ECLIA stands for “Electrochemiluminescence immunoassay.” It is a type of immunoassay used in medical laboratories to measure the concentration of various substances in a patient’s blood. ECLIA is commonly employed to detect and quantify hormones, proteins, drugs, and other analytes that are important for diagnosing and monitoring various diseases and conditions.

What is ECLIA?
ECLIA stands for “Electrochemiluminescence immunoassay.” It is a sensitive laboratory technique used to detect and quantify substances in the blood or body fluids, widely employed in medical diagnostics.
Principles of ECLIA:
The principles of ECLIA (Electrochemiluminescence immunoassay) are based on the following key steps:
- Antibody-Antigen Binding: Specific antibodies are used to selectively bind to the target analyte (antigen) of interest present in the patient’s sample. The antibodies are designed to recognize and bind only to the specific analyte they are meant to detect.
- Luminescent Labeling: One of the antibodies used in the assay is labeled with a luminescent marker. This labeling allows for the indirect measurement of the bound analyte through the detection of light emission.
- Formation of Antibody-Analyte Complex: When the patient’s sample is introduced to the system, the specific antibodies bind to the target analyte, forming a complex.
- Electrochemical Stimulation: The ECLIA instrument applies an electrical current to the system, inducing a chemical reaction between the labeled antibody and a special “labeling reagent” present in the system.
- Light Emission: The chemical reaction results in the emission of light (luminescence) from the labeled antibody. The intensity of the emitted light is directly proportional to the amount of analyte present in the sample.
- Quantification: The instrument measures the intensity of the emitted light and correlates it with the concentration of the analyte in the patient’s sample. This provides a quantitative result, allowing accurate determination of the analyte’s concentration.
Advantages of ECLIA:
ECLIA (Electrochemiluminescence immunoassay) offers several advantages, making it a preferred method in clinical laboratories for detecting and quantifying various analytes. Some of the key advantages of ECLIA include:
- High Sensitivity: ECLIA is highly sensitive, capable of detecting analytes at very low concentrations in the patient’s sample. This sensitivity allows for the early detection of diseases and conditions, even when analyte levels are low.
- Wide Dynamic Range: ECLIA has a broad dynamic range, meaning it can accurately measure both low and high concentrations of analytes in the same sample. This flexibility is essential for detecting a wide range of medical conditions and monitoring treatment responses.
- Precision and Accuracy: ECLIA provides precise and accurate quantitative results, reducing the potential for errors and ensuring reliable diagnostic information for healthcare professionals.
- Low Interference: The method is less susceptible to interference from other substances present in the patient’s sample, minimizing false-positive or false-negative results and enhancing the assay’s specificity.
- Fast Results: ECLIA offers rapid assay times, allowing for quick turnaround of test results. This speed is beneficial for urgent or time-sensitive diagnostic needs.
- Automation and Throughput: ECLIA can be easily automated, enabling high-throughput testing in clinical laboratories. The automated process reduces manual labor, increases efficiency, and allows for the analysis of a large number of samples in a shorter time.
- Minimal Sample Volume: ECLIA requires a small amount of patient sample, reducing the volume of blood or body fluid needed for testing. This is particularly advantageous for pediatric and elderly patients who may have limited blood volume tolerance.
- Versatility: ECLIA can be used to measure a wide range of analytes, including hormones, proteins, drugs, tumor markers, infectious agents, and more. Its versatility makes it suitable for various diagnostic applications.
- Long Shelf Life of Reagents: The reagents used in ECLIA typically have a long shelf life, providing stability and cost-effectiveness for laboratories.
- Standardization: ECLIA methods are often standardized across different instruments and laboratories, ensuring consistent and comparable results between different testing facilities.
Disadvantages of ECLIA:
- Cost: ECLIA instrumentation and reagents can be relatively expensive compared to other immunoassay methods. The initial setup cost and ongoing maintenance costs may pose challenges for smaller laboratories or healthcare facilities with limited resources.
- Complexity: ECLIA requires specialized equipment and trained personnel to operate and maintain the instrumentation properly. The complexity of the technology may limit its accessibility in certain settings.
