Columbia Agar, also known as Columbia Blood Agar, is a type of agar medium used in microbiology for the cultivation and isolation of bacteria, particularly those that are fastidious or difficult to grow on standard nutrient agar. It was developed at Columbia University in New York and is named after the institution.
- Medium Name: Columbia Agar, also known as Columbia Blood Agar.
- Development: Developed at Columbia University in New York, hence the name.
- Composition: It contains ingredients like peptones, beef heart infusion, yeast extract, and, often, sheep or horse blood.
- Enriched Medium: Columbia Agar is an enriched agar medium, providing essential nutrients for bacterial growth.
- Selective Properties: It is selective for fastidious bacteria, particularly those that require hemin and NAD for growth.
- Hemolysis Patterns: Can be used as a differential medium to distinguish between different Streptococcus species based on their hemolysis patterns (alpha, beta, gamma).
- Clinical Use: Commonly used in clinical microbiology labs to isolate and identify pathogens from various clinical samples.
- Anaerobic Growth: With appropriate supplements and anaerobic conditions, it can support the growth of anaerobic bacteria.
- Nutrient Agar Alternative: Sometimes used instead of standard nutrient agar when more enriched growth conditions are needed.
- Blood Agar: Often contains blood, typically sheep or horse blood, which provides growth factors and hemin.
- Fastidious Bacteria: Ideal for cultivating fastidious bacteria like Streptococcus pneumoniae and Haemophilus influenzae.
- Hemin and NAD: These are cofactors found in blood that are essential for the growth of certain bacteria.
- Identification: Helps in the isolation and identification of specific bacterial species.
- Beta-Hemolysis: Some bacteria, like Streptococcus pyogenes, exhibit beta-hemolysis, where they completely lyse red blood cells on the agar, creating a clear zone.
- Alpha-Hemolysis: Others, like Streptococcus pneumoniae, show alpha-hemolysis, causing partial hemolysis and a greenish coloration.
- Gamma-Hemolysis: Some bacteria, like Enterococcus, do not cause hemolysis and produce no change in the medium (gamma-hemolysis).
- Microbiological Culture: Part of the microbiologist’s toolkit for culturing and identifying bacteria.
- Custom Formulations: Specific formulations of Columbia Agar may vary depending on the laboratory’s needs and the targeted bacteria.
Defination of Columbia Agar:
Columbia Agar, also known as Columbia Blood Agar, is an enriched microbiological growth medium containing nutrients, typically peptones, beef heart infusion, yeast extract, and blood (usually sheep or horse), used to cultivate and selectively grow fastidious bacteria, especially those requiring hemin and NAD for growth. It is commonly employed in clinical microbiology for isolating and identifying pathogens from clinical samples.
History and Modifications of Columbia Agar:
- Development at Columbia University: Columbia Agar was originally developed at Columbia University in New York for microbiological use.
- Initial Formulation: The original formulation included ingredients like peptones, beef heart infusion, yeast extract, and blood (usually sheep or horse) to support bacterial growth.
- Enriched Growth Medium: Columbia Agar is an enriched growth medium with nutrients and blood, making it suitable for cultivating fastidious bacteria.
- Selective Properties: It selectively supports the growth of bacteria that require hemin and NAD for growth, facilitating the isolation of specific pathogens.
- Clinical Microbiology: Columbia Agar is extensively used in clinical microbiology laboratories for isolating and identifying bacterial pathogens from clinical samples.
- Anaerobic Growth Variations: Modified versions of Columbia Agar exist to facilitate the growth of anaerobic bacteria when supplemented with appropriate reducing agents and under anaerobic conditions.
- Custom Formulations: Laboratories can create customized formulations of Columbia Agar to meet specific growth requirements or target particular bacterial species.
Purpose and Significance of Columbia Agar:
- Enriched Bacterial Growth: Columbia Agar serves as an enriched medium that provides essential nutrients and blood, promoting the growth of various bacteria.
