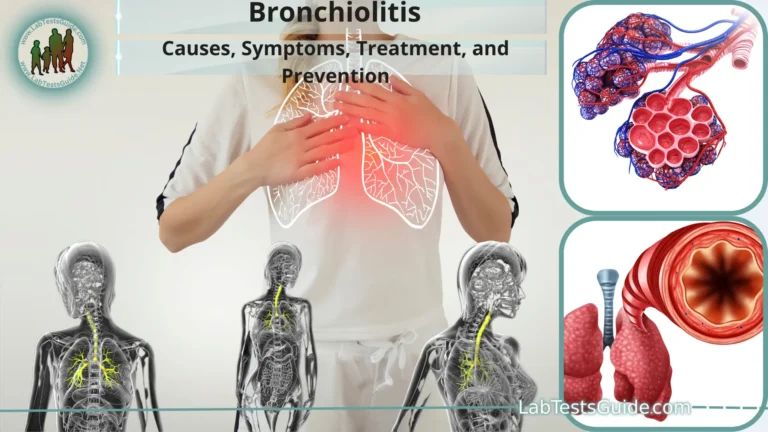
Bronchiectasis is a chronic respiratory condition characterized by the abnormal widening and damage to the bronchial tubes (airways) in the lungs. This damage results in the accumulation of mucus and makes it difficult for the affected person to clear this mucus from their airways. Over time, this can lead to recurrent lung infections and respiratory symptoms.

What Is Bronchiectasis?
Bronchiectasis is a chronic respiratory condition characterized by the abnormal widening and damage to the bronchial tubes (airways) in the lungs. In a healthy respiratory system, the airways are flexible and maintain their shape, allowing air to flow freely in and out of the lungs. However, in bronchiectasis, these airways become damaged and lose their elasticity, resulting in a permanent and abnormal dilation (widening) of the bronchi.
Causes and Underlying Conditions:
Here are some of the common causes and underlying conditions associated with bronchiectasis.
- Infections: Repeated or severe lung infections, such as pneumonia, bronchitis, or tuberculosis, can lead to bronchiectasis. These infections can cause inflammation and damage to the airways, resulting in the characteristic widening seen in bronchiectasis.
- Cystic Fibrosis: Cystic fibrosis (CF) is a genetic condition that affects the respiratory and digestive systems. In CF, a defective gene causes the production of thick and sticky mucus, which can obstruct the airways and lead to bronchiectasis over time.
- Autoimmune Diseases: Some autoimmune diseases, such as rheumatoid arthritis, Sjögren’s syndrome, and systemic lupus erythematosus, can cause chronic inflammation in the body. This inflammation may extend to the airways and contribute to the development of bronchiectasis.
- Allergic Bronchopulmonary Aspergillosis (ABPA): ABPA is a condition in which the immune system has an exaggerated response to the fungus Aspergillus. This condition can lead to inflammation and damage to the airways, increasing the risk of bronchiectasis.
- Primary Ciliary Dyskinesia (PCD): PCD is a rare genetic disorder that affects the cilia, which are tiny hair-like structures lining the respiratory tract. When cilia do not function properly, they are unable to effectively clear mucus and foreign particles from the airways, potentially leading to bronchiectasis.
- Immune Deficiency: Certain immune deficiencies, such as selective IgA deficiency or common variable immunodeficiency (CVID), can result in recurrent and severe respiratory infections, which may contribute to bronchiectasis.
- Aspiration: Inhaling foreign objects, liquids, or gastric contents into the lungs (aspiration) can lead to chronic inflammation and lung damage, potentially resulting in bronchiectasis.
- Obstructive Airway Conditions: Conditions that cause chronic airway obstruction, such as chronic obstructive pulmonary disease (COPD) or severe asthma, can lead to bronchiectasis due to persistent inflammation and mucus accumulation.
- Environmental Exposures: Prolonged exposure to environmental irritants, such as smoke, pollutants, or toxic fumes, can contribute to chronic airway inflammation and bronchiectasis in some individuals.
Symptoms of Bronchiectasis:
Common symptoms of bronchiectasis include.
- Chronic Cough: Individuals with bronchiectasis often have a persistent cough that may produce mucus or phlegm. This cough can be particularly troublesome and may worsen over time.
- Excessive Mucus Production: One of the hallmark symptoms is the increased production of mucus, which is typically thick and sticky. This mucus can contribute to airway blockages and recurrent infections.