- Technical Expertise: ECLIA requires skilled technicians or laboratory professionals who are familiar with the method’s principles and instrumentation. The need for trained personnel may restrict its availability in remote or underserved areas.
- Sample Interference: Although ECLIA is less prone to interference than some other immunoassay methods, certain substances or matrix effects in the patient’s sample can still affect the accuracy and specificity of the assay.
- Cross-Reactivity: Like any immunoassay, ECLIA may exhibit cross-reactivity with related substances, leading to false-positive or false-negative results. Manufacturers work to minimize cross-reactivity, but it can still occur in some cases.
- Limited Customization: ECLIA tests are often commercially available as pre-packaged kits, which may limit the ability to customize assays for specific research or clinical needs.
- Turnaround Time: While ECLIA generally offers rapid results compared to traditional methods, it may still take some time to complete the analysis, especially when a high number of samples need to be processed.
- Limited Analyte Stability: Some analytes may have limited stability in the patient’s sample, which could affect the accuracy of results if testing is not performed promptly after sample collection.
- Matrix Effects: Certain complex sample matrices may influence the assay performance, affecting the accuracy and precision of results.
- Limited Point-of-Care Application: The specialized equipment and technical requirements of ECLIA limit its feasibility for point-of-care testing, which requires simpler, more portable methods.
Applications in Medical Diagnostics:
ECLIA (Electrochemiluminescence immunoassay) has a wide range of applications in medical diagnostics. It is a valuable tool used to detect and quantify various analytes in patient samples, aiding in the diagnosis, monitoring, and management of numerous diseases and conditions. Some of the key applications of ECLIA in medical diagnostics include:
- Endocrinology: ECLIA is commonly used to measure hormones such as thyroid hormones (T3, T4, TSH), reproductive hormones (e.g., testosterone, estradiol, progesterone), and other endocrine markers. These tests help diagnose hormonal imbalances and disorders like hypothyroidism, hyperthyroidism, and reproductive disorders.
- Oncology: ECLIA plays a crucial role in detecting tumor markers associated with specific cancers. It is used for monitoring cancer progression, assessing treatment responses, and detecting cancer recurrence. Common tumor markers measured using ECLIA include PSA (Prostate-Specific Antigen), CA 125 (Cancer Antigen 125), and AFP (Alpha-Fetoprotein).
- Cardiology: ECLIA is utilized to measure cardiac biomarkers like troponin, creatine kinase (CK), and brain natriuretic peptide (BNP) to diagnose and assess the severity of heart attacks, heart failure, and other cardiac conditions.
- Infectious Diseases: ECLIA is employed in the detection of infectious agents, including viruses (e.g., HIV, hepatitis B and C), bacteria (e.g., H. pylori), and parasites (e.g., Toxoplasma gondii). Rapid and accurate diagnosis of infectious diseases is vital for appropriate treatment and infection control.
- Autoimmune Diseases: ECLIA is used to measure autoantibodies associated with various autoimmune disorders like rheumatoid arthritis, systemic lupus erythematosus (SLE), and autoimmune thyroid diseases.
- Allergy Testing: ECLIA is applied to assess specific IgE antibodies in allergic reactions, aiding in the diagnosis and management of allergies.
- Therapeutic Drug Monitoring (TDM): ECLIA is used to measure drug concentrations in the blood to optimize drug dosages and ensure therapeutic efficacy while avoiding toxic levels.
- Prenatal Screening: ECLIA is utilized in prenatal care to measure markers like human chorionic gonadotropin (hCG) and alpha-fetoprotein (AFP) to screen for fetal abnormalities and genetic disorders.
- Bone Metabolism: ECLIA can measure markers like vitamin D, parathyroid hormone (PTH), and bone-specific alkaline phosphatase (BAP) to assess bone health and diagnose conditions like osteoporosis.
- Immunology: ECLIA is used to measure various immunological markers, including cytokines, chemokines, and immune cells, providing insights into immune responses and immune-related disorders.