- Support for Fastidious Bacteria: It is particularly valuable for cultivating fastidious bacteria that have specific growth requirements, including the need for hemin and NAD.
- Selective Medium: Columbia Agar selectively supports the growth of bacteria with specific nutritional needs, making it useful for isolating and identifying pathogens.
- Clinical Microbiology: Widely used in clinical microbiology labs, it aids in the isolation and identification of bacterial pathogens from clinical samples.
- Differential Properties: Columbia Agar can differentiate between bacterial species based on their hemolysis patterns (alpha, beta, gamma), assisting in identification.
- Anaerobic Growth Support: Modified versions enable the cultivation of anaerobic bacteria when combined with appropriate supplements and anaerobic conditions.
- Customization: Laboratories can tailor Columbia Agar formulations to suit specific bacterial growth requirements or research objectives.
Importance of Columbia Agar in Microbiology:
- Selective Growth: It selectively supports the growth of fastidious bacteria, making it crucial for isolating specific pathogens.
- Enriched Nutrients: Provides essential nutrients and blood, facilitating the luxuriant growth of a wide range of bacteria.
- Clinical Diagnosis: Widely used in clinical microbiology labs for isolating and identifying bacterial pathogens from clinical samples.
- Hemolysis Patterns: Helps differentiate between bacterial species based on their hemolysis patterns, aiding in identification.
- Anaerobic Growth: Modified versions enable the cultivation of anaerobic bacteria, expanding its utility in diverse microbiological studies.
- Customization: Laboratories can customize Columbia Agar formulations to suit specific research needs and targeted bacteria.
Principles of Columbia Agar:
- Enriched Growth Medium: Provides essential nutrients, including peptones, yeast extract, and blood, to support bacterial growth.
- Selective Properties: Selectively promotes the growth of fastidious bacteria with specific growth requirements, such as hemin and NAD.
- Differential Medium: Differentiates between bacterial species based on their hemolysis patterns (alpha, beta, gamma).
- Clinical Utility: Widely used in clinical microbiology to isolate and identify bacterial pathogens in clinical samples.
- Anaerobic Compatibility: Can be modified to support the growth of anaerobic bacteria when supplemented and incubated in anaerobic conditions.
- Enhanced Growth: Colonies on Columbia Agar tend to be larger and exhibit more luxuriant growth compared to other blood agar bases.
Clinical Applications of Columbia Agar:
- Isolation of Pathogens: Columbia Agar is commonly used in clinical microbiology laboratories for the isolation and cultivation of pathogenic bacteria from various clinical specimens, such as throat swabs, sputum, wound exudates, and blood cultures.
- Identification of Fastidious Bacteria: It is especially useful for the cultivation and identification of fastidious bacteria, which have specific nutritional requirements and may not grow well on standard agar media. Fastidious bacteria often include important human pathogens.
- Hemolysis Pattern Differentiation: Columbia Agar can be employed to differentiate between bacterial species based on their hemolysis patterns, such as alpha-hemolysis, beta-hemolysis, or gamma-hemolysis. This differentiation assists in the identification of pathogenic bacteria, such as Streptococcus species.
- Clinical Diagnosis: Clinical microbiologists use Columbia Agar to identify and confirm the presence of pathogenic bacteria in patient samples. This information is crucial for diagnosing infectious diseases and guiding appropriate treatment strategies.
- Antibiotic Susceptibility Testing: Bacterial isolates grown on Columbia Agar can be subjected to antibiotic susceptibility testing to determine the most effective antibiotics for treating infections caused by these bacteria. This aids in selecting the appropriate antibiotic therapy for patients.
- Research and Surveillance: In addition to its diagnostic role, Columbia Agar is used in research and epidemiological surveillance to study the prevalence and characteristics of specific bacterial strains, including antibiotic resistance patterns.
Ingredients, Materials and composition of Columbia Agar:
The composition of Columbia Agar can vary slightly depending on specific formulations used in different laboratories or commercial products. However, I can provide a general overview of the typical ingredients, materials, and composition of Columbia Agar:
Ingredients:
- Peptones: These are enzymatic digests of proteins and serve as a source of amino acids, nitrogen, and essential growth factors for bacteria.
