Brittle diabetes, also known as labile diabetes, is a rare and severe form of diabetes mellitus characterized by extreme fluctuations in blood sugar levels. People with brittle diabetes experience frequent and unpredictable swings between high blood sugar (hyperglycemia) and low blood sugar (hypoglycemia), often without apparent cause.

Definition of Brittle diabetes.
Brittle diabetes is a term used to describe an uncommon and severe form of diabetes mellitus characterized by extreme and unpredictable fluctuations in blood sugar levels. Unlike the stable blood sugar control typically seen in most individuals with diabetes, those with brittle diabetes experience rapid and severe swings between high blood sugar (hyperglycemia) and low blood sugar (hypoglycemia), often without an obvious trigger or apparent cause.
Causes and Risk Factors:
Here are some common causes and risk factors.
- Insulin Sensitivity and Production Issues: Problems with insulin sensitivity or insufficient insulin production by the pancreas can contribute to unstable blood sugar levels. In some cases, individuals with brittle diabetes may have a severe form of insulin resistance, making it difficult for insulin to regulate their blood sugar effectively.
- Hormonal Imbalances: Hormonal fluctuations, such as those associated with conditions like polycystic ovary syndrome (PCOS) or thyroid disorders, can impact blood sugar control and contribute to the brittleness of diabetes.
- Medication Interactions: Some medications, including certain drugs used to treat other medical conditions, can interfere with the action of insulin or other diabetes medications, leading to blood sugar instability.
- Stress: High levels of stress, whether from daily life stressors, emotional factors, or illness, can significantly affect blood sugar levels. Stress hormones like cortisol can cause blood sugar to rise.
- Inadequate Diabetes Management: Poor adherence to medication regimens, irregular meal patterns, and inconsistent monitoring of blood sugar levels can all contribute to blood sugar fluctuations.
- Dietary Factors: Inconsistent or erratic eating habits, as well as consumption of foods that cause rapid spikes or drops in blood sugar (e.g., sugary snacks or high-carbohydrate meals), can lead to instability in blood sugar levels.
- Alcohol and Substance Use: The consumption of alcohol or certain drugs can disrupt blood sugar regulation and contribute to hypoglycemia or hyperglycemia.
- Underlying Medical Conditions: Coexisting medical conditions, such as gastroparesis (delayed stomach emptying), can affect digestion and nutrient absorption, making it challenging to manage blood sugar levels.
- Psychological Factors: Emotional factors, including anxiety, depression, and other mental health issues, can impact diabetes management. Stress and emotional distress can lead to erratic blood sugar patterns.
- Individual Variability: Some individuals may simply be more prone to extreme blood sugar fluctuations due to genetic or physiological factors.
- Infections or Illness: Illnesses and infections can stress the body and affect blood sugar levels, making it harder to maintain stable control.
Symptoms and Diagnosis:
Here are some common symptoms and information on the diagnosis of brittle diabetes.
Symptoms of Hyperglycemia (High Blood Sugar):
- Excessive Thirst: Feeling constantly thirsty and drinking large amounts of fluids.
- Frequent Urination: Urinating more frequently than usual.
- Fatigue: Persistent tiredness and lack of energy.
- Blurred Vision: Vision may become blurry or hazy.
- Increased Hunger: Constant feelings of hunger, even after eating.
- Dry Skin and Mouth: Skin may become dry, and the mouth may feel parched.
- Frequent Infections: High blood sugar levels can weaken the immune system, leading to an increased risk of infections.
Symptoms of Hypoglycemia (Low Blood Sugar):
- Sweating: Profuse sweating, especially when not exerting physically.
- Trembling or Shaking: Uncontrollable trembling or shivering.
- Rapid Heartbeat: Heart palpitations and a fast heartbeat.
- Dizziness: Feeling lightheaded or dizzy.
- Irritability: Sudden mood changes, including irritability or nervousness.
- Confusion: Difficulty concentrating or thinking clearly.
- Hunger: Intense hunger and cravings for sugary foods.
- Weakness: Muscle weakness or a feeling of extreme fatigue.
- Headache: A persistent headache.
Diagnosis of Brittle Diabetes:
- Medical History: The process of diagnosing brittle diabetes typically begins with a detailed medical history. A healthcare provider will ask about symptoms, blood sugar patterns, medication regimens, diet, lifestyle, and any underlying medical conditions.
