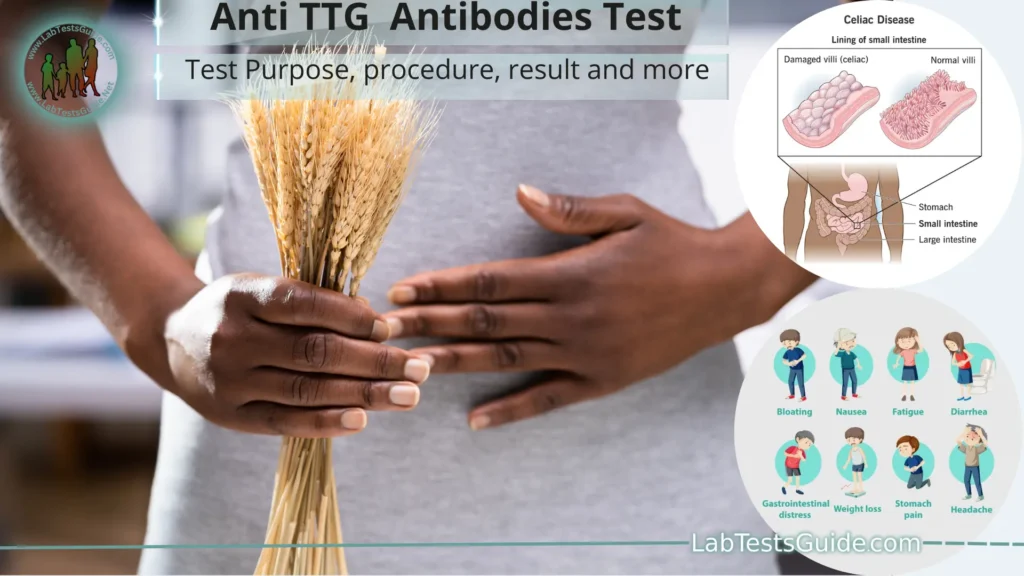
The Anti-tissue Transglutaminase (Anti TTG) antibody test is a blood test used to diagnose and monitor certain autoimmune diseases, particularly celiac disease. Celiac disease is an autoimmune disorder where the ingestion of gluten, a protein found in wheat, barley, and rye, triggers an immune response that damages the small intestine lining. Anti-TTG antibodies are produced by the immune system in response to the presence of gluten.
Defination of Anti TTG Antobodies:
The Anti TTG (Anti-tissue Transglutaminase) antibodies test is a medical laboratory test used to diagnose and monitor certain autoimmune disorders, with a primary focus on celiac disease.
Understanding Celiac Disease:
Celiac disease, also known as celiac sprue or gluten-sensitive enteropathy, is an autoimmune disorder that primarily affects the small intestine in genetically predisposed individuals. Here’s a comprehensive overview to help you understand this condition:
- Definition:
- Celiac disease is an autoimmune disorder characterized by an abnormal immune response to the consumption of gluten, a protein found in wheat, barley, and rye.
- Epidemiology:
- Celiac disease can affect individuals of all ages, races, and genders.
- It is estimated to affect around 1% of the global population, but many cases go undiagnosed.
- Pathophysiology:
- In individuals with celiac disease, the ingestion of gluten triggers an immune response.
- This immune response leads to inflammation and damage to the lining of the small intestine (intestinal villi), which impairs nutrient absorption.
- Symptoms:
- Celiac disease can manifest with a wide range of symptoms, including:
- Gastrointestinal symptoms: Diarrhea, abdominal pain, bloating, and constipation.
- Non-gastrointestinal symptoms: Fatigue, joint pain, skin rashes, and neurological issues.
- Some individuals may be asymptomatic, which is referred to as “silent” celiac disease.
- Celiac disease can manifest with a wide range of symptoms, including:
- Diagnosis:
- Diagnosis typically involves a combination of blood tests (such as the Anti-TTG Antibody Test) and a small intestine biopsy.