Common Uses of ECLIA:
ECLIA (Electrochemiluminescence immunoassay) is a widely used laboratory technique with various applications across different areas of medical diagnostics and research. Some of the common uses of ECLIA include:
- Hormone Testing: ECLIA is commonly employed to measure hormone levels in the blood. This includes thyroid hormones (T3, T4, TSH), reproductive hormones (e.g., testosterone, estrogen, progesterone), and other hormones related to the endocrine system. Hormone testing helps diagnose hormonal imbalances and various endocrine disorders.
- Tumor Marker Analysis: ECLIA is used to detect and quantify specific tumor markers associated with various cancers. Common tumor markers measured using ECLIA include PSA (Prostate-Specific Antigen) for prostate cancer, CA 125 (Cancer Antigen 125) for ovarian cancer, and CEA (Carcinoembryonic Antigen) for colorectal cancer.
- Cardiac Biomarker Testing: ECLIA plays a vital role in measuring cardiac biomarkers like troponin, CK-MB (Creatine Kinase-MB), and BNP (Brain Natriuretic Peptide) for the diagnosis and assessment of heart attacks, heart failure, and other cardiovascular conditions.
- Infectious Disease Testing: ECLIA is utilized to detect and quantify antibodies or antigens related to infectious agents such as HIV, hepatitis viruses, syphilis, and other pathogens. It is a valuable tool in diagnosing and monitoring infectious diseases.
- Autoimmune Disease Diagnosis: ECLIA is used to measure autoantibodies associated with autoimmune disorders such as rheumatoid arthritis, systemic lupus erythematosus (SLE), and autoimmune thyroid diseases.
- Therapeutic Drug Monitoring (TDM): ECLIA is applied to measure drug concentrations in the blood, ensuring appropriate drug dosages for therapeutic efficacy and avoiding potential toxicity.
- Allergy Testing: ECLIA is used to measure specific IgE antibodies in allergic reactions, aiding in the diagnosis and management of allergies.
- Prenatal Screening: ECLIA is employed in prenatal care to measure markers such as hCG (human chorionic gonadotropin) and AFP (alpha-fetoprotein) for screening fetal abnormalities and genetic disorders.
- Bone Health Assessment: ECLIA can measure markers related to bone metabolism, such as vitamin D, PTH (parathyroid hormone), and BAP (bone-specific alkaline phosphatase), to assess bone health and diagnose conditions like osteoporosis.
- Immunological Research: ECLIA is widely used in immunology research to quantify cytokines, chemokines, and other immune system-related molecules to study immune responses and immunological disorders.
Components of ECLIA:
The Electrochemiluminescence immunoassay (ECLIA) involves several essential components that work together to detect and quantify analytes in a patient’s sample. The key components of ECLIA include:
- Solid Phase: ECLIA utilizes a solid phase, typically in the form of microtiter plates or beads coated with specific capture antibodies. These antibodies are designed to bind to the target analyte of interest.
- Detection Antibody: A detection antibody is used in ECLIA, which is specific to the analyte being measured. This detection antibody is labeled with a luminescent marker, such as ruthenium or iridium complexes.
- Patient Sample: The patient’s blood, serum, plasma, or other body fluid containing the analyte of interest is collected and used as the sample for analysis.
- Calibration Standards: A set of calibration standards with known concentrations of the analyte is prepared. These standards are used to create a calibration curve, which allows for the quantification of the analyte in the patient’s sample.
- Control Samples: Control samples with known analyte concentrations (low, medium, and high) are included in the assay to ensure the accuracy and reliability of the test results.
- Labeling Reagent: A special labeling reagent is used in the ECLIA system, which reacts with the luminescent marker on the detection antibody to generate the chemiluminescent signal.
- Detection System: ECLIA instruments have a detection system to measure the emitted light (chemiluminescence) from the labeled detection antibody. The intensity of the emitted light is directly proportional to the amount of analyte present in the sample.
- Reaction Vessels: The ECLIA system contains reaction vessels, such as microtiter plates or tubes, where the interactions between the antibodies and the analyte take place.
- Wash Buffer: A wash buffer is used to remove any unbound components and reduce background noise in the assay, ensuring a clean signal during detection.
- Incubation Module: The assay typically involves incubation steps, where the patient’s sample, detection antibody, and other components come into contact and allow for the formation of the antibody-analyte complex.