- Blood Sugar Monitoring: Continuous or frequent monitoring of blood sugar levels is essential. This may involve using a blood glucose meter to track daily fluctuations. Patterns of extreme highs and lows over time may raise suspicion of brittle diabetes.
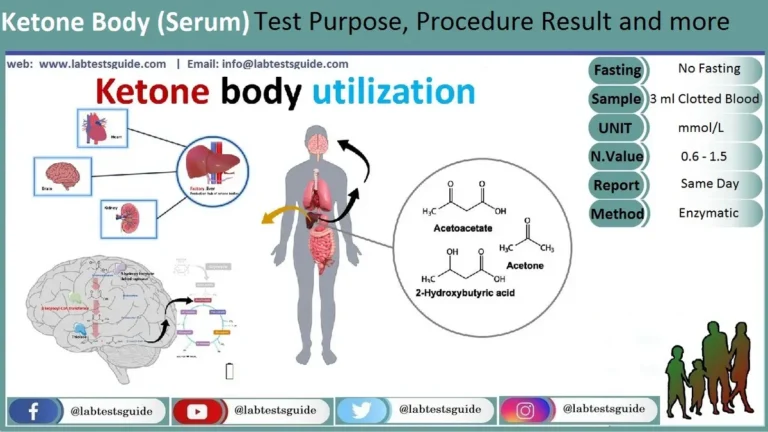
- Hemoglobin A1c Test: This blood test provides an average of blood sugar levels over the past two to three months. Individuals with brittle diabetes may still have a high A1c, indicating poor long-term blood sugar control, despite experiencing frequent fluctuations.
- C-peptide Test: This test measures the level of C-peptide in the blood, which can help determine the body’s ability to produce insulin. Low levels of C-peptide may suggest reduced insulin production.
- Other Tests: Additional tests may be ordered to investigate underlying factors contributing to brittle diabetes, such as hormonal imbalances or coexisting medical conditions.
- Psychological Assessment: Because stress and psychological factors can significantly impact blood sugar control, a psychological assessment may be conducted to evaluate the emotional well-being of the individual.
Management and Treatment:
Here are the key components of managing and treating brittle diabetes.
Blood Sugar Monitoring:
- Frequent blood sugar monitoring is essential. Some individuals may benefit from continuous glucose monitoring (CGM) systems, which provide real-time data on blood sugar levels.
- Keeping a detailed record of blood sugar readings, meals, activities, and symptoms can help identify patterns and triggers.
Medications and Insulin Therapy:
- Medications and insulin therapy are typically necessary to regulate blood sugar levels.
- A healthcare provider will prescribe insulin regimens tailored to the individual’s needs, which may include multiple daily injections or insulin pump therapy.
- Continuous subcutaneous insulin infusion (CSII) through an insulin pump allows for precise insulin delivery and flexibility in adjusting basal and bolus insulin doses.
Dietary Management:
- Working with a registered dietitian or nutritionist to create a customized meal plan is crucial. The plan should focus on consistent carbohydrate intake and meal timing to help stabilize blood sugar levels.
- Monitoring carbohydrate intake, portion control, and making healthier food choices can also contribute to better blood sugar control.
Lifestyle Modifications:
- Regular physical activity can improve insulin sensitivity and contribute to blood sugar stability. It’s important to discuss an exercise plan with a healthcare provider to avoid hypoglycemia during or after physical activity.
- Adequate sleep and stress management techniques, such as relaxation exercises or meditation, can help reduce stress-related blood sugar fluctuations.
Psychological Support:
- Managing the psychological aspects of brittle diabetes is essential. Stress, anxiety, and depression can trigger blood sugar fluctuations. Psychotherapy, counseling, or support groups can be beneficial in addressing these emotional factors.
Medication Adjustments:
- Medication regimens may need frequent adjustments based on changes in blood sugar patterns, lifestyle factors, and other considerations.
- Some individuals may require medications that address specific aspects of blood sugar control, such as incretin-based therapies or medications that reduce insulin resistance.
- Hormonal Management: If hormonal imbalances contribute to brittle diabetes, addressing these imbalances with appropriate medications or treatments may be necessary.
- Regular Medical Checkups: Routine follow-up visits with healthcare providers, including endocrinologists and diabetes educators, are important for ongoing assessment, monitoring, and adjustments to the treatment plan.
