Anticoagulants, also known as blood thinners, are medications that help prevent the formation of blood clots in the circulatory system. Blood clots can be dangerous as they can block blood flow, leading to serious medical conditions like deep vein thrombosis (DVT), pulmonary embolism (PE), stroke, and heart attack.
Definition of Anticoagulants.
Anticoagulants are substances or medications that inhibit or slow down the process of blood clotting (coagulation). They work by interfering with various components of the coagulation cascade, preventing the formation of blood clots within the bloodstream. Anticoagulants are used medically to prevent or treat conditions characterized by excessive or harmful blood clot formation, such as deep vein thrombosis, pulmonary embolism, atrial fibrillation, and certain cardiovascular conditions. They help reduce the risk of dangerous blood clots that can lead to strokes, heart attacks, or other serious medical complications.
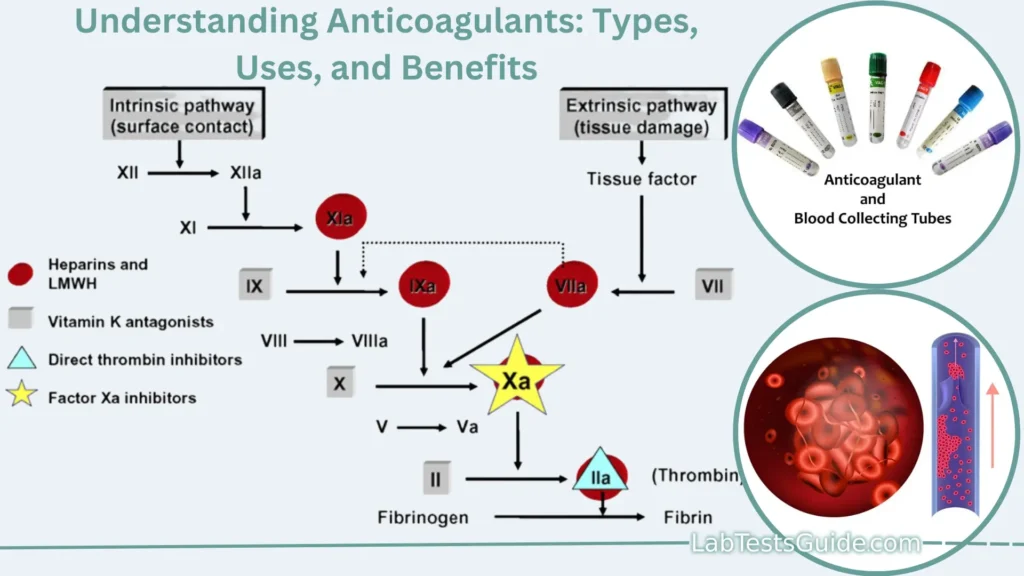
Mechanism of Action:
- Inhibition of Clotting Factors: Anticoagulants target specific clotting factors in the blood, which are proteins that play key roles in the clotting process. By inhibiting these factors, anticoagulants slow down or disrupt the clotting cascade, a series of chemical reactions that lead to clot formation.
- Preventing Platelet Aggregation: Some anticoagulants, such as heparin, work by preventing platelets from sticking together. Platelets are small cell fragments in the blood that play a crucial role in clot formation. By inhibiting platelet aggregation, anticoagulants reduce the likelihood of clot formation.
- Inhibiting Thrombin: Thrombin is a central enzyme in the clotting cascade that converts fibrinogen (a soluble protein) into fibrin (insoluble strands), forming the structural framework of a blood clot. Anticoagulants like heparin and direct thrombin inhibitors (e.g., dabigatran) directly interfere with thrombin’s activity.
- Vitamin K Inhibition: Warfarin (Coumadin), a commonly used anticoagulant, interferes with the production of vitamin K-dependent clotting factors (Factors II, VII, IX, and X) in the liver. Vitamin K is necessary for the activation of these clotting factors. By reducing their production, warfarin indirectly prolongs the time it takes for blood to clot.
- Direct Oral Anticoagulants (DOACs): DOACs, such as rivaroxaban, apixaban, and edoxaban, target specific clotting factors in the blood, such as Factor Xa or thrombin, directly inhibiting their activity. These medications are more selective and have a more predictable response compared to warfarin.
- Antiplatelet Agents: While not classified as anticoagulants, drugs like aspirin and clopidogrel are often used to prevent platelet activation and aggregation, reducing the risk of clot formation. They work primarily by inhibiting platelet function rather than targeting clotting factors.