- Data Analysis Software: ECLIA instruments are equipped with data analysis software to interpret the chemiluminescence signals, convert them into analyte concentrations using the calibration curve, and display the final results.
ECLIA Procedure:
The Electrochemiluminescence immunoassay (ECLIA) procedure involves several steps that facilitate the detection and quantification of specific analytes in a patient’s sample. Here’s a general outline of the ECLIA procedure:
- Sample Collection: A blood sample, serum, plasma, or other body fluid containing the analyte of interest is collected from the patient.
- Sample Preparation: The collected sample may undergo initial processing steps, such as centrifugation, to separate the liquid portion (serum or plasma) from the cellular components.
- Incubation: The prepared patient sample is added to microtiter plates or tubes that contain solid-phase capture antibodies specific to the target analyte. These antibodies immobilize the analyte, facilitating its detection.
- Addition of Detection Antibody: A detection antibody labeled with a luminescent marker, such as ruthenium or iridium complexes, is added to the reaction vessel. This detection antibody specifically binds to the captured analyte, forming an antibody-analyte complex.
- Formation of Antibody-Analyte Complex: During the incubation period, the detection antibody binds to the analyte on the solid phase, creating a sandwich complex with the capture antibody. This complex captures the analyte, ensuring specificity in the assay.
- Wash Step: After the incubation period, unbound components are removed from the reaction vessel through a wash step. This wash step helps eliminate any non-specific binding, reducing background noise and increasing assay sensitivity.
- Addition of Labeling Reagent: A special labeling reagent is added to the reaction vessel. This reagent reacts with the luminescent marker on the detection antibody, triggering an electrochemical reaction.
- Electrochemical Stimulation: The ECLIA instrument applies an electrical current to induce the electrochemical reaction between the labeling reagent and the luminescent marker. This reaction generates light (chemiluminescence).
- Chemiluminescence Detection: The emitted light (chemiluminescence) is detected and measured by the ECLIA instrument’s detection system. The intensity of the emitted light is directly proportional to the amount of analyte present in the patient’s sample.
- Calibration and Quantification: The ECLIA instrument uses a set of calibration standards with known concentrations of the analyte to create a calibration curve. The measured chemiluminescence signals from the patient sample are then compared to the calibration curve to quantify the analyte’s concentration.
- Data Analysis and Reporting: The ECLIA instrument’s data analysis software interprets the signals, converts them into analyte concentrations, and displays the final results, which can be reported to the healthcare provider for clinical interpretation.
Interpreting ECLIA Results:
Interpreting ECLIA (Electrochemiluminescence immunoassay) results involves understanding the quantitative values obtained from the chemiluminescence signals generated during the assay. Here are the key steps in interpreting ECLIA results:
- Reference Range or Cut-off Value: The first step in interpreting ECLIA results is to compare the obtained value with the established reference range or cut-off value. The reference range represents the normal or expected range of values for a particular analyte in a healthy population. The cut-off value is used to distinguish between normal and abnormal results. If the ECLIA result falls within the reference range or below the cut-off value, it is considered normal or negative, respectively. If the result exceeds the reference range or the cut-off value, it is considered abnormal or positive.
- Units of Measurement: Pay attention to the units of measurement used in the ECLIA report. Some analytes may be reported in different units based on the specific instrument or laboratory’s protocols. Understanding the units is crucial for proper interpretation and comparison with standard values.
- Clinical Context: Interpreting ECLIA results should always be done in the context of the patient’s clinical history, symptoms, and other diagnostic findings. A single abnormal result may not be conclusive, and further investigation or follow-up testing may be necessary to confirm a diagnosis or assess the clinical significance of the result.
- Trend Analysis: For patients undergoing treatment or monitoring for a specific condition, tracking the trend of ECLIA results over time is essential. A trend of increasing or decreasing values can provide valuable information about the patient’s response to treatment or disease progression.
- Confirmatory Testing: In some cases, confirmatory testing may be required to validate the ECLIA results, especially if the result is unexpected or at the borderline of the reference range or cut-off value. Additional tests can help confirm or rule out the presence of specific conditions.