- Emergency Preparedness: Individuals with brittle diabetes and their caregivers should be educated on how to respond to severe hypoglycemia or hyperglycemia episodes, including the administration of glucagon (for severe hypoglycemia) or seeking medical assistance during diabetic ketoacidosis (DKA).
- Continuous Education: Staying informed about the latest diabetes management techniques, technologies, and research can help individuals make informed decisions about their care.
Challenges in Managing Brittle Diabetes:
Here are some of the key challenges associated with managing brittle diabetes.
- Blood Sugar Variability: The hallmark of brittle diabetes is the erratic and unpredictable blood sugar fluctuations. Managing these extreme highs and lows can be challenging, as they can occur suddenly and without an apparent trigger.
- Hyperglycemia and Hypoglycemia: Individuals with brittle diabetes are at risk of both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) episodes. Balancing blood sugar levels within a narrow range is often difficult.
- Unpredictable Triggers: Identifying the specific triggers for blood sugar fluctuations can be elusive. Factors such as stress, illness, hormonal changes, and medication interactions can contribute, but the exact cause may not always be clear.
- Medication Adjustments: Frequent adjustments to medication regimens, including insulin doses and types, are often necessary to manage blood sugar levels effectively. Finding the right balance can be a complex and ongoing process.
- Dietary Challenges: Maintaining a consistent and balanced diet is crucial for blood sugar control. However, the unpredictable nature of brittle diabetes can make it challenging to plan meals and avoid extreme blood sugar spikes or crashes.
- Psychological Impact: The emotional toll of living with brittle diabetes can be substantial. The constant worry and anxiety about blood sugar fluctuations can lead to stress, depression, and a reduced quality of life.
- Emergency Situations: Individuals with brittle diabetes are at a higher risk of severe hypoglycemia or diabetic ketoacidosis (DKA). Knowing how to respond to these emergencies and having access to the necessary supplies and support is crucial.
- Complex Treatment Plans: Managing brittle diabetes often requires a multidisciplinary approach involving endocrinologists, dietitians, mental health professionals, and other specialists. Coordinating care and adhering to complex treatment plans can be overwhelming.
- Financial Burden: The costs associated with managing brittle diabetes, including medications, insulin, medical devices, and frequent healthcare visits, can place a significant financial burden on individuals and their families.
- Social Isolation: Managing brittle diabetes may limit participation in social activities, as individuals may need to closely monitor their blood sugar levels, adhere to specific meal schedules, or deal with the effects of blood sugar fluctuations in social situations.
- Continuous Education: Staying informed about the latest advancements in diabetes management and technology is essential, but it can also be time-consuming and overwhelming.
Medical Care and Support:
Here are key aspects of medical care and support for individuals with brittle diabetes.
- Endocrinologist Care: An endocrinologist is a medical specialist with expertise in hormonal disorders, including diabetes. Regular visits to an endocrinologist are crucial for monitoring blood sugar control, adjusting treatment plans, and addressing any hormonal imbalances that may contribute to brittle diabetes.
- Diabetes Educators: Diabetes educators play a vital role in educating individuals with brittle diabetes about the condition, insulin administration, blood sugar monitoring, and lifestyle management. They provide practical guidance for daily self-care.
- Registered Dietitians/Nutritionists: Working with a registered dietitian or nutritionist helps individuals develop customized meal plans that support stable blood sugar control. These professionals can assist in managing carbohydrate intake, portion sizes, and overall dietary choices.
- Mental Health Support: Managing the psychological aspects of brittle diabetes is crucial. Mental health professionals, such as psychologists or counselors, can help individuals cope with stress, anxiety, and depression that may arise due to the condition. Support groups can also provide a sense of community and understanding.
- Continuous Glucose Monitoring (CGM): CGM systems provide real-time data on blood sugar levels, allowing individuals and healthcare providers to track fluctuations and make timely adjustments to insulin therapy and lifestyle choices.
- Insulin Pump Therapy: For some individuals with brittle diabetes, insulin pump therapy may offer better control and flexibility in managing insulin delivery. Endocrinologists and diabetes educators can assist with selecting and adjusting insulin pumps.
- Medication Management: Healthcare providers regularly review and adjust medication regimens, including insulin doses and types, to address blood sugar fluctuations and improve control.