- Beef Heart Infusion: Provides additional nutrients and growth factors.
- Yeast Extract: Acts as a source of B vitamins and other growth-promoting substances.
- Corn Starch: Serves as an energy source for bacterial growth and may also neutralize toxic metabolites by absorbing them.
- Sodium Chloride: Provides essential electrolytes and helps maintain osmotic equilibrium.
- Sheep or Horse Blood: Often used to demonstrate hemolytic reactions and supply heme (X factor), which is necessary for the growth of many pathogenic bacteria.
- Agar: A solidifying agent that gives the medium its gel-like consistency.
- Distilled Water: Used to dissolve and mix the ingredients.
Materials:
- Laboratory Glassware: Erlenmeyer flasks, beakers, or containers for mixing and autoclaving the medium.
- Bunsen Burner: Used for sterilization of equipment and to create aseptic conditions.
- Autoclave: Used to sterilize the medium after preparation.
Composition of Columbia Agar:
The exact composition of Columbia Agar can vary slightly between different formulations and manufacturers. However, I can provide a general overview of the typical ingredients, their quantities, and their purposes in Columbia Agar:
| Ingredient | Quantity per Liter of Medium | Purpose |
|---|---|---|
| Peptones | 10-15 grams | Provide amino acids, nitrogen, and growth factors for bacteria. |
| Beef Heart Infusion | 2-5 grams | Supplies additional nutrients and growth-promoting substances. |
| Yeast Extract | 1.5-2.5 grams | Acts as a source of B vitamins and other growth-promoting factors. |
| Corn Starch | 1-2 grams | Serves as an energy source for bacterial growth and may neutralize toxic metabolites. |
| Sodium Chloride | 5-10 grams | Provides essential electrolytes and helps maintain osmotic equilibrium. |
| Sheep or Horse Blood | Typically 5-10% of the total volume | Demonstrates hemolytic reactions and supplies heme (X factor) for the growth of many pathogens. |
| Agar | 13-15 grams | Solidifying agent that gives the medium its gel-like consistency. |
| Distilled Water | To make up the total volume | Used to dissolve and mix the ingredients. |
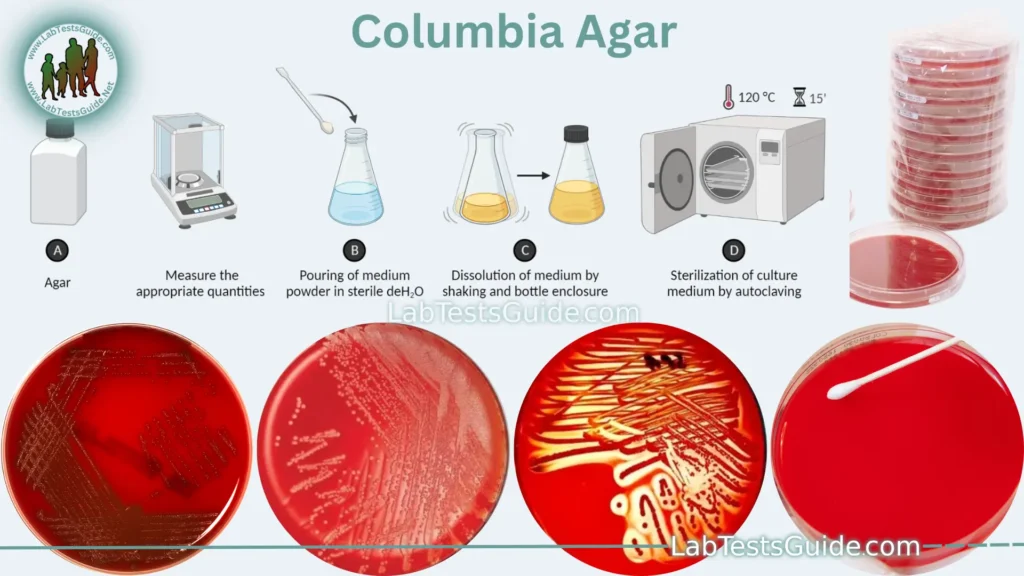
Preparation of Columbia Agar:
- Gather Ingredients and Materials:
- Collect all the required ingredients, including peptones, beef heart infusion, yeast extract, corn starch, sodium chloride, sheep or horse blood, agar, and distilled water.