- Shortness of Breath: As the airways become damaged and narrowed, it becomes more difficult for air to move in and out of the lungs. This can result in a sensation of breathlessness, especially during physical activity.
- Wheezing: Wheezing is a high-pitched whistling sound produced during breathing and is often heard in people with bronchiectasis due to the narrowed and obstructed airways.
- Chest Pain: Some individuals may experience chest discomfort or pain, which can result from coughing or infections in the lungs.
- Fatigue: Chronic coughing, difficulty breathing, and recurrent infections can lead to fatigue and a decreased ability to engage in regular activities.
- Recurrent Lung Infections: Bronchiectasis makes the airways more susceptible to infections, leading to frequent respiratory infections, including bronchitis and pneumonia.
- Clubbing of Fingers and Toes: In severe cases of bronchiectasis, the fingertips and toes may develop clubbing, a condition in which the ends of the fingers and toes become enlarged and the nails curve around the fingertips.
- Blood in the Sputum: In some instances, people with bronchiectasis may cough up blood or have blood-tinged mucus. This is known as hemoptysis and should be evaluated by a healthcare professional.
- Weight Loss: Unintentional weight loss can occur in individuals with bronchiectasis, often due to reduced appetite and increased energy expenditure from chronic coughing and breathing difficulties.
Prevention and Risk Reduction:
Here are some prevention and risk reduction strategies.
- Vaccinations: Ensure that you and your children are up-to-date with vaccinations, including those for influenza (flu) and pneumonia. These vaccines can help prevent respiratory infections that can lead to bronchiectasis.
- Respiratory Hygiene: Practice good respiratory hygiene to reduce the risk of respiratory infections. This includes covering your mouth and nose when coughing or sneezing, using tissues or your elbow, and disposing of tissues properly.
- Infection Control: If you have a chronic respiratory condition or a weakened immune system, take extra precautions to avoid exposure to infections. This may include avoiding close contact with sick individuals and practicing good hand hygiene.
- Manage Chronic Conditions: If you have conditions that can contribute to bronchiectasis, such as cystic fibrosis or autoimmune diseases, work closely with your healthcare team to manage these conditions effectively.
- Avoid Smoking and Secondhand Smoke: Smoking is a major risk factor for lung disease, including bronchiectasis. If you smoke, seek support to quit. Additionally, avoid exposure to secondhand smoke, as it can also harm your lungs.
- Environmental Factors: Limit exposure to environmental pollutants and irritants that can damage the airways. This includes reducing exposure to air pollution, occupational hazards, and indoor allergens like mold and dust mites.
- Proper Nutrition: Maintain a healthy diet and maintain a healthy weight. Good nutrition can support overall health and immune function.
- Stay Active: Regular physical activity can help maintain lung function and overall health. Consult with your healthcare provider to determine an appropriate exercise routine.
- Manage Gastroesophageal Reflux Disease (GERD): If you have GERD, which can contribute to bronchiectasis, work with your healthcare provider to manage and treat this condition effectively.
- Bronchial Clearance Techniques: If you have a condition that makes it difficult to clear mucus from your airways, such as cystic fibrosis, you may benefit from specific airway clearance techniques. Consult with a respiratory therapist or specialist for guidance.
- Early Intervention: If you develop respiratory symptoms or recurrent lung infections, seek prompt medical attention. Early diagnosis and treatment of respiratory conditions can help prevent complications like bronchiectasis.
- Medication Adherence: If you have a chronic respiratory condition that requires medication, adhere to your prescribed treatment plan diligently. This can help control the underlying disease and reduce the risk of complications.
Diagnosis of Bronchiectasis:
Here are the key steps and methods used in the diagnosis of bronchiectasis.
- Medical History: Your healthcare provider will start by taking a detailed medical history, which may include asking about your symptoms, their duration, and any risk factors or underlying conditions that could contribute to bronchiectasis.
- Physical Examination: A physical examination can help your healthcare provider assess your lung function and listen for abnormal breath sounds, such as wheezing or crackles, using a stethoscope.
Imaging Studies:
- Chest X-ray: While a chest X-ray can provide a preliminary evaluation of the lungs, it may not always show early or mild cases of bronchiectasis.