- Emergency Preparedness: Individuals and their caregivers should be educated on how to respond to severe hypoglycemia or hyperglycemia episodes. This includes knowing how to administer glucagon (for severe hypoglycemia) or recognizing signs of diabetic ketoacidosis (DKA).
- Regular Health Checkups: In addition to diabetes-related care, individuals with brittle diabetes should continue to receive routine health checkups to monitor overall health and detect any potential complications early.
- Coordination of Care: Effective communication and coordination among healthcare providers, including primary care physicians, specialists, and support staff, are critical to ensure that all aspects of care are addressed and that treatment plans are well-coordinated.
- Education and Empowerment: Empowering individuals with brittle diabetes through education about their condition, treatment options, and self-care strategies can enhance their ability to manage their diabetes effectively.
- Access to Resources: Individuals with brittle diabetes should have access to the necessary supplies, medications, and technologies required for their care. Access to insurance coverage and financial assistance programs can also be crucial.
Complications:
Here are some of the potential complications.
Diabetic Ketoacidosis (DKA):
- DKA is a life-threatening complication that can occur during periods of severe hyperglycemia. It is characterized by the accumulation of ketones in the blood, leading to acidosis. Symptoms include excessive thirst, frequent urination, abdominal pain, vomiting, rapid breathing, and confusion. DKA requires immediate medical attention and treatment with insulin and fluids.
Hypoglycemic Complications:
- Severe hypoglycemia (low blood sugar) can result in unconsciousness, seizures, and, in extreme cases, coma or death if not promptly treated. Hypoglycemic episodes may require the administration of glucagon or rapid-acting carbohydrates to raise blood sugar levels.
Neuropathy (Nerve Damage):
- Frequent and severe blood sugar fluctuations can contribute to nerve damage (neuropathy). This can lead to symptoms such as numbness, tingling, and pain, often affecting the hands and feet. Autonomic neuropathy may also impact the digestive, cardiovascular, and urinary systems.
Retinopathy (Eye Damage):
- Prolonged exposure to high blood sugar levels can damage the blood vessels in the retina, leading to diabetic retinopathy. This condition can cause vision problems, including blurred vision and, in severe cases, blindness.
Nephropathy (Kidney Damage):
- Kidney damage can occur as a result of prolonged hyperglycemia. It may progress to diabetic nephropathy, leading to impaired kidney function or kidney failure. Early detection and management are essential to slow or prevent this complication.
Cardiovascular Complications:
- Uncontrolled blood sugar levels increase the risk of cardiovascular issues, such as heart disease, hypertension, and stroke. Individuals with brittle diabetes may also be at a higher risk of experiencing sudden and severe changes in blood pressure during hyperglycemic or hypoglycemic episodes.
Foot Complications:
- Neuropathy and impaired circulation due to diabetes can lead to foot problems, including ulcers, infections, and, in severe cases, amputations. Regular foot care and monitoring are essential.
Mental Health Issues:
- Living with brittle diabetes can take a toll on mental health. The stress, anxiety, and depression that can result from constant blood sugar fluctuations and the challenges of managing the condition can impact overall well-being.
Delayed Wound Healing:
- Poor blood sugar control can hinder the body’s ability to heal wounds, increasing the risk of infections and complications from injuries or surgeries.
Gastroparesis:
- This condition, characterized by delayed stomach emptying, can lead to erratic digestion and absorption of nutrients, making it more challenging to manage blood sugar levels and overall health.
Cognitive Function:
- Fluctuations in blood sugar levels, especially hypoglycemic episodes, may have short-term and long-term effects on cognitive function, memory, and mental clarity.
Research and Future Directions:
Here are some research areas and future directions in the field of brittle diabetes.
- Precision Medicine: Researchers are exploring the potential for precision medicine approaches to tailor diabetes treatments to individual patients. This includes considering genetic factors, insulin sensitivity, and other biomarkers to develop personalized treatment plans.
- Advanced Continuous Glucose Monitoring (CGM): Ongoing research is focused on improving the accuracy and reliability of CGM systems. This includes the development of next-generation sensors and algorithms that can better predict blood sugar fluctuations.
- Closed-Loop Insulin Delivery: The development of closed-loop or “artificial pancreas” systems continues to be a major area of research. These systems aim to automate insulin delivery based on real-time glucose data, reducing the burden of manual insulin adjustments.