- Blood tests help identify celiac-specific antibodies in the bloodstream.
- Biopsy confirms the characteristic damage to the small intestinal villi.
- Treatment:
- The primary and only effective treatment for celiac disease is a lifelong gluten-free diet.
- Strict avoidance of gluten-containing foods is necessary to alleviate symptoms and prevent complications.
- Complications:
- Untreated celiac disease can lead to various complications, including malnutrition, anemia, osteoporosis, infertility, and an increased risk of certain cancers.
- Gluten Sensitivity vs. Celiac Disease:
- Celiac disease is an autoimmune disorder with specific diagnostic criteria.
- Gluten sensitivity, on the other hand, is a condition characterized by gastrointestinal symptoms in response to gluten ingestion without the autoimmune response seen in celiac disease.
- Management and Support:
- Managing celiac disease requires careful dietary planning and label reading to avoid hidden sources of gluten.
- Support groups and resources are available to help individuals cope with the challenges of living gluten-free.
- Research and Future Directions:
- Ongoing research is focused on improving diagnostic methods, understanding the genetic basis of celiac disease, and exploring potential treatments beyond a gluten-free diet.
Role of Anti-TTG Antibodies:
The role of Anti-TTG (Anti-tissue Transglutaminase) antibodies is crucial in the context of celiac disease diagnosis and understanding. These antibodies play several important roles:
- Diagnostic Marker:
- Anti-TTG antibodies are a key diagnostic marker for celiac disease. Elevated levels of Anti-TTG antibodies in the blood are often indicative of an autoimmune response to gluten consumption.
- They serve as a reliable indicator that an individual’s immune system is reacting to the presence of tissue transglutaminase in the small intestine.
- Autoimmune Response Indicator:
- The presence of Anti-TTG antibodies in the bloodstream indicates that the immune system is targeting and reacting against tissue transglutaminase, an enzyme found in the lining of the small intestine.
- This autoimmune response leads to the characteristic damage to the intestinal villi, which is a hallmark of celiac disease.
- Screening Tool:
- Anti-TTG antibody testing is often used as an initial screening tool for celiac disease, especially in individuals who exhibit symptoms like gastrointestinal discomfort, malabsorption issues, or unexplained weight loss.
- It helps healthcare providers identify individuals who may need further diagnostic evaluation.
- Monitoring Disease Activity:
- Anti-TTG antibody levels can also be used to monitor disease activity and treatment effectiveness in individuals with celiac disease.
- A decrease in Anti-TTG antibody levels over time can indicate that the gluten-free diet is working and that the autoimmune response is subsiding.
- Differentiating Celiac Disease from Other Conditions:
- While Anti-TTG antibodies are highly specific for celiac disease, their presence or absence can help differentiate celiac disease from other conditions, such as non-celiac gluten sensitivity.
- In non-celiac gluten sensitivity, Anti-TTG antibodies are typically not elevated.
- Clinical Decision-Making:
- Healthcare providers use Anti-TTG antibody test results, in combination with other diagnostic information like small intestine biopsy findings, to make clinical decisions regarding celiac disease diagnosis and management.
- Research and Understanding:
- Anti-TTG antibodies have been a subject of research in understanding the immunological mechanisms involved in celiac disease.
- Studying these antibodies helps researchers gain insights into the autoimmune responses that occur in celiac disease and may lead to potential therapeutic developments.
Significance in Celiac Disease Diagnosis:
The significance of Anti-TTG (Anti-tissue Transglutaminase) antibodies in celiac disease diagnosis is substantial. These antibodies play a central role in identifying and confirming the presence of celiac disease. Here’s why they are significant:
- High Sensitivity and Specificity:
- Anti-TTG antibodies have a high sensitivity and specificity for celiac disease. Sensitivity refers to the ability of the test to correctly identify individuals with the disease, while specificity refers to its ability to correctly identify individuals without the disease.