- High-Resolution Computed Tomography (HRCT) Scan: This imaging test is the gold standard for diagnosing bronchiectasis. HRCT provides detailed images of the lungs, allowing for the visualization of dilated airways and areas of lung damage.
- Pulmonary Function Tests (PFTs): Lung function tests may be performed to assess how well your lungs are functioning. Spirometry and other PFTs can help determine the extent of airflow obstruction or restriction.
- Sputum Analysis: A sample of your sputum (mucus coughed up from your lungs) may be collected and analyzed in a laboratory to check for signs of infection, including bacteria or fungi. This can help guide treatment decisions.
- Bronchoscopy: In some cases, a bronchoscopy may be performed. During this procedure, a thin, flexible tube with a camera on the end (bronchoscope) is inserted through the nose or mouth and into the airways. This allows for direct visualization of the airways and the collection of tissue samples (biopsy) if needed.
- Blood Tests: Blood tests may be conducted to check for signs of inflammation or to investigate potential underlying causes, such as autoimmune diseases.
- Sweat Test: If cystic fibrosis is suspected as the underlying cause of bronchiectasis, a sweat test may be performed to measure the amount of salt (sodium and chloride) in your sweat. Elevated levels can indicate cystic fibrosis.
- Genetic Testing: In cases where a genetic condition is suspected, genetic testing may be recommended to identify specific gene mutations associated with bronchiectasis.
- Allergy Testing: If allergies are believed to contribute to bronchiectasis, allergy testing may help identify allergens that trigger respiratory symptoms.
- Lung Biopsy: In rare cases, a lung biopsy may be necessary to examine lung tissue for more detailed information about the extent of lung damage and the underlying cause. This procedure is typically reserved for situations where other diagnostic tests do not provide a clear diagnosis.
Treatment and Management:
Here are the key components of treatment and management.
Medications:
- Antibiotics: Antibiotics are prescribed to treat and prevent lung infections, which are common in bronchiectasis. Depending on the severity and type of infection, antibiotics may be given orally, through inhalation, or intravenously.
- Bronchodilators: Bronchodilator medications help relax and widen the airways, making it easier to breathe. They may be used if airflow obstruction is present.
- Mucolytics: Mucolytic medications help thin and loosen mucus, making it easier to clear from the airways. This can help reduce coughing and improve airflow.
- Chest Physiotherapy: Techniques such as postural drainage, percussion, and vibration may be taught by a respiratory therapist to help clear mucus from the airways. These techniques are often part of a daily regimen for individuals with bronchiectasis.
- Pulmonary Rehabilitation: Pulmonary rehabilitation programs include exercise training, education, and counseling to improve lung function and overall quality of life. These programs are tailored to each individual’s needs.
- Surgery: In severe cases of bronchiectasis with localized lung damage that does not respond to other treatments, surgery may be considered. Surgical options include lung resection (removing damaged portions of the lung) or lung transplant.
Lifestyle Modifications:
- Smoking Cessation: If you smoke, quitting is crucial as smoking can worsen bronchiectasis and increase the risk of infections.
- Environmental Modifications: Avoid environmental irritants such as air pollution, allergens, and occupational hazards that can exacerbate lung symptoms.
- Hydration: Staying well-hydrated can help keep mucus from becoming too thick and sticky, making it easier to clear from the airways.
- Nutrition: A balanced diet can support overall health and immune function. Consult a dietitian if needed.
- Vaccinations: Stay up-to-date on recommended vaccinations, including those for influenza and pneumonia, to reduce the risk of respiratory infections.
- Manage Underlying Conditions: If bronchiectasis is secondary to an underlying condition, such as cystic fibrosis or autoimmune diseases, managing and treating that condition is essential.
- Monitoring and Follow-Up: Regular follow-up appointments with a healthcare provider are necessary to monitor lung function, adjust treatment plans, and address any changes in symptoms.
- Patient Education: Learning about bronchiectasis and self-management strategies is essential. Education helps individuals better understand their condition, medications, and how to recognize and respond to worsening symptoms.
- Psychosocial Support: Living with a chronic respiratory condition can be emotionally challenging. Seek support from friends, family, support groups, or mental health professionals as needed.
Understanding the Respiratory System:
- Airway and Nose: The respiratory process begins when air is inhaled through the nose or mouth. The nose serves as a primary entrance for air, where it is filtered, moistened, and warmed before reaching the lower respiratory tract.