Types of Anticoagulants used in Laboratory:
Anticoagulants are substances used in laboratories to prevent blood from clotting, allowing for various diagnostic tests and analyses. Some common types of anticoagulants used in laboratory settings include:
- Heparin: Heparin is a naturally occurring anticoagulant that works by inhibiting blood clotting factors. It is often used for tests like activated partial thromboplastin time (APTT) and is available in unfractionated and low molecular weight forms.
- EDTA (Ethylenediaminetetraacetic acid): EDTA is a chelating agent that binds to calcium ions, preventing them from participating in the coagulation cascade. It is commonly used in hematology for complete blood counts (CBC) and other blood cell-related tests.
- Sodium Citrate: Sodium citrate is an anticoagulant that works by binding calcium ions. It is often used for coagulation studies, such as prothrombin time (PT) and activated partial thromboplastin time (APTT).
- Sodium Heparin: Sodium heparin is a variant of heparin that is used for specialized tests, including antithrombin assays.
- Oxalates: Potassium oxalate and sodium oxalate are anticoagulants used for certain chemistry tests, particularly those involving glucose measurements.
- Citrate-Phosphate-Dextrose (CPD): CPD is used for preserving whole blood for blood transfusion purposes.
- ACD (Acid-Citrate-Dextrose): ACD is another anticoagulant used for blood collection in blood banks.
Types of Anticoagulants:
Here are some of the main types of anticoagulants:
Heparin:
- Heparin is one of the oldest and most commonly used anticoagulants.
- It acts rapidly and is often used in hospital settings, such as during surgeries or when a patient is at risk of developing blood clots.
- Heparin is typically administered through intravenous (IV) injections or subcutaneous injections.
Warfarin (Coumadin):
- Warfarin is an oral anticoagulant that has been in use for decades.
- It works by inhibiting the production of vitamin K-dependent clotting factors (Factors II, VII, IX, and X) in the liver.
- Warfarin requires careful monitoring of the International Normalized Ratio (INR) to ensure that it is within the therapeutic range.
Direct Oral Anticoagulants (DOACs):
- DOACs are a newer class of oral anticoagulants that have gained popularity due to their effectiveness and ease of use.
- Examples of DOACs include dabigatran (Pradaxa), rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa).
- DOACs directly target specific clotting factors in the blood, such as Factor Xa or thrombin.
- They have a more predictable response compared to warfarin and do not require routine INR monitoring.
Antiplatelet Drugs:
- While not traditional anticoagulants, antiplatelet drugs are often used to prevent clot formation by inhibiting platelet function.
- Common antiplatelet drugs include aspirin and clopidogrel (Plavix).
- They are used to reduce the risk of blood clots in conditions like coronary artery disease, stroke, and peripheral artery disease.
Low Molecular Weight Heparins (LMWH):
- LMWHs, such as enoxaparin (Lovenox) and dalteparin (Fragmin), are derived from heparin but have different properties.
- They are administered by subcutaneous injection.
- LMWHs have a longer duration of action compared to regular heparin.
Fondaparinux (Arixtra):
- Fondaparinux is a synthetic anticoagulant that specifically inhibits Factor Xa in the clotting cascade.
- It is administered by subcutaneous injection.
Other Novel Anticoagulants:
- Ongoing research has led to the development of new anticoagulants with different mechanisms of action, such as betrixaban (Bevyxxa) and darexaban. These may have specific indications or advantages in certain clinical situations.
Indications for Anticoagulant Use:
Here are some common indications for anticoagulant therapy.
- Atrial Fibrillation (AFib): Atrial fibrillation is an irregular heart rhythm that can lead to the formation of blood clots in the atria (upper chambers of the heart). These clots can then travel to other parts of the body and cause strokes or other complications. Anticoagulants are often prescribed to reduce the risk of stroke in individuals with AFib.
- Venous Thromboembolism (VTE): VTE includes conditions such as deep vein thrombosis (DVT) and pulmonary embolism (PE), where blood clots form in the veins, usually in the legs, and can break free, traveling to the lungs or other organs. Anticoagulants are used to treat and prevent VTE.
Mechanical Heart Valves: People with mechanical heart valves are at increased risk of blood clots forming on the valve itself. Anticoagulants are often prescribed to prevent these clots and reduce the risk of valve-related complications.- Post-Surgical Prophylaxis: After certain surgeries, especially those involving the hips, knees, or major orthopedic procedures, there is an increased risk of DVT and PE. Anticoagulants may be prescribed for a short period to prevent these complications.
- Stroke Prevention in High-Risk Patients: Patients with certain risk factors for stroke, such as a history of stroke or transient ischemic attack (TIA), heart disease, or other vascular conditions, may be prescribed anticoagulants to reduce the risk of future strokes.