- Ensure you have the necessary laboratory glassware and equipment, such as Erlenmeyer flasks, a Bunsen burner, an autoclave, and containers for pouring and storing the agar.
- Weigh and Mix Ingredients:
- Weigh the appropriate quantities of each ingredient according to the formulation you are following.
- Mix the dry ingredients (peptones, beef heart infusion, yeast extract, corn starch, sodium chloride, and agar) together in a clean container.
- Prepare Blood Component:
- If using sheep or horse blood, collect and anticoagulate the blood.
- Aseptically add the desired volume of blood to the mixture. Blood percentage can vary but is typically 5-10% of the total volume.
- Dissolve Ingredients in Water:
- In a separate container, add distilled water.
- Gradually add the dry mixture while stirring continuously to ensure even dispersion.
- Heat and Sterilize:
- Heat the mixture while stirring until it dissolves completely.
- Sterilize the medium by autoclaving it at the appropriate conditions (typically 121°C for 15 minutes).
- Pour and Solidify:
- Aseptically pour the sterilized medium into sterile petri dishes or containers to solidify.
- Allow the agar to cool and solidify in a sterile environment, either at room temperature or in a controlled incubator.
- Storage:
- Seal the containers with the solidified agar and store them in a cool, dry place until needed.
Required Specimins for Culturing on Columbia Agar:
- Sputum: Sputum samples are commonly cultured on Columbia Agar to detect and identify respiratory pathogens, including Streptococcus pneumoniae and Haemophilus influenzae.
- Throat Swabs: Throat swabs are cultured to identify bacteria causing pharyngitis or tonsillitis, such as Streptococcus pyogenes (Group A Streptococcus).
- Blood Cultures: Columbia Agar can be used for subculturing positive blood cultures to identify the causative agents of bloodstream infections.
- Wound Exudates: Specimens from wounds or abscesses can be cultured on Columbia Agar to isolate and identify wound pathogens, including Staphylococcus aureus and Streptococcus species.
- Cerebrospinal Fluid (CSF): CSF samples are cultured on Columbia Agar to detect and identify bacteria causing meningitis, such as Neisseria meningitidis or Streptococcus pneumoniae.
- Urinary Tract Specimens: Urine samples may be cultured on Columbia Agar to identify bacteria responsible for urinary tract infections (UTIs), including Escherichia coli.
- Stool Samples: Columbia Agar can be used to culture stool specimens to isolate enteric pathogens, such as Salmonella and Shigella species.
- Respiratory Specimens: Besides sputum, other respiratory specimens like bronchoalveolar lavage (BAL) fluid and bronchial washings may be cultured on Columbia Agar to identify respiratory pathogens.
- Genital Swabs: Specimens from the genital tract, such as vaginal swabs or urethral swabs, can be cultured to identify sexually transmitted infections (STIs).
- Tissue Biopsies: Tissue biopsies may be cultured on Columbia Agar in cases of suspected deep-seated infections or abscesses.
- Environmental Samples: In research settings, environmental samples may be cultured on Columbia Agar to study the presence and characteristics of bacteria in various settings.
Usage Procedure of Columbia Agar:
- Prepare the Medium: Prepare Columbia Agar according to the manufacturer’s instructions or laboratory protocols. Sterilize it by autoclaving.
- Prepare Specimens: Collect clinical specimens (e.g., sputum, throat swabs, blood cultures, wound exudates) aseptically following proper collection techniques.
- Inoculation: Using a sterile loop or swab, transfer a small amount of the specimen onto the surface of the Columbia Agar medium.