- Pharynx and Larynx: The air passes from the nose or mouth into the pharynx and then to the larynx.
The larynx contains the vocal cords and functions in sound production. - Trachea (Windpipe): The trachea is a tube composed of cartilage rings that carries air from the larynx to the bronchi. It is lined with cilia (tiny hair-like structures) and mucus-producing cells that help trap and remove foreign particles and bacteria from the air.
- Bronchi and Bronchioles: The trachea divides into two main bronchi, one leading to each lung.
The bronchi further divide into smaller bronchioles, which eventually lead to the tiny air sacs called alveoli. - Alveoli: Alveoli are small, grape-like structures within the lungs where the actual gas exchange takes place. Oxygen from the inhaled air diffuses into the bloodstream, while carbon dioxide from the bloodstream diffuses into the alveoli to be exhaled.
- Lungs: The lungs are paired, spongy organs that house the bronchi, bronchioles, and alveoli.
The right lung has three lobes, while the left lung has two lobes, accommodating the heart.
Diaphragm and Respiratory Muscles:
- Breathing is controlled by the diaphragm, a large, dome-shaped muscle located at the base of the lungs.
- When the diaphragm contracts (moves downward), it increases the volume of the chest cavity, causing air to be drawn into the lungs (inhalation).
- When the diaphragm relaxes (moves upward), the chest cavity decreases in volume, leading to exhalation.
- Other muscles in the ribcage also aid in breathing by expanding or contracting the chest cavity.
- Respiratory Control Center: The brainstem contains the respiratory control center, which regulates the rate and depth of breathing in response to changes in blood oxygen and carbon dioxide levels.
- Gas Exchange: Oxygen is transported in the bloodstream bound to hemoglobin in red blood cells.
Carbon dioxide is transported in the blood in various forms, primarily as bicarbonate ions, and is released into the alveoli for exhalation. - Exhalation: Exhalation is a passive process that occurs as a result of the relaxation of the diaphragm and respiratory muscles, causing the chest cavity to decrease in size and expel air.
Complications and Long-Term Effects:
Here are some of the potential complications and long-term effects associated with bronchiectasis.
- Recurrent Respiratory Infections: Individuals with bronchiectasis are prone to frequent respiratory infections, such as bronchitis and pneumonia. These infections can lead to worsening lung damage over time and may require repeated courses of antibiotics.
- Chronic Cough and Sputum Production: The persistent cough and excessive production of thick, sticky mucus can be distressing and interfere with daily activities, impacting overall quality of life.
- Progressive Lung Damage: Bronchiectasis is characterized by the irreversible widening and scarring of the airways. Over time, this damage can lead to a decline in lung function, making it progressively more difficult to breathe.
- Respiratory Failure: In severe cases, bronchiectasis can lead to respiratory failure, where the lungs are unable to provide adequate oxygen to the bloodstream or remove carbon dioxide efficiently. This can result in a need for supplemental oxygen therapy or mechanical ventilation.
- Chest Pain and Discomfort: Chronic coughing and lung infections can cause chest pain and discomfort, impacting an individual’s daily life and ability to engage in physical activities.
- Hemoptysis: In some cases, individuals with bronchiectasis may cough up blood or have blood-tinged mucus (hemoptysis). This requires immediate medical attention to determine the cause and appropriate treatment.
- Nutritional Issues: Frequent respiratory infections and difficulty breathing can lead to reduced appetite and weight loss, potentially affecting overall nutrition and energy levels.
- Decreased Exercise Tolerance: As lung function declines, individuals with bronchiectasis may experience reduced exercise tolerance and limitations in physical activities.
- Pulmonary Hypertension: In advanced cases, chronic lung damage can lead to pulmonary hypertension, a condition characterized by high blood pressure in the arteries of the lungs, which can strain the heart.
- Psychological and Emotional Impact: Living with a chronic respiratory condition can have psychological and emotional effects, including anxiety, depression, and reduced quality of life.
- Complications from Medications: Long-term use of medications, particularly antibiotics, can have side effects and may lead to antibiotic resistance.
- Secondary Infections: Frequent respiratory infections can increase the risk of secondary infections in other parts of the body.
- Impact on Daily Life: The symptoms and limitations associated with bronchiectasis can affect an individual’s ability to work, engage in social activities, and enjoy a normal life.
Prognosis and Outlook:
Here are some key considerations regarding prognosis and outlook.