- Cancer-Associated Thrombosis: Some cancers and cancer treatments can increase the risk of blood clots. Anticoagulants are used to manage and prevent clotting complications in cancer patients.
- Antiphospholipid Syndrome (APS): APS is an autoimmune disorder that can lead to excessive clotting. Anticoagulants are often prescribed to prevent recurrent thrombotic events in individuals with APS.
- Left Ventricular Thrombus: In cases where blood clots form in the left ventricle of the heart (typically due to conditions like dilated cardiomyopathy or aneurysms), anticoagulants may be used to prevent embolization of the clot.
- High-Risk Pregnancies: Pregnant women with certain medical conditions or a history of pregnancy-related clotting disorders may be prescribed anticoagulants to reduce the risk of pregnancy-related complications like preeclampsia and fetal growth restriction.
- Chronic Anticoagulation: Some individuals with recurrent blood clotting disorders or chronic conditions that increase their clotting risk may require long-term or lifelong anticoagulant therapy.
Prescribing and Monitoring:
Here are key considerations in prescribing and monitoring anticoagulants:
Prescribing Anticoagulants:
- Medical Assessment: The decision to prescribe anticoagulants should be based on a thorough medical assessment, including the patient’s medical history, current medical conditions, risk factors for clotting, and potential contraindications.
- Choice of Anticoagulant: Select the appropriate type of anticoagulant based on the patient’s condition, age, comorbidities, and other individual factors. Consider factors like oral versus injectable anticoagulants, patient preferences, and drug interactions.
- Dosing: Prescribe the correct dose of the anticoagulant, taking into account the patient’s weight, renal function, and any other specific dosing guidelines for the chosen medication.
- Duration of Therapy: Determine whether the patient needs short-term or long-term anticoagulation. For example, post-surgical prophylaxis may be short-term, while conditions like atrial fibrillation may require lifelong anticoagulation.
- Patient Education: Ensure that the patient understands the importance of adherence to the prescribed regimen, including dosing instructions, potential side effects, and the significance of regular monitoring.
Monitoring Anticoagulant Therapy:
- Regular Blood Tests: Depending on the type of anticoagulant, patients may require regular blood tests to monitor the effectiveness of therapy and assess the risk of bleeding. Common tests include the International Normalized Ratio (INR) for warfarin or drug-specific tests for direct oral anticoagulants (DOACs).
- Individualized INR Range: For patients on warfarin, establish an individualized target INR range based on their specific condition and risk factors. Adjust the dose as needed to maintain INR within this range.
- Assessing Bleeding Risk: Continuously evaluate the patient’s risk of bleeding, taking into account factors such as age, comorbidities, concomitant medications, and recent surgical procedures.
- Patient Compliance: Regularly assess the patient’s adherence to the prescribed anticoagulant regimen. Non-compliance can lead to treatment failure or increased bleeding risk.
- Drug Interactions: Be vigilant for potential drug interactions that can affect anticoagulant effectiveness or safety. Adjust medications or doses as necessary to mitigate interactions.
- Monitoring for Side Effects: Watch for signs of adverse effects, such as bleeding, allergic reactions, or other drug-related complications. Educate patients on recognizing and reporting these symptoms promptly.
- Patient Education: Provide ongoing education to patients about the importance of monitoring, recognizing signs of bleeding or clotting, and maintaining a balanced and healthy lifestyle.
- Regular Follow-Up: Schedule regular follow-up appointments to assess the patient’s response to treatment, make dose adjustments if necessary, and address any concerns or questions the patient may have.
- Communication: Maintain open communication with the patient and other healthcare providers involved in the patient’s care to ensure that anticoagulant therapy is effectively managed within the broader healthcare context.
Potential Side Effects and Complications:
Here are some of the common side effects and complications associated with anticoagulant therapy.
- Bleeding: The most significant risk of anticoagulant therapy is bleeding. This can manifest as.
- Minor Bleeding: Such as nosebleeds, gum bleeding, or easy bruising.
- Major Bleeding: More serious bleeding events, including gastrointestinal bleeding, intracranial hemorrhage (bleeding in the brain), or bleeding in other vital organs.
- Heparin-Induced Thrombocytopenia (HIT): Some patients receiving heparin can develop an immune reaction that leads to a decrease in platelet count, potentially causing clotting complications. HIT is more commonly associated with unfractionated heparin than low molecular weight heparins.
- Osteoporosis: Long-term use of heparin or warfarin can lead to decreased bone density and an increased risk of osteoporosis, which can result in fractures.