- Streaking or Swabbing: For quantitative cultures, streak the specimen onto the surface using a calibrated loop. For qualitative cultures, gently swab the specimen across the agar surface.
- Incubation: Incubate the inoculated Columbia Agar plates in a controlled environment (typically at 35-37°C) for an appropriate duration (e.g., 18-24 hours).
- Observation: Examine the plates for bacterial growth and colony morphology. Note any hemolysis patterns (alpha, beta, gamma) on blood agar variants.
- Identification: Based on colony characteristics, conduct further biochemical tests or use specific identification methods (e.g., Gram staining, biochemical assays) to identify the cultured bacteria.
- Antibiotic Susceptibility Testing: Perform antibiotic susceptibility testing on isolated bacteria if needed to determine the most effective antibiotic therapy.
- Data Recording: Record all relevant information, including specimen source, bacterial species identification, and antibiotic susceptibility results, in the laboratory records.
- Reporting: Prepare a laboratory report summarizing the findings and communicate the results to healthcare professionals or researchers as required.
- Sterilization: Properly dispose of used agar plates and contaminated materials. Sterilize any waste generated during the process.
- Quality Control: Implement quality control measures to ensure the accuracy and reliability of results, including regular testing of the medium and equipment.
Result Interpretation of Columbia Agar:
- Bacterial Growth:
- Look for the presence or absence of bacterial growth on the agar plates. Growth indicates the presence of viable bacteria in the specimen.
- Colony Morphology:
- Examine the characteristics of bacterial colonies, including size, shape, color, and texture. Note any variations in colony appearance.
- Hemolysis Patterns:
- On blood agar variants of Columbia Agar, observe hemolysis patterns around colonies:
- Alpha-hemolysis: Partial hemolysis, resulting in a greenish zone around colonies.
- Beta-hemolysis: Complete hemolysis, leading to a clear zone around colonies.
- Gamma-hemolysis: No hemolysis, with no change in the agar appearance around colonies.
- On blood agar variants of Columbia Agar, observe hemolysis patterns around colonies:
- Quantitative vs. Qualitative Culture:
- Consider whether the culture is quantitative (counting colony-forming units) or qualitative (identifying the presence or absence of specific bacteria).
- Bacterial Identification:
- Based on colony characteristics and, if necessary, conduct further tests for bacterial identification. This may include Gram staining, biochemical tests, or molecular techniques.
- Antibiotic Susceptibility Testing:
- If the purpose of the culture is to determine antibiotic susceptibility, assess the results of susceptibility testing to guide appropriate treatment decisions.
Growth of Bacterias and Colony Characteristics on Columbia Agar:
| Bacterium | Growth on Columbia Agar | Colony Characteristics |
|---|---|---|
| Staphylococcus aureus | Good | Round, convex, golden yellow colonies |
| Staphylococcus epidermidis | Good | Round, convex, white or light yellow colonies |
| Streptococcus pyogenes | Good | Beta-hemolytic colonies with a clear zone of hemolysis around them |
| Streptococcus pneumoniae | Good | Alpha-hemolytic colonies with a green zone of hemolysis around them |
| Enterococcus faecalis | Good | Round, convex, white or light gray colonies |
| Bacillus subtilis | Good | Large, flat, spreading colonies with a wavy edge |
| Escherichia coli | Poor or no growth | Not recommended for isolation of Gram-negative bacteria |
| Klebsiella pneumoniae | Poor or no growth | Not recommended for isolation of Gram-negative bacteria |
| Pseudomonas aeruginosa | Poor or no growth | Not recommended for isolation of Gram-negative bacteria |
Limitations of Columbia Agar:
- Selective Properties: While it supports the growth of many bacteria, it may not be suitable for all types of microorganisms, especially those with highly specialized growth requirements that differ from the nutrients provided by Columbia Agar.
- Complexity: The formulation of Columbia Agar is relatively complex compared to some other agar media, which can make it more time-consuming to prepare and may require careful quality control to ensure consistency.