- In the case of Anti-TTG antibody testing, it is highly sensitive, meaning it is effective at identifying individuals with celiac disease, and it is highly specific, meaning it is unlikely to produce false-positive results in individuals without celiac disease.
- Early Detection:
- Anti-TTG antibody testing can detect celiac disease at an early stage, even before significant damage occurs to the small intestine.
- This early detection is crucial because it allows for the initiation of a gluten-free diet before severe complications develop.
- Non-Invasive:
- Unlike small intestine biopsy, which is another important diagnostic tool for celiac disease, Anti-TTG antibody testing is non-invasive.
- It involves a simple blood draw, making it less burdensome and more accessible for patients.
- Screening Tool:
- Anti-TTG antibody testing is often used as an initial screening tool for individuals suspected of having celiac disease.
- Positive results may prompt further diagnostic evaluation, including a small intestine biopsy, to confirm the diagnosis definitively.
- Monitoring Disease Activity:
- Anti-TTG antibody levels can be used to monitor disease activity and the effectiveness of treatment (typically a gluten-free diet) in individuals with celiac disease.
- A decrease in Anti-TTG antibody levels over time may indicate that the autoimmune response is subsiding due to dietary changes.
- Differentiation from Other Conditions:
- Celiac disease can sometimes mimic the symptoms of other gastrointestinal disorders. Anti-TTG antibody testing helps differentiate celiac disease from these other conditions.
- For example, non-celiac gluten sensitivity lacks the autoimmune response seen in celiac disease, and Anti-TTG antibody levels are typically not elevated in this condition.
- Clinical Decision-Making:
- Healthcare providers use the results of Anti-TTG antibody testing, in conjunction with clinical symptoms and other diagnostic tests, to make informed decisions regarding celiac disease diagnosis and management.
Sample and its Precautions:
Sample Collection:
- Sample for celiac disease diagnosis is typically a blood sample.
- The blood is drawn from a vein, usually in the arm.
Precautions:
- Fasting is not required; patients can eat before the test.
- Inform the healthcare provider of any medications or supplements being taken, as they might affect the results.
- For accurate results, ensure proper identification of the patient to prevent sample mix-up.
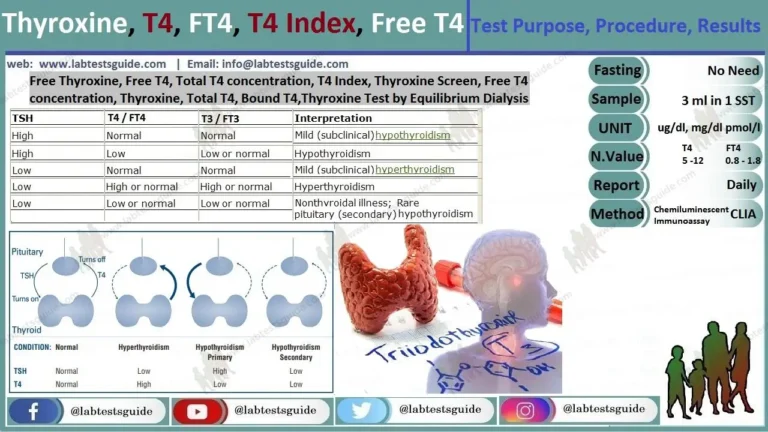
Anti TTG Test Types:
- Anti-TTG IgA Test:
- This test measures IgA (immunoglobulin A) antibodies against tissue transglutaminase.
- IgA antibodies are commonly used because they are found in the mucous membranes of the gastrointestinal tract, which is where celiac disease primarily affects.
- It is the primary form of the Anti-TTG antibody test and is considered highly specific for celiac disease diagnosis.
- Results are typically reported in units such as U/mL (units per milliliter) or IU/mL (international units per milliliter).
- Anti-TTG IgG Test:
- In some cases, individuals with celiac disease may have IgA deficiency, which can lead to false-negative results on the Anti-TTG IgA test.
- In such cases, the Anti-TTG IgG test is used to detect IgG antibodies against tissue transglutaminase.