- Quality Control: ECLIA results should be evaluated in the context of quality control measures. Quality control samples with known analyte concentrations are included in each batch of testing to ensure the accuracy and reliability of the assay.
- Interpretation Guidelines: Interpretation guidelines provided by the assay’s manufacturer or established medical guidelines can aid in understanding the clinical significance of the ECLIA results.
Factors Affecting ECLIA Results:
Several factors can affect the results of ECLIA (Electrochemiluminescence immunoassay), potentially leading to inaccurate or unreliable measurements. It is essential for laboratory professionals and healthcare providers to be aware of these factors to ensure the accuracy and validity of the test results. Some of the key factors that can influence ECLIA results include:
- Sample Quality: The quality of the patient’s sample, such as blood, serum, or plasma, is critical. Hemolysis (rupturing of red blood cells), lipemia (excess fat in the blood), or icterus (presence of bilirubin) can interfere with the assay and affect the accuracy of the results.
- Matrix Effects: The presence of complex sample matrices or interfering substances can impact the specificity of the ECLIA assay. Matrix effects can cause false-positive or false-negative results by interfering with the binding of antibodies to the target analyte.
- Sample Contamination: Contamination of the sample with foreign substances or other analytes may lead to cross-reactivity and interference, affecting the accuracy of the assay.
- Calibration: Proper calibration of the ECLIA instrument is essential for accurate quantification of analytes. Calibration standards with known concentrations must be used to generate a calibration curve that converts the detected signals into analyte concentrations.
- Instrument Performance: The performance and maintenance of the ECLIA instrument, including the detection system and electrode, can impact the sensitivity and precision of the assay. Regular maintenance and calibration checks are necessary to ensure accurate results.
- Reaction Time and Temperature: The timing and temperature during the assay steps, such as incubation and chemiluminescence detection, must be controlled consistently. Deviations from the recommended parameters can affect the kinetics of the reaction and compromise the assay’s accuracy.
- Reagent Quality: The quality and stability of reagents, including the capture and detection antibodies, labeling reagent, and wash buffer, can influence the assay’s performance. Expired or degraded reagents may lead to unreliable results.
- Interference from Endogenous Substances: Some substances naturally present in the patient’s sample can interfere with the assay, leading to false results. For example, heterophilic antibodies and rheumatoid factors can cause interference in immunoassays, including ECLIA.
- Lot-to-Lot Variation: Reagents from different batches or lots may have variations in performance, leading to differences in assay results. Proper quality control measures and validation are necessary when using new reagent lots.
- Operator Technique: Skilled and well-trained laboratory personnel are crucial for performing ECLIA accurately. Variability in operator technique can impact the reproducibility and reliability of the results.
Limitations and Considerations:
ECLIA (Electrochemiluminescence immunoassay) is a powerful diagnostic technique, but it does have some limitations and considerations that should be taken into account when using this method:
- Specificity: While ECLIA is generally highly specific due to the use of specific antibodies, cross-reactivity with related substances can occur. This can lead to false-positive or false-negative results in certain situations.
- Matrix Effects: Interference from the sample matrix, especially in complex samples like blood or serum, can affect assay performance. Hemolysis, lipemia, or icterus can interfere with the accuracy of the results.
- Hemolyzed Samples: Hemolysis (rupturing of red blood cells) can release intracellular components that may interfere with the assay and affect the accuracy of the results. Hemolyzed samples should be avoided or flagged for appropriate interpretation.
- Sample Stability: Some analytes may be unstable in the patient’s sample, leading to potential changes in concentration over time. Samples should be processed promptly, and storage conditions should be carefully considered to minimize degradation.
- Reference Ranges: Reference ranges may vary between different laboratories and patient populations. It is essential to use appropriate reference ranges for specific patient demographics and conditions.
- Calibration: Accurate calibration of the ECLIA instrument is crucial for reliable results. Proper calibration using known concentrations of the analyte is necessary to generate a calibration curve for quantification.
- Quality Control: Regular quality control measures are essential to monitor the performance of the assay and detect any drift or variations in results. Quality control samples with known analyte concentrations are included in each batch of testing.