- Anaerobic Growth: Columbia Agar is primarily designed for aerobic or facultative anaerobic bacteria. It may not support the growth of strict anaerobes without modifications and additional reducing agents.
- Hemolysis Patterns: While it can differentiate between hemolysis patterns (alpha, beta, gamma), this differentiation may not always be clear-cut, and interpretation can sometimes be subjective.
- Cost: Columbia Agar can be more expensive to prepare or purchase compared to simpler media, which can be a consideration for laboratories with budget constraints.
- Specialized Media: For some specific bacterial species or applications, other specialized media may be more suitable, and Columbia Agar may not provide the necessary selectivity or differential characteristics.
- Labor-Intensive: Columbia Agar may require more labor and expertise for interpretation, especially when identifying bacterial species based on colony characteristics or biochemical tests.
- Clinical Correlation: The presence of bacterial growth on Columbia Agar does not necessarily indicate pathogenicity. Clinical correlation with a patient’s symptoms and other diagnostic tests is essential for accurate diagnosis.
- Antibiotic Susceptibility: While Columbia Agar can be used for initial bacterial isolation, it may not be the primary medium used for antibiotic susceptibility testing, which is typically performed on more specialized media.
- Research Requirements: In research settings, where specific bacterial strains or conditions are needed, other media tailored to those requirements may be preferred over Columbia Agar.
Safety Considerations of Columbia Agar:
- Personal Protective Equipment (PPE): Always wear appropriate PPE, including lab coats, gloves, and safety goggles or face shields, when handling Columbia Agar and bacterial cultures.
- Aseptic Techniques: Practice strict aseptic techniques to minimize the risk of contamination when inoculating, streaking, or transferring specimens onto Columbia Agar plates.
- Biohazard Safety Cabinet (BSC): When working with potentially infectious or aerosol-generating materials, use a BSC to contain and protect against airborne particles. Follow BSC protocols for safe operation.
- Hand Hygiene: Wash hands thoroughly with soap and water before and after handling Columbia Agar and bacterial cultures. Use hand sanitizers when needed.
- Labeling and Documentation: Properly label all agar plates, containers, and specimens with relevant information, including the specimen source, date, and any potential biohazards.
- Disposal: Dispose of used Columbia Agar plates and contaminated materials in accordance with laboratory waste disposal protocols and local regulations. Autoclave waste before disposal if required.
- Incubation Conditions: Incubate agar plates at appropriate temperatures and conditions to promote bacterial growth while minimizing the risk of overgrowth or contamination.
- Antibiotic Resistance Testing: When performing antibiotic susceptibility testing on isolated bacteria, handle antibiotics with care and follow safety guidelines for working with antimicrobial agents.
- Emergency Procedures: Be familiar with laboratory emergency procedures, including spill cleanup, first aid, and response to potential exposures to infectious agents.
- Training and Education: Ensure that laboratory personnel are adequately trained in microbiological techniques and safety protocols. Keep up-to-date with safety training.
- Reporting and Communication: Report any accidents, spills, or potential exposures to laboratory supervisors and follow established reporting procedures.
- Access Control: Restrict access to the laboratory to authorized personnel only, and ensure that laboratory doors are locked when unattended.
- Safety Data Sheets (SDS): Maintain and make accessible Safety Data Sheets (SDS) for all chemicals and reagents used in the laboratory, including agar components.
- Risk Assessment: Conduct risk assessments for specific experiments or procedures involving Columbia Agar to identify potential hazards and implement appropriate safety measures.