- This test is often used as an alternative when IgA deficiency is suspected or confirmed.
- Results are also reported in units such as U/mL or IU/mL.
Normal Values:
The normal reference values for the Anti-TTG (Anti-tissue Transglutaminase) antibody tests can vary between laboratories and assay methods. Typically, results for these tests are reported in units such as U/mL (units per milliliter) or IU/mL (international units per milliliter). Here are approximate normal reference ranges for both the Anti-TTG IgA and IgG antibody tests:
Anti-TTG IgA Test:
- Normal Value: Typically less than 4 U/mL or IU/mL.
- A result below this threshold is often considered negative or normal, indicating a low likelihood of celiac disease.
Anti-TTG IgG Test:
- Normal Value: Typically less than 6 U/mL or IU/mL.
- Like the IgA test, a result below this threshold is generally considered negative or normal.
Result Interpretation:
Interpreting the results of medical tests, including those for celiac disease like the Anti-TTG (Anti-tissue Transglutaminase) antibody tests, requires careful consideration of various factors. Here’s how you can interpret these test results:
Anti-TTG IgA Test:
- Negative Result (Below the Reference Range):
- If your Anti-TTG IgA test result falls below the established reference range (typically less than 4 U/mL or IU/mL), it is usually considered negative or normal.
- A negative result suggests a low likelihood of celiac disease. However, it does not completely rule out the possibility, especially in cases of IgA deficiency.
- Positive Result (Above the Reference Range):
- If your Anti-TTG IgA test result is above the reference range, it is considered positive or elevated.
- An elevated result suggests an autoimmune response to tissue transglutaminase and is indicative of a higher likelihood of celiac disease.
- A positive result should be followed up with additional diagnostic steps, such as a small intestine biopsy, to confirm the diagnosis.
Anti-TTG IgG Test:
- Negative Result (Below the Reference Range):
- Similar to the IgA test, a negative result for the Anti-TTG IgG test (typically less than 6 U/mL or IU/mL) is considered normal and suggests a low likelihood of celiac disease.
- Positive Result (Above the Reference Range):
- An elevated result on the Anti-TTG IgG test indicates the presence of IgG antibodies against tissue transglutaminase.
- This result may be used when there is suspicion of IgA deficiency or when IgA-based tests are inconclusive.
- A positive Anti-TTG IgG result should also lead to further diagnostic evaluation, such as a small intestine biopsy, to confirm celiac disease.
Confirming Celiac Disease Diagnosis:
Confirming a diagnosis of celiac disease typically involves a combination of clinical evaluation, laboratory tests, and, in many cases, a small intestine biopsy. Here are the steps involved in confirming celiac disease:
- Clinical Evaluation:
- Begin with a thorough clinical evaluation by a healthcare provider, such as a gastroenterologist or primary care physician.
- The healthcare provider will review your medical history and discuss your symptoms and family history, as celiac disease tends to run in families.
- Be sure to provide detailed information about any gastrointestinal symptoms, skin conditions, fatigue, or other health issues you have been experiencing.
- Blood Tests:
- Blood tests are often the initial step in diagnosing celiac disease. Two primary blood tests are commonly used:
- Anti-TTG (Anti-tissue Transglutaminase) IgA Test: This measures IgA antibodies against tissue transglutaminase. Elevated levels suggest an autoimmune response.
- Total IgA Test: This test checks for IgA deficiency, which can affect the accuracy of the IgA-based tests. If you have IgA deficiency, other tests like the Anti-TTG IgG test may be used.
- Blood tests are often the initial step in diagnosing celiac disease. Two primary blood tests are commonly used:
- Genetic Testing:
- Genetic testing may be performed to check for the presence of specific genetic markers associated with celiac disease, particularly the HLA-DQ2 and HLA-DQ8 genes.
- However, having these genes does not necessarily mean you have celiac disease; it indicates a genetic predisposition.