- Operator Skill: Proper training and proficiency of laboratory personnel are critical for accurate and consistent ECLIA results. Operator skill can influence the precision and reliability of the assay.
- Interference from Heterophilic Antibodies: Heterophilic antibodies present in some patient samples can cause interference in immunoassays, including ECLIA. Special blocking reagents or sample pretreatment may be needed to minimize this effect.
- High-Dose Hook Effect: In certain cases, very high concentrations of the analyte can lead to the “hook effect,” where the signal decreases instead of increasing. Dilution of the sample may be necessary to obtain accurate results.
- Cost and Equipment: ECLIA requires specialized equipment and reagents, which can be relatively expensive. The initial setup cost and ongoing maintenance should be considered when implementing ECLIA in a laboratory.
ECLIA vs. Other Immunoassay Methods:
| Feature | ECLIA | ELISA (Enzyme-Linked Immunosorbent Assay) | CLIA (Chemiluminescent Immunoassay) |
|---|---|---|---|
| Detection Method | Electrochemiluminescence | Enzyme-Color Reaction | Chemiluminescence |
| Signal Detection | Electrical current induces | Color change due to enzyme-substrate reaction | Chemical reaction produces light emission |
| Sensitivity | High | Moderate to High | Moderate to High |
| Dynamic Range | Wide | Limited | Wide |
| Cross-Reactivity | Low | Possible cross-reactivity with related substances | Low |
| Sample Interference | Low | Possible interference from sample components | Low |
| Automation | Fully automated | Can be automated, but manual steps may be required | Fully automated |
| Throughput | High | Moderate to High | High |
| Cost | Relatively higher | Moderate | Relatively higher |
| Sample Volume | Requires small sample volume | May require larger sample volume | Requires small sample volume |
| Time to Results | Rapid | Generally longer incubation and detection times | Rapid |
| Point-of-Care Testing | Less suitable for POC testing | Some ELISAs adapted for POC testing | Less suitable for POC testing |
| Common Applications | Medical diagnostics and research | Medical diagnostics, research, and screening | Medical diagnostics and research |
Future Trends in ECLIA Technology:
As with many areas of medical technology, ECLIA (Electrochemiluminescence immunoassay) is expected to continue evolving and improving in the future. Several potential trends and advancements can be anticipated in ECLIA technology:
- Enhanced Sensitivity and Detection Limits: Ongoing research and development may lead to improvements in the sensitivity of ECLIA, allowing for the detection of even lower concentrations of analytes in patient samples. This heightened sensitivity can be crucial in early disease detection and monitoring.
- Multiplex Assays: Future ECLIA platforms may enable the simultaneous measurement of multiple analytes in a single sample. Multiplex assays can improve efficiency and reduce the sample volume needed, making diagnostic testing faster and more cost-effective.
- Miniaturization and Point-of-Care Testing: Efforts to miniaturize ECLIA systems and make them more portable can open doors for point-of-care testing. Portable ECLIA devices may be used in remote or resource-limited settings, allowing for rapid and on-the-spot diagnostic decisions.
- High-Throughput Automation: Automation in ECLIA technology is expected to advance further, enabling laboratories to process large numbers of samples efficiently. Automated systems can reduce manual labor, minimize human errors, and increase overall laboratory throughput.
- Integration with Other Technologies: ECLIA may be integrated with other diagnostic technologies, such as molecular testing or imaging modalities. Combining different diagnostic methods can provide a more comprehensive picture of a patient’s health status.
- Personalized Medicine: Future ECLIA assays may play a vital role in personalized medicine, tailoring treatment plans based on individual patient characteristics and biomarker profiles. ECLIA technology can help identify patients who are likely to respond to specific treatments or therapies.
- High-Resolution Analysis: Advancements in detection systems and data analysis may allow for high-resolution analysis of analytes, providing detailed insights into disease processes and treatment responses.
- Digital Health and Connectivity: ECLIA instruments could become part of digital health ecosystems, integrating with electronic health records (EHRs) and enabling remote monitoring and real-time data sharing between healthcare providers and patients.