- Early Diagnosis and Treatment: Early diagnosis and prompt initiation of treatment are crucial for improving the prognosis. Early intervention can help prevent or delay the progression of lung damage and reduce the frequency and severity of respiratory infections.
- Underlying Cause: Identifying and addressing the underlying cause of bronchiectasis is important. For example, if the condition is related to an underlying condition like cystic fibrosis, managing the primary condition can significantly improve the outlook.
- Treatment Adherence: Adherence to prescribed medications, airway clearance techniques, and other treatment recommendations is essential for managing symptoms and preventing complications. Individuals who follow their treatment plans diligently tend to have better outcomes.
- Lifestyle and Self-Care: Adopting a healthy lifestyle, including smoking cessation, maintaining good nutrition, staying physically active, and managing environmental triggers, can positively impact the prognosis.
- Pulmonary Rehabilitation: Participating in pulmonary rehabilitation programs can help improve lung function, exercise tolerance, and overall quality of life.
- Regular Monitoring: Regular follow-up with healthcare providers for lung function tests and imaging studies allows for the early detection of changes in lung health and adjustments to treatment plans.
- Supportive Care: Psychosocial support, including counseling and support groups, can help individuals cope with the emotional and psychological aspects of living with a chronic respiratory condition.
- Complications: Prompt management of complications such as respiratory infections, hemoptysis (coughing up blood), and exacerbations can prevent more serious health issues.
- Individual Variability: It’s important to recognize that the progression of bronchiectasis can vary from person to person. Some individuals may experience stable lung function for years, while others may have a more rapid decline.
- Advanced Disease: In advanced cases with significant lung damage, the prognosis may be less favorable, and individuals may require oxygen therapy or lung transplantation.
FAQs:
What is bronchiectasis?
Bronchiectasis is a chronic respiratory condition characterized by the permanent widening and damage to the airways in the lungs, leading to increased mucus production, persistent cough, and recurrent respiratory infections.
What causes bronchiectasis?
Bronchiectasis can be caused by various factors, including recurrent lung infections, autoimmune diseases, inhaling foreign objects, and genetic conditions like cystic fibrosis.
What are the common symptoms of bronchiectasis?
Common symptoms include chronic cough, excessive mucus production, shortness of breath, wheezing, recurrent lung infections, and fatigue.
How is bronchiectasis diagnosed?
Diagnosis involves a combination of medical history, physical examination, imaging studies (usually a high-resolution CT scan), pulmonary function tests, sputum analysis, and sometimes bronchoscopy.
Can bronchiectasis be cured?
Bronchiectasis is typically a chronic condition, and the underlying lung damage is usually irreversible. However, with appropriate treatment and management, symptoms can be controlled, and complications can be minimized.
What is the treatment for bronchiectasis?
Treatment may include antibiotics to treat infections, bronchodilators to open airways, mucolytics to thin mucus, chest physiotherapy, pulmonary rehabilitation, and in some cases, surgery.
Is bronchiectasis contagious?
No, bronchiectasis itself is not contagious. It is a non-communicable respiratory condition. However, the underlying infections that can occur in bronchiectasis may be contagious.
Can bronchiectasis be prevented?
Preventing bronchiectasis involves managing underlying causes, avoiding respiratory infections, practicing good respiratory hygiene, and addressing environmental factors that may contribute to lung damage.
What is the prognosis for bronchiectasis?
The prognosis varies depending on factors like the underlying cause, severity of lung damage, and how well it’s managed. With early diagnosis and appropriate care, many people with bronchiectasis can lead relatively normal lives.
Is there a cure for bronchiectasis?
There is no cure for bronchiectasis, but treatment can help manage symptoms, prevent complications, and improve the quality of life for individuals with the condition.
Conclusion:
In conclusion, bronchiectasis is a chronic respiratory condition characterized by irreversible damage to the airways in the lungs, leading to symptoms such as chronic cough, excess mucus production, and recurrent infections. While it is not curable, early diagnosis, proper management, and lifestyle modifications can significantly improve the prognosis and quality of life for individuals with bronchiectasis. Treatment strategies, including medications, airway clearance techniques, and pulmonary rehabilitation, aim to control symptoms, prevent complications, and promote overall lung health. Regular monitoring and adherence to recommended therapies, along with addressing underlying causes, are essential components of effective bronchiectasis management.
Possible References Used