- Small Intestine Biopsy:
- A small intestine biopsy is often considered the gold standard for confirming celiac disease. It involves the removal of a tiny tissue sample from the lining of the small intestine during an endoscopy.
- The biopsy is examined under a microscope to look for characteristic damage to the intestinal villi. This damage is a hallmark of celiac disease.
- A diagnosis of celiac disease is typically confirmed when the biopsy shows villous atrophy or other histopathological changes consistent with the disease.
- Response to a Gluten-Free Diet:
- In some cases, a positive response to a gluten-free diet may be considered supportive evidence of celiac disease. If your symptoms improve or resolve after adhering to a strict gluten-free diet, this suggests a diagnosis of celiac disease.
- However, a gluten-free diet should not be initiated before blood tests and biopsy, as this can affect test results.
- Additional Testing:
- In certain situations, additional tests may be conducted to assess complications or related conditions, such as osteoporosis, nutritional deficiencies, or skin disorders.
- Consultation with a Specialist:
- A gastroenterologist or a specialist in celiac disease is often involved in the diagnosis and management of celiac disease.
- They can help coordinate and interpret the various tests and guide you through the diagnostic process.
FAQs:
What is the Anti-TTG antibodies test?
The Anti-TTG antibodies test is a blood test used to detect the presence and quantity of antibodies against tissue transglutaminase. It is primarily used in the diagnosis of celiac disease.
Why is the Anti-TTG antibodies test performed?
The test is performed to aid in the diagnosis of celiac disease by identifying an autoimmune response to gluten ingestion.
What is the significance of Anti-TTG antibodies in celiac disease diagnosis?
Elevated Anti-TTG antibody levels in the blood indicate an autoimmune response to tissue transglutaminase, which is associated with the characteristic damage to the small intestine in celiac disease.
How is the test performed?
A blood sample is typically collected from a vein in the arm. The sample is then sent to a laboratory for analysis.
What are the normal reference values for the Anti-TTG antibodies test?
Normal values can vary between laboratories but are often less than 4 U/mL or IU/mL for the Anti-TTG IgA test and less than 6 U/mL or IU/mL for the Anti-TTG IgG test.
What does a positive Anti-TTG antibodies test result mean?
A positive result suggests an elevated level of Anti-TTG antibodies in the blood, which is indicative of a higher likelihood of celiac disease.
Are there other conditions that can cause positive Anti-TTG antibody results?
While celiac disease is the primary condition associated with positive Anti-TTG antibody results, certain other autoimmune and gastrointestinal disorders can also cause elevated levels.
What should I do if I have a positive Anti-TTG antibodies test result?
A positive result should lead to further diagnostic evaluation, including genetic testing and a small intestine biopsy, to confirm the presence of celiac disease.
Can Anti-TTG antibodies tests yield false-positive or false-negative results?
While these tests are highly specific, factors such as IgA deficiency or recent gluten consumption can affect results. False negatives can occur, especially in individuals with IgA deficiency.
Is it necessary to follow a gluten-containing diet before the test?
To increase the accuracy of the test, it is typically recommended to be on a gluten-containing diet for a period before testing. Consult your healthcare provider for specific guidelines.
Is the Anti-TTG antibodies test the only diagnostic test for celiac disease?
No, celiac disease diagnosis usually involves a combination of clinical evaluation, antibody testing (including Anti-TTG), genetic testing, and, in many cases, a small intestine biopsy for confirmation.
Conclusion:
In conclusion, the Anti-TTG (Anti-tissue Transglutaminase) antibodies test is a vital tool in the diagnosis of celiac disease, aiding in the identification of an autoimmune response to gluten ingestion. Elevated levels of these antibodies in the blood serve as a key indicator of the disease, prompting further diagnostic steps. However, a comprehensive diagnosis of celiac disease often involves a combination of clinical evaluation, genetic testing, and small intestine biopsy to confirm the presence of the condition and guide appropriate management, primarily a lifelong gluten-free diet.
Possible References Used