- Skin Necrosis: Warfarin, in rare cases, can cause skin necrosis (death of skin tissue) due to a paradoxical increase in clotting in small blood vessels. This typically occurs shortly after initiating therapy.
- Allergic Reactions: While uncommon, some individuals may experience allergic reactions to anticoagulants, which can include skin rashes, itching, or more severe allergic responses.
- Gastrointestinal Symptoms: Anticoagulants like warfarin can sometimes cause gastrointestinal discomfort, including nausea and diarrhea.
- Drug Interactions: Anticoagulants can interact with other medications, potentially affecting their effectiveness or increasing the risk of bleeding. Patients should inform their healthcare providers about all medications and supplements they are taking.
- Over-anticoagulation: Occasionally, patients may experience over-anticoagulation, leading to excessive bleeding. This can happen due to factors like incorrect dosing, drug interactions, or individual variations in drug metabolism.
- Thrombosis or Clotting Events: Paradoxically, anticoagulant therapy may not prevent all clotting events, and in some cases, it can lead to an increased risk of certain types of clot formation, such as venous limb gangrene in HIT patients or thrombosis in those with underlying prothrombotic conditions.
- Dietary Interactions: Patients on warfarin need to be cautious about their diet because vitamin K-rich foods can interfere with the drug’s effectiveness. Maintaining a consistent intake of vitamin K-containing foods is essential for warfarin therapy.
- Pregnancy Concerns: Anticoagulants pose risks and benefits during pregnancy. They can reduce the risk of blood clots but may also carry risks to the developing fetus. Pregnant women on anticoagulants should receive specialized care and monitoring.
- Reduced Effectiveness with Age: In older adults, particularly those with age-related kidney function decline, the effectiveness of anticoagulants like DOACs may be reduced, necessitating careful dosing adjustments.
Patient Education:
Here are key points to include in patient education when it comes to anticoagulant therapy:
- Understanding the Condition: Explain the medical condition that requires anticoagulant therapy, such as atrial fibrillation, deep vein thrombosis, or a mechanical heart valve. Provide information about the risk of blood clots and the consequences of untreated clots.
- Medication Overview: Discuss the specific anticoagulant medication prescribed, including its name, purpose, and how it works to prevent blood clots.
- Dosing Instructions: Explain the prescribed dosage, including when and how to take the medication. Emphasize the importance of taking it as directed.
- Monitoring: Inform the patient about the need for regular monitoring, such as blood tests (e.g., INR for warfarin), and the significance of staying within the target therapeutic range.
- Side Effects and Complications: Educate the patient about potential side effects and complications of anticoagulant therapy, particularly bleeding. Describe when to seek medical attention for bleeding or unusual symptoms.
- Dietary Considerations: If the patient is on warfarin, discuss dietary considerations related to vitamin K-rich foods and the importance of maintaining a consistent diet.
- Medication Interactions: Advise patients to inform all healthcare providers about their anticoagulant therapy, as other medications or supplements can interact with anticoagulants.
- Lifestyle Modifications: Encourage patients to make lifestyle changes to reduce clotting risk, such as regular exercise, smoking cessation, and maintaining a healthy weight.
- Alcohol and Drug Use: Caution against excessive alcohol consumption and the use of recreational drugs, as these can increase the risk of bleeding.
- Pregnancy and Contraception: Discuss pregnancy considerations, as anticoagulants can have implications for pregnancy. Ensure that women of childbearing age have a plan for contraception and pregnancy management if necessary.
- Travel Precautions: Provide guidance on travel, particularly for long flights or trips that may increase the risk of clot formation. Encourage frequent movement and hydration during travel.
- Medication Management: Stress the importance of taking medications consistently and on time. Discuss strategies to help patients remember to take their anticoagulant medication.
- Emergency Preparedness: Teach patients how to respond in case of an emergency, such as severe bleeding or injury. Provide instructions on when to call 911 or seek immediate medical attention.
- Regular Follow-Up: Emphasize the importance of attending all follow-up appointments with healthcare providers to assess treatment effectiveness and make any necessary adjustments.
- Patient Support Resources: Provide information about support groups, educational materials, and resources that can help patients manage their condition and medication.
- Questions and Concerns: Encourage patients to ask questions and voice any concerns they may have about their treatment. Ensure they have access to a healthcare provider for clarifications.
- Written Information: Provide written instructions and educational materials that patients can refer to at home. This can serve as a helpful reference.
Alternatives to Anticoagulants:
Here are some alternatives to anticoagulants.
- Antiplatelet Therapy: Antiplatelet drugs, such as aspirin and clopidogrel (Plavix), work by inhibiting platelet function and reducing the risk of platelet aggregation, which can lead to clot formation. They are commonly used in conditions like coronary artery disease and stroke prevention.
