve) |
| Hemolysis | Positive (+ve)- Beta |
| Indole | Negative (-ve) |
| Motility | Negative (-ve) |
| MR (Methyl Red) | Positive (+ve) |
| Nitrate Reduction | Positive (+ve) |
| OF (Oxidative-Fermentative) | Fermentative |
| Oxidase | Negative (-ve) |
| Pigment | Mostly Positive (+ve) |
| PYR | Negative (-ve) |
| Shape | Cocci |
| Spore | Non-Sporing |
| Urease | Positive (+ve) |
| VP (Voges Proskauer) | Positive (+ve) |
| Arabinose | Negative (-ve) |
| Cellobiose | Negative (-ve) |
| DNase | Positive (+ve) |
| Fructose | Positive (+ve) |
| Galactose | Positive (+ve) |
| Glucose | Positive (+ve) |
| Lactose | Positive (+ve) |
| Maltose | Positive (+ve) |
| Mannitol | Positive (+ve) |
| Mannose | Positive (+ve) |
| Raffinose | Negative (-ve) |
| Ribose | Positive (+ve) |
| Salicin | Negative (-ve) |
| Sucrose | Positive (+ve) |
| Trehalose | Positive (+ve) |
| Xylose | Negative (-ve) |
| Acetoin Production | Positive (+ve) |
| Alkaline Phosphatase | Positive (+ve) |
| Arginine Dehydrolase | Positive (+ve) |
| Hyalurodinase | Positive (+ve) |
| Lipase | Positive (+ve) |
| Ornithine Decarboxylase | Negative (-ve) |
Molecular Tests:
Polymerase chain reaction (PCR) and other molecular methods can detect specific genetic markers of Staphylococcus aureus, including genes responsible for antibiotic resistance, such as mecA gene in MRSA.
Toxin Detection:
In some cases, detection of specific toxins (e.g., enterotoxins) may be necessary to confirm Staphylococcus aureus as the cause of certain syndromes like food poisoning.
Toxin detection is a laboratory method used to identify the presence of specific toxins produced by bacteria, viruses, or other microorganisms in clinical specimens. For Staphylococcus aureus, toxin detection is essential for diagnosing toxin-mediated syndromes and food poisoning caused by the bacterium. Here are some common methods used for toxin detection in Staphylococcus aureus infections:
- Enzyme Immunoassays (EIA): EIA, also known as enzyme-linked immunosorbent assay (ELISA), is a commonly used technique for detecting toxins. It involves using specific antibodies that bind to the target toxin in the clinical specimen. If the toxin is present, it will bind to the antibody-enzyme complex, resulting in a color change that can be measured.
- PCR-Based Assays: Polymerase chain reaction (PCR) can be used to detect genes that encode for Staphylococcus aureus toxins, such as enterotoxins responsible for food poisoning. If the target genes are present in the clinical specimen, it indicates the presence of the toxin-producing bacterium.
- Cell-Based Assays: In some cases, cell-based assays are used to detect the activity of toxins. These assays involve exposing cultured cells to the clinical specimen, and if the toxin is present, it will cause specific cellular changes or damage that can be observed under a microscope.
- Immunodiffusion: Immunodiffusion techniques, such as double immunodiffusion (Ouchterlony technique), are used to detect and identify toxins based on their antigen-antibody reactions in gel plates.
- Mass Spectrometry: Mass spectrometry is a powerful analytical technique that can detect and identify toxins based on their molecular weight and fragmentation patterns.
Identification of MRSA:
Additional tests, such as the cefoxitin disk diffusion test or PCR for mecA gene, are used to confirm methicillin-resistant Staphylococcus aureus (MRSA).
The identification of MRSA (methicillin-resistant Staphylococcus aureus) involves specific laboratory tests to detect the presence of the mecA gene, which confers resistance to methicillin and other beta-lactam antibiotics. Here’s an overview of the methods used to identify MRSA:
- Cefoxitin Disk Diffusion Test: This is a rapid and simple test where a cefoxitin antibiotic disk is placed on an agar plate inoculated with Staphylococcus aureus. If the bacteria are resistant to methicillin, they will also be resistant to cefoxitin, causing a zone of inhibition around the disk indicating MRSA.
- Oxacillin Agar Screen Test: Similar to the cefoxitin test, this method uses an oxacillin-containing agar plate. If the isolate shows resistance to oxacillin, it is considered MRSA.
- Molecular Methods (PCR): Polymerase chain reaction (PCR) is a highly sensitive and specific technique used to detect the presence of the mecA gene in Staphylococcus aureus isolates. The mecA gene is responsible for methicillin resistance. If the mecA gene is detected, the isolate is confirmed as MRSA.
Main diseases caused by Staphylococcus aureus
- Skin Infections & Surgical wound infections
- Osteomyelitis
- Food poisoning/gastroenteritis
- Toxic shock syndrome
- Pneumonia (mainly hospital acquired)
- Acute endocarditis
- Infective arthritis
- Necrotizing fasciitis
- Sepsis and Staphylococcal scalded skin syndrome (SSSS)
Prevention of Staphylococcus aureus infection
- Proper wound cleaning and the use of disinfectants help prevent infection.
- Thorough hand washing and covering exposed skin help medical personnel prevent infection or spread to other patients.
- Patients and staff carrying epidemic strains, particularly MRSA, should be isolated.
- Patients can be given disinfectant baths or treated with a topical antibiotic to eradicate the transport of MRSA.
- Infection control programs should be used in hospitals.
Treatment of Staphylococcus aureus infection
- Localized infections are treated by incision and drainage, while antibiotic therapy is indicated for systemic infections.
- Oral therapy may include trimethoprim-sulfamethoxazole, doxycycline or minocycline, clindamycin, or linezolid; Vancomycin is the drug of choice for intravenous therapy, with daptomycin, tigecycline, or linezolid as acceptable alternatives.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections acquired in the hospital and in the community are a major global problem. Therefore, empirical therapy should include antibiotics active against MRSA strains.
- Treatment is symptomatic for patients with food poisoning (although the source of infection must be identified so that appropriate preventive procedures can be implemented)
Related Articles:
Possible References Used