Comparison of Columbia Agar with Other Microbiological Media:
| Property | Columbia Agar | Blood Agar | MacConkey Agar | Sabouraud Agar |
|---|---|---|---|---|
| Composition | Complex | Nutrient-rich | Selective | Selective |
| Purpose | General | General | Selective | Fungal Isolation |
| Selectivity | Moderate | Low | High (for Gram-negative) | High (for Fungi) |
| Blood Component | Yes (Sheep or Horse) | Yes (Sheep or Horse) | No | No |
| Hemolysis Differentiation | Yes (Alpha, Beta, Gamma) | Yes (Alpha, Beta, Gamma) | No | No |
| Growth Support | Wide range of bacteria | Wide range of bacteria | Limited (Gram-negative) | Fungi |
| Anaerobic Growth | Possible with modifications | Possible with modifications | Not suitable | Possible |
| Typical Incubation Temp | 35-37°C | 35-37°C | 35-37°C | 25-30°C |
| Common Applications | Bacterial culture, hemolysis detection | Bacterial culture, hemolysis detection | Enteric bacteria isolation | Fungal isolation |
| Limitations | May not support strict anaerobes | May not support strict anaerobes | Selective for Gram-negative | Selective for Fungi |
| Special Considerations | Additional supplements for anaerobes | Additional supplements for anaerobes | Inhibits Gram-positive bacteria | pH control for fungi |
| Common Use Cases | Clinical microbiology, bacterial identification | Clinical microbiology, bacterial identification | Enteric pathogen isolation | Mycology (fungi) |
FAQs:
1. What is Columbia Agar?
- Columbia Agar is a microbiological growth medium used to culture a wide range of bacterial species. It contains various nutrients and is often supplemented with blood to support the growth of bacteria.
2. What is the purpose of using Columbia Agar?
- Columbia Agar is used for the isolation, cultivation, and identification of bacteria from clinical specimens. It is especially valuable for culturing fastidious or nutritionally demanding bacterial species.
3. How is Columbia Agar different from other agar media?
- Columbia Agar is distinct in its formulation, including the use of peptones, beef heart infusion, yeast extract, and blood. It is known for its ability to support the growth of a wide range of bacteria, including those that may not grow well on other media.
4. What types of bacteria can be cultured on Columbia Agar?
- Columbia Agar can support the growth of both Gram-positive and Gram-negative bacteria. It is particularly suitable for fastidious bacteria, such as Streptococcus and Haemophilus species.
5. What are the different hemolysis patterns observed on Columbia Agar?
- Columbia Agar, especially when supplemented with blood, can exhibit three main hemolysis patterns: alpha-hemolysis (partial hemolysis), beta-hemolysis (complete hemolysis), and gamma-hemolysis (no hemolysis).
6. What is the significance of hemolysis patterns on Columbia Agar?
- Hemolysis patterns help differentiate between bacterial species and are important for identifying certain pathogens. For example, beta-hemolysis is often associated with pathogenic Streptococcus species.
7. How is Columbia Agar prepared in the laboratory?
- Columbia Agar is prepared by mixing its components, including peptones, beef heart infusion, yeast extract, corn starch, sodium chloride, agar, and blood, followed by autoclaving to sterilize the medium.
8. Are there any safety considerations when working with Columbia Agar?
- Yes, safety precautions should be taken when working with Columbia Agar and bacterial cultures. This includes wearing appropriate personal protective equipment, practicing aseptic techniques, and following laboratory safety protocols.
9. What are the limitations of Columbia Agar?
- Columbia Agar may not support the growth of all bacterial species, especially strict anaerobes. It is also not suitable for certain specialized applications or selective culture requirements.
10. What are the clinical applications of Columbia Agar?
- Columbia Agar is used in clinical microbiology laboratories for isolating and identifying bacterial pathogens from clinical specimens, aiding in the diagnosis of infectious diseases.
Conclusion:
In conclusion, Columbia Agar is a versatile microbiological growth medium with a rich nutrient composition used in clinical microbiology and research settings. It supports the growth of a wide range of bacterial species, including fastidious organisms, making it a valuable tool for isolating and identifying pathogens from clinical specimens. Its ability to differentiate hemolysis patterns and provide essential nutrients for bacterial growth enhances its utility in diagnostic microbiology.
While Columbia Agar offers numerous advantages, it also has limitations, such as the inability to support strict anaerobic growth and its selectivity for certain bacterial species. Understanding these limitations and considering specific laboratory requirements is essential when choosing agar media for microbiological applications.
Possible References Used