- Hormonal Therapies: Research is ongoing to explore hormonal therapies, such as incretin-based medications and other novel approaches, to improve blood sugar control in individuals with brittle diabetes, particularly those with underlying hormonal imbalances.
- Stem Cell Therapy: Investigational studies are exploring the potential of stem cell therapy to restore beta cell function in type 1 diabetes, which could provide a more stable source of insulin production.
- Behavioral Interventions: Research into the psychological and behavioral aspects of diabetes management is vital. This includes examining interventions to reduce diabetes-related stress and improve coping strategies.
- Telemedicine and Digital Health: Advances in telemedicine and digital health technologies are changing the way individuals with brittle diabetes receive care. Remote monitoring, virtual consultations, and mobile apps for diabetes management are areas of active research.
- Genetic Studies: Genetic research is shedding light on the genetic factors that may predispose individuals to brittle diabetes. Identifying these genetic markers could lead to targeted therapies.
- Microbiome Research: The gut microbiome’s role in diabetes management is a growing area of interest. Research is exploring how gut bacteria may influence blood sugar control and how microbiome-related interventions could help.
- Patient-Reported Outcomes: Studies are focusing on understanding the impact of brittle diabetes on patients’ quality of life and well-being. This includes research into the psychosocial aspects of the condition and interventions to improve mental health outcomes.
- Access to Care: Addressing healthcare disparities and ensuring equitable access to diabetes care and technology is a pressing research concern, particularly in underserved communities.
- Prevention Strategies: While brittle diabetes often arises in individuals with longstanding diabetes, there is research into strategies for preventing the development of brittle patterns in newly diagnosed individuals.
FAQs:
What is brittle diabetes?
Brittle diabetes is a rare and severe form of diabetes characterized by extreme and unpredictable fluctuations in blood sugar levels.
What causes brittle diabetes?
The exact cause can vary, but it often results from factors like insulin sensitivity issues, hormonal imbalances, medication interactions, stress, and psychological factors.
How is brittle diabetes diagnosed?
Diagnosis involves blood sugar monitoring, hemoglobin A1c tests, C-peptide tests, and a thorough medical history and physical examination.
What are the symptoms of brittle diabetes?
Symptoms include excessive thirst, frequent urination, fatigue, blurred vision, confusion, sweating, and symptoms of both hyperglycemia and hypoglycemia.
How is brittle diabetes managed and treated?
Treatment includes blood sugar monitoring, insulin therapy, dietary management, lifestyle modifications, and psychological support.
What are the complications of brittle diabetes?
Complications can include diabetic ketoacidosis (DKA), severe hypoglycemia, neuropathy, retinopathy, nephropathy, cardiovascular issues, and mental health challenges.
Is there a cure for brittle diabetes?
There is no cure, but management can improve blood sugar control and reduce complications.
Can people with brittle diabetes lead normal lives?
With proper care and support, individuals with brittle diabetes can lead fulfilling lives, but it may require more diligence in diabetes management.
Is brittle diabetes the same as type 1 diabetes?
Brittle diabetes can occur in both type 1 and type 2 diabetes, but it’s not synonymous with either. It’s a term used to describe unstable blood sugar patterns.
What are the treatment options for severe hypoglycemia in brittle diabetes?
Severe hypoglycemia may require glucagon administration or the help of others to raise blood sugar levels. Preventing hypoglycemia is a primary goal.
Can brittle diabetes be prevented?
Preventing brittle diabetes may not always be possible, but achieving good blood sugar control from the beginning of a diabetes diagnosis can help minimize the risk.
Is there ongoing research into brittle diabetes?
Yes, ongoing research aims to better understand brittle diabetes, improve treatment options, and enhance the quality of life for individuals with this condition.
Conclusion:
In summary, brittle diabetes represents a complex and uncommon form of diabetes marked by severe and unpredictable fluctuations in blood sugar levels, posing significant challenges to those affected. However, with the guidance of dedicated healthcare professionals, personalized treatment plans encompassing blood sugar monitoring, insulin therapy, dietary management, and psychological support can significantly enhance the quality of life for individuals with this condition. Ongoing research and advancements in diabetes care offer hope for improved management strategies, fostering the potential for more stable blood sugar control and a brighter future for those living with brittle diabetes.
Possible References Used