- Mechanical Intervention: In some cases, mechanical interventions may be an option. For example, patients with atrial fibrillation or certain types of heart valve problems may benefit from implantable devices like left atrial appendage closure devices, which reduce the risk of stroke without the need for long-term anticoagulation.
- Compression Stockings: Compression stockings or garments can help prevent blood clots in the legs, such as deep vein thrombosis (DVT). They work by applying pressure to the legs to improve blood flow.
- Inferior Vena Cava (IVC) Filters: IVC filters are devices inserted into the large vein in the abdomen to trap blood clots before they can travel to the lungs (pulmonary embolism). They are typically used when anticoagulation is contraindicated or has failed.
- Thrombolytic Therapy: Thrombolytic therapy involves the administration of drugs that can dissolve blood clots rapidly. This approach is used in emergencies, such as massive pulmonary embolism or acute ischemic stroke.
- Surgical Interventions: In certain cases, surgery may be necessary to remove blood clots or to address underlying anatomical issues that contribute to clot formation. Surgical options vary depending on the condition and location of the clot.
- Diet and Lifestyle Modifications: Patients at risk of blood clots can make lifestyle changes to reduce their risk. This includes maintaining a healthy weight, staying physically active, quitting smoking, and reducing alcohol consumption.
- Anti-Inflammatory Medications: In some conditions, such as antiphospholipid syndrome (APS), immunosuppressive or anti-inflammatory medications may be used to reduce the risk of clot formation.
- Novel Therapies and Clinical Trials: Ongoing research and clinical trials may lead to the development of new therapies and treatment options for conditions that traditionally require anticoagulants. Patients may have the opportunity to participate in clinical trials if they meet specific criteria.
FAQs:
What are anticoagulants?
Anticoagulants are medications that prevent or reduce the formation of blood clots. They are also known as blood thinners, although they do not actually “thin” the blood but rather interfere with the clotting process.
Why are anticoagulants prescribed?
Anticoagulants are prescribed to reduce the risk of blood clot formation, which can lead to conditions such as strokes, heart attacks, deep vein thrombosis (DVT), pulmonary embolism (PE), and more. They are also used to prevent clots in certain medical procedures and conditions.
What are the common types of anticoagulants?
Common anticoagulants include heparin, warfarin (Coumadin), direct oral anticoagulants (DOACs), and antiplatelet drugs like aspirin and clopidogrel.
How do anticoagulants work?
Anticoagulants work by inhibiting specific clotting factors in the blood, preventing platelet aggregation, or interfering with the clotting cascade. Their mechanisms of action vary depending on the type of anticoagulant.
Are anticoagulants safe?
Anticoagulants can be safe and effective when used under the guidance of a healthcare provider. However, they carry a risk of bleeding, so their use must be carefully monitored and managed.
What are the potential side effects of anticoagulants?
The most significant side effect is bleeding, which can range from minor bruising to major hemorrhage. Other potential side effects include skin necrosis, allergic reactions, and interactions with other medications.
How is anticoagulant therapy monitored?
Monitoring varies by the type of anticoagulant. For example, warfarin requires regular INR tests, while DOACs may have specific drug level tests. Monitoring helps ensure the medication is effective and the patient is within the therapeutic range.
Can I continue my normal activities while taking anticoagulants?
In most cases, yes, but you should be cautious about activities that could increase the risk of injury or bleeding. Consult with your healthcare provider about any specific restrictions or precautions.
Can I drink alcohol while taking anticoagulants?
Moderate alcohol consumption is generally safe, but excessive alcohol intake can increase the risk of bleeding. Consult with your healthcare provider for personalized guidance.
Are there dietary restrictions with anticoagulants?
Patients on warfarin need to be cautious about vitamin K-rich foods, as they can affect the medication’s effectiveness. Maintaining a consistent diet is important. Consult with your healthcare provider or a dietitian for guidance.
Can I stop taking anticoagulants on my own?
No, you should never stop or adjust your anticoagulant medication without consulting your healthcare provider. Abruptly discontinuing anticoagulants can be dangerous.
Conclusion:
In conclusion, anticoagulants are essential medications for preventing and treating potentially life-threatening blood clots, but their administration demands a comprehensive approach encompassing accurate diagnosis, personalized dosing, diligent monitoring, and patient education. Striking the delicate balance between mitigating clotting risks and minimizing bleeding complications remains paramount, making collaboration between healthcare providers and informed, engaged patients pivotal in achieving successful anticoagulant therapy outcomes.
Possible References Used







2 Comments