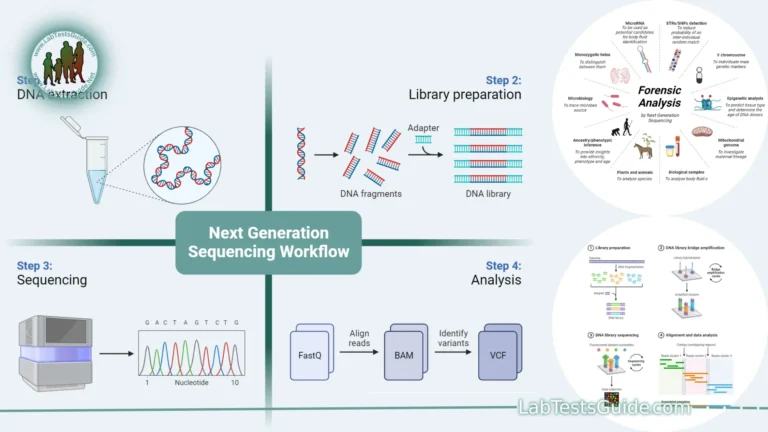
- Integration with Next-Generation Sequencing (NGS): ECLIA could be combined with NGS technologies, allowing for a comprehensive assessment of genetic and protein-level information to enhance disease diagnosis and treatment.
- Novel Biomarkers: Ongoing research may lead to the discovery of new biomarkers, and ECLIA technology can be adapted to measure these biomarkers accurately, contributing to improved diagnostic capabilities.
FAQs:
What is ECLIA?
ECLIA stands for “Electrochemiluminescence immunoassay.” It is a highly sensitive laboratory technique used to detect and quantify substances in the blood or body fluids, widely employed in medical diagnostics.
How does ECLIA work?
ECLIA involves the use of specific antibodies that selectively bind to the target analyte in the patient’s sample. A detection antibody labeled with a luminescent marker is then introduced. When an electrical current is applied, the labeled antibody undergoes an electrochemical reaction, emitting light (chemiluminescence) that is proportional to the analyte’s concentration.
What are the advantages of ECLIA over other immunoassay methods?
ECLIA offers advantages such as high sensitivity, wide dynamic range, low interference, fast results, minimal sample volume, and high automation and throughput capabilities. These features make it a preferred method in clinical diagnostics.
What are the limitations of ECLIA?
ECLIA limitations include potential cross-reactivity, sample interference from certain matrices, and the need for skilled operators and specialized equipment. Hemolysis or other sample issues may also impact results.
What analytes can be measured using ECLIA?
ECLIA can measure a wide range of analytes, including hormones, tumor markers, cardiac biomarkers, infectious agents, autoimmune markers, drugs, and more. Its versatility allows for various diagnostic applications.
Is ECLIA suitable for point-of-care testing (POCT)? ECLIA is less suitable for POCT due to its requirement for specialized equipment and infrastructure. Other rapid immunoassay methods may be more appropriate for point-of-care applications.
How are ECLIA results interpreted?
ECLIA results are interpreted by comparing the obtained value with established reference ranges or cut-off values. The clinical context, patient history, and other diagnostic findings are also considered for accurate interpretation.
What are the future trends in ECLIA technology?
Future trends in ECLIA technology include enhanced sensitivity, multiplex assays, miniaturization for POCT, high-throughput automation, integration with other diagnostic methods, and personalized medicine applications.
What role does ECLIA play in medical diagnostics?
ECLIA plays a crucial role in medical diagnostics by providing accurate and precise measurements of various analytes in patient samples. It aids in the early detection, diagnosis, monitoring, and management of numerous diseases and conditions, contributing to improved patient care.
Conclusion:
In conclusion, ECLIA (Electrochemiluminescence immunoassay) is a highly sensitive and versatile laboratory technique used in medical diagnostics. It offers numerous advantages, including high sensitivity, wide dynamic range, and fast results. While ECLIA has some limitations, ongoing advancements in technology and research are expected to further enhance its capabilities. ECLIA plays a crucial role in detecting and quantifying various analytes, contributing to improved patient care and personalized medicine in the future.
